How has the pandemic affected rates of five common surgeries and diagnostic procedures?

The COVID-19 pandemic has proven very disruptive on many levels. This includes affecting the way patients access healthcare and the degree to which they have had various procedures. We look at the impact on five high volume elective procedures (some surgeries and some diagnostic) and find fascinating trends across our 2019 to 2022 study period.
Authors
Discovery Health's Shirley Collie (Chief Analytics Actuary), Sameera Haneef (Senior Actuary) and Karl Bernhardt (Actuarial Analyst)
We set out to investigate:
First, utilisation trends over the course of the pandemic, with a focus on five high volume elective procedures:
- Spinal surgery
- Cataract surgery
- Tonsillectomies and adenoidectomies
- Endoscopies
- Cardiac catheterisations (angiograms)
Second:
- Whether changes in utilisation around cardiac catheterisation had a long-term effect on medical scheme members' health outcomes and wellbeing.
We look at how the rates of the above-mentioned procedures changed from 2019 (pre-COVID baseline) to 2022. Our data set spans procedures claimed for by 3.46 million Discovery Health administered medical scheme members.
Our findings: Utilisation trends
Looking at healthcare procedure utilisation trends over the course of the pandemic, we find varying degrees of sensitivity to the changes brought about by the pandemic and various restrictions put in place to curb the spread of COVID-19.
(a) Spinal and cataract surgeries
Comparing the frequency of various procedures pre-COVID and during the pandemic, we see that procedures like spinal surgery and cataract surgery returned to normal levels relatively quickly - within a few months post the initial level 5 lockdown (which kicked in 26 March 2020 and lasted to 30 April 2020).
- Admissions for spinal surgery reduced by 11% in 2020 and 8% in 2021 (compared to 2019 levels). We also observed a decrease in conservative care over 2020 and 2021, with less utilisation of out-of-hospital physiotherapy, chiropractor, and GP services prior to a surgical spinal admission.
- Admissions for cataract surgery reduced by 20% in 2020 but showed strong recovery in 2021, with a marginal decrease of just 4% in 2021 compared to 2019 (pre-COVID) levels.
The quick recovery to pre-pandemic admission levels in 2022 in these areas is likely a function of both supply and demand. Surgeons carried on operating on previously scheduled patients, and patients with chronic back pain or cataracts were unlikely to delay getting immediate relief through surgery.
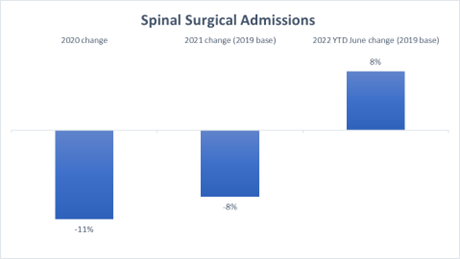
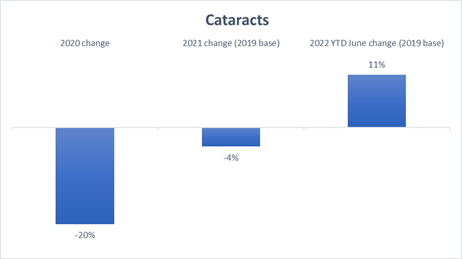
Figures 1 (a) and (b) Admission rates for spinal surgery and cataract surgery. The 0% baseline indicates pre-COVID / 2019 levels.
(b) Tonsillectomies and adenoidectomies
Other procedures showed changes in utilisation that were quite unique to the COVID-19 environment. School closures, mask-wearing, and the use of sanitisers significantly reduced the spread of childhood illnesses and contributed greatly to the 60% reduction in tonsillectomies and adenoidectomies seen through 2020. This trend continued late into 2021 and, as social circumstances have returned to pre-pandemic norms, has recently showed signs of recovery.

Figure 2: Admission rates for tonsillectomies and adenoidectomies in 2020, 2021 and early 2022. The 0% baseline indicates pre-COVID / 2019 levels.
