Discovery Health's Hospital Care Initiative is the first in South Africa to provide consistent public rankings of private hospital performance

Discovery Health's Hospital Care Initiative provides members with information on the quality of care, patient experience and cost from nearly 150 private hospitals in South Africa so they can choose the best care possible.
Authors
Jared Champion (Senior Actuary, Discovery Health), Chana Suttner (Actuary, Discovery Health), Jackie Duvenage (Actuarial Analyst, Discovery Health), Michael Cohen (Actuary, Discovery Health), Shirley Collie (Chief Health Analytics Actuary, Discovery Health)
The case for consistent public reporting of quality outcomes across the industry
In 2013, South Africa's Competition Commission embarked on the most systematic and comprehensive investigation into the private healthcare sector. After six years, the commission identified numerous gaps in the monitoring, reporting and incentivising of quality healthcare. In particular, the commission argued, healthcare funders needed to more actively incentivise value when purchasing healthcare services.
Although several South African hospital groups have taken the initiative to publicly report on a limited number of quality metrics, such as adverse events, this information remains difficult to compare consistently across the industry.
In the United States, consumers can compare hospital performance via a public database of selected facilities. Public healthcare funder, the Centers for Medicare and Medicaid Services, uses this data to calculate value-based reimbursements. Unlike simple fee-for-service models of reimbursement, value-based programmes reward healthcare providers with incentive payments for the quality of care they provide to patients.
Internationally, data suggests that the public reporting of performance and quality metrics pushes hospitals to take steps to improve quality. When Sweden publicly released its hospital quality index, facility scores improved by 22% from 2007 to 2009 by research published by BCG on Heart Intensive Care Admissions (RIKS-HIA data). The poorest performing hospitals improved their index scores significantly faster than other facilities, ultimately charting a 40% improvement over the same period.
At Discovery Health, we believe we have a societal obligation to drive transparency and quality. Discovery Health administers 17 employer based medical aid schemes and the Discovery Health Medical Scheme, open to all South Africans regardless of employment affiliation.
Using data from members across these schemes, we have developed the Hospital Care Initiative, the first large-scale, public ranking of private hospitals in South Africa based on quality of care, patient satisfaction and cost.
The Hospital Care Initiative enables members to compare hospitals across these measures. It also encourages hospitals to improve care.
We believe that transparency and accountability are key to building a high-quality, efficient healthcare system.
Many factors influence the hospitals we choose. Quality of care should be one of them
If you or someone you love needed hospital care, how would you choose where to go? For most, the choice of hospital is influenced by location, convenience or the availability of specialist care.
But what if you could choose a hospital based on how well it actually offered care?
Why should patients consider cost efficiency when choosing a hospital?
Cost efficiency has a direct impact on medical scheme claims inflation, and consequent premium levels, thus impacting affordability. Hospital cost efficiency is correlated with theatre time and length of stay efficiency both of which are also indicators of healthcare quality.
Methodology: What makes a good hospital?
As part of the Hospital Care Initiative, Discovery Health adapted international reporting standards1 to assess hospitals in four initial categories: death rates, rates of readmission, patient satisfaction and efficiency, (Figure 1).
We used statistical methods to ensure a like-for-like comparison between hospitals through robust risk adjustment. To do this, we controlled for patient demographics, such as age, sex and chronic conditions, that could skew hospital outcomes to be better or worse. Likewise, we accounted for relevant patient clinical history. Finally, we also controlled for admission-related diagnoses and procedures.