(c) Endoscopies
Diagnostic procedures were also severely impacted over the course of the pandemic. Of course, this raises concerns about the long-term consequences of medical scheme members not getting either diagnoses or medical care they need on time.
For example, the rate of endoscopies (a non-surgical procedure in which doctors look at the digestive tract) was down by 27% in 2020, compared to 2019 levels.
There was a more obvious reduction in the hospital and day clinic setting, compared to endoscopies performed in doctors' rooms. This trend likely reflects people's reluctance to go to healthcare facilities for fear of contracting COVID-19 over the course of the pandemic.
We see that the return to pre-COVID endoscopy levels has been gradual, with admission rates remaining suppressed throughout 2021, and only surpassing pre-COVID levels early in 2022 as some deferred procedures were caught up and new procedures carried out.
- It's likely that most of what we are seeing in 2022 are new procedures. Generally speaking, a portion of the endoscopies that were cancelled at the start of 2020 may no longer be required in 2022, as sometimes patients experience an improvement or resolution of symptoms, or patients may have sought alternative care forms.
- We also looked back at procedures that had been authorised when COVID-19 first reached South African shores and over the ensuing hard lockdown period and saw that only 30% of the endoscopies that were cancelled after they had been authorised back then, were later carried out. So, in 2022 we aren't looking so much at procedures caught up as at new procedures.
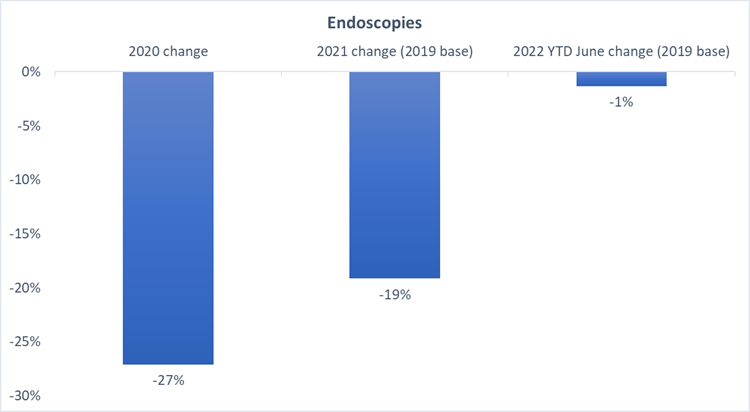
Figure 3: Admission rates for endoscopies in 2020, 2021 and 2022. The 0% baseline indicates pre-COVID / 2019 levels.
(d) Cardiac catheterisations (angiograms)
Looking at claims data for all Discovery Health administered medical schemes, we see a 28% reduction in admissions for cardiac catheterisations over the past two years, once again relative to pre-COVID levels.
Similar trends have been reported on globally. A study by Ullah (2021)[1] reported an almost 50% decrease in cardiac catheterisation procedures early on in the pandemic in tertiary cardiac hospitals in England. These trends raise serious concerns around the long-term worsening of cardiovascular health outcomes for high-risk patients who weren't being diagnosed, accessing care and treatment in time.
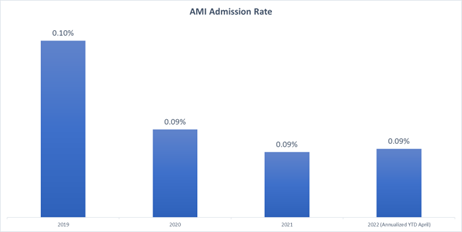
We used the incidence of strokes and acute myocardial infarctions (heart attacks) as a proxy for or sign that people deteriorated because they were not accessing healthcare in time over the past two years.
So, did rates of stroke and heart attack go up? Unexpectedly, they did not.
Looking at outcomes for Discovery Health administered medical scheme members over the pandemic, we see that the rate at which strokes and heart attacks were happening actually reduced by approximately 21% over 2020 and 2021 in comparison to 2019 (pre-COVID) levels.
Why would this be? In light of steady demand from cardiovascular patients, relatively consistent out-of-hospital treatment patterns and the lack of worsening of patient outcomes, the significant reduction in cardiac admissions implies some element of change in supply-side (healthcare provider and facilities) behaviour and protocols in relation to this procedure. We'll carry on monitoring the longer-term impact. However, this a favourable result for our client medical schemes, given the lowered rate of invasive angiograms in comparison to alternative non-invasive diagnostic techniques.
1https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7520383/
- Is it possible that less serious cases were treated in alternative ways, avoiding invasive procedures (like angiograms)? One alternative to the angiogram is Computed Tomography Coronary Angiography (CTCA).
Both are screening tests for coronary artery disease. What are the similarities and what are the differences?
- Both are effective imaging tests in diagnosing conditions relating to the heart and blood vessels.
- Both may use a dye to make blood vessels show up more clearly on images.
- Angiograms are called invasive, as a flexible tube (called a catheter, which needs an incision to be inserted and so is done under local anaesthetic) is threaded through an artery from the groin or arm to the heart or arteries that feed the heart. For people with known coronary artery disease this can also be used to treat the disease in the same session, so treatment (e.g., a stent or artery balloon procedure) can happen right away.
- Angiograms are recommended for patients who have a high risk of coronary artery disease and who have typical symptoms.
- CTCA is a less invasive way of doing an angiogram. Computer tomography scanners looks at the arteries that send blood to the heart (using a combination of x-ray and other technology) to make images of the heart and blood vessels. CTCA is used to diagnose a range of heart conditions and can accurately highlight narrowed or congested blood vessels. It's quick, painless, non-invasive, and doesn't need much preparation or recovery time.
- They are able to rule out coronary artery disease in patients who don't have typical symptoms and who are at low- or medium-risk of disease, and so reduce the need for invasive angiograms for all patients.
- Angiograms typically cost more than CTCAs.
So CTCA is recommended as a first-line diagnostic tool for patients with low- to intermediate- risk of coronary artery disease. Yet, Discovery Health data shows that this tool remains underutilised. There are almost five times as many invasive angiograms performed than CTCAs. So, there is still a preference for angiograms, and it would seem that these are being applied to low-, medium- and high-risk patients.
However, our data show that utilisation of CTCAs increased over the COVID-19 period (a 35% increase in 2021, compared to 2019). And, the latest 2022 year-to-date May data shows just over a doubling of CTCA utilisation rates relative to the corresponding year-to-date period in 2019 (Figure 4a).
(a)Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407-77.
(b)Moss AJ, Williams MC, Newby DE, Nicol ED. The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep 2017;10:15.
(c)Gulati M, Levy PD, Mukherjee D, et al. AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 2021;144:e368-454.
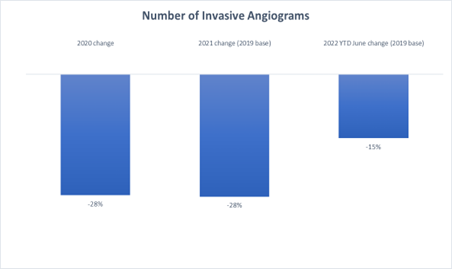
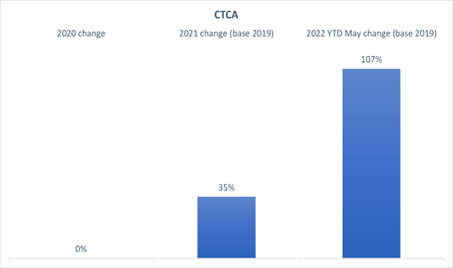
Figures 4 (a) Reduction in admission rates for invasive angiograms from 2019-2020, 2019-2021 and 2019-2022.
Figure 4 (b) Increase in admissions for CTCAs over 2020, 2021 and 2022 (compared to 2019). The 0% baseline indicates pre-COVID / 2019 levels.
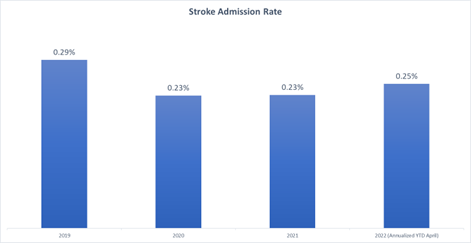
Figures 5 (a) Decrease in admissions to treat strokes over 2020, 2021 and 2022 (compared to 2019).
Figure 5 (b) Decrease in Acute Myocardial Infarction (heart attack) admission rate over 2020, 2021 and 2022 (compared to 2019).
Discussion and conclusion
There's no disputing that the COVID-19 pandemic changed the way patients and healthcare providers approached elective surgeries and diagnostic procedures.
The long-term impact of these disruptions on the health and wellbeing of our medical scheme member population is yet to be fully understood or quantified, and we will carry on monitoring this impact.
For now, we can say that it's encouraging to see screening procedures such as endoscopies returning to pre-COVID levels in 2022, as these are important health-conserving processes. In general, the sooner one catches or treats a medical illness or condition, the better the chances of better treatment outcomes.
It's very interesting that the drop in invasive angiograms over 2020 and 2021 wasn't paralleled by an (expected) increase in strokes or heart attacks. At the same time, we saw more non-invasive CTCAs take place.
This calls into question whether angiograms should be as routine as they are for patients at risk of coronary artery disease or whether patients (low-to medium risk) could be allocated to CTCA screening more often where appropriate.
These dynamics also challenge beliefs about what it means to deliver great quality care to patients and call for a look at alternatives that may make sense, such as CTCAs.
- Ullah A, Fraser DGW, Fath-Ordoubadi F, Holt CM, Malik N. Decrease in cardiac catheterization and MI during COVID pandemic. Am Heart J Plus. 2021 Jan;1:100001. doi: 10.1016/j.ahjo.2020.100001. Epub 2020 Sep 28. PMID: 34173587; PMCID: PMC7520383.
-
- Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407-77.
- Moss AJ, Williams MC, Newby DE, Nicol ED. The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep 2017;10:15.
- Gulati M, Levy PD, Mukherjee D, et al. AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 2021;144:e368-454.
- Discovery Health's Shirley Collie (Chief Analytics Actuary), Sameera Haneef (Senior Actuary) and Karl Bernhardt (Actuarial Analyst)
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
You may want to explore other analyses on our Discovery Health Insights Hub. These include our post, "New study published in British Journal of Sports Medicine: Exercise protects against serious COVID-19 outcomes. This paper outlined the remarkable protection that regular exercise - at moderate or high levels - provides, in lowering the risk of serious COVID-19 illness.
Disclaimer
All information shared on this page is based on perspectives gained from analysis of figures and trends emanating from discovery health's data pool. The analysis, which is conducted by discovery health's actuarial and data scientist team, aims to encourage industry dialogue. This content is shared for educational and informational purposes only. It does not constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions.

Deep dive: Admission rates across South Africa's four COVID-19 waves confirm Omicron-driven fourth wave's lower severity, and more.
07 July 2022
Authors: Chana Suttner (Actuary, Discovery Health),Michael Cohen (Actuarial Analyst, Discovery Health), Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health

Long COVID symptoms, impact on carrying out daily activities: Survey of just over 7,000 medical scheme members reveals key insights
16 June 2022
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health), Lizelle Steenkamp (Senior Healthcare Statistician, Discovery Health), Lebohang Radebe (Data Scientist, Discovery Health), Dr Smybinn Mathews (Clinician, Discovery Health) and Dr Dave Jacobs (Senior Clinician and Clinical Classification System Architect, Discovery Health)

Discovery's COVID-19 personal resilience index predicts an individual's resilience to serious COVID-19 illness
23 May 2022
Authors: Lizelle Steenkamp (Senior Healthcare Statistician at Discovery Health), Tommy Chen (Actuary at Discovery Health), Jared Champion (Senior Actuary at Discovery Health) and Donald Ntjana (Senior Data Scientist at Discovery Health)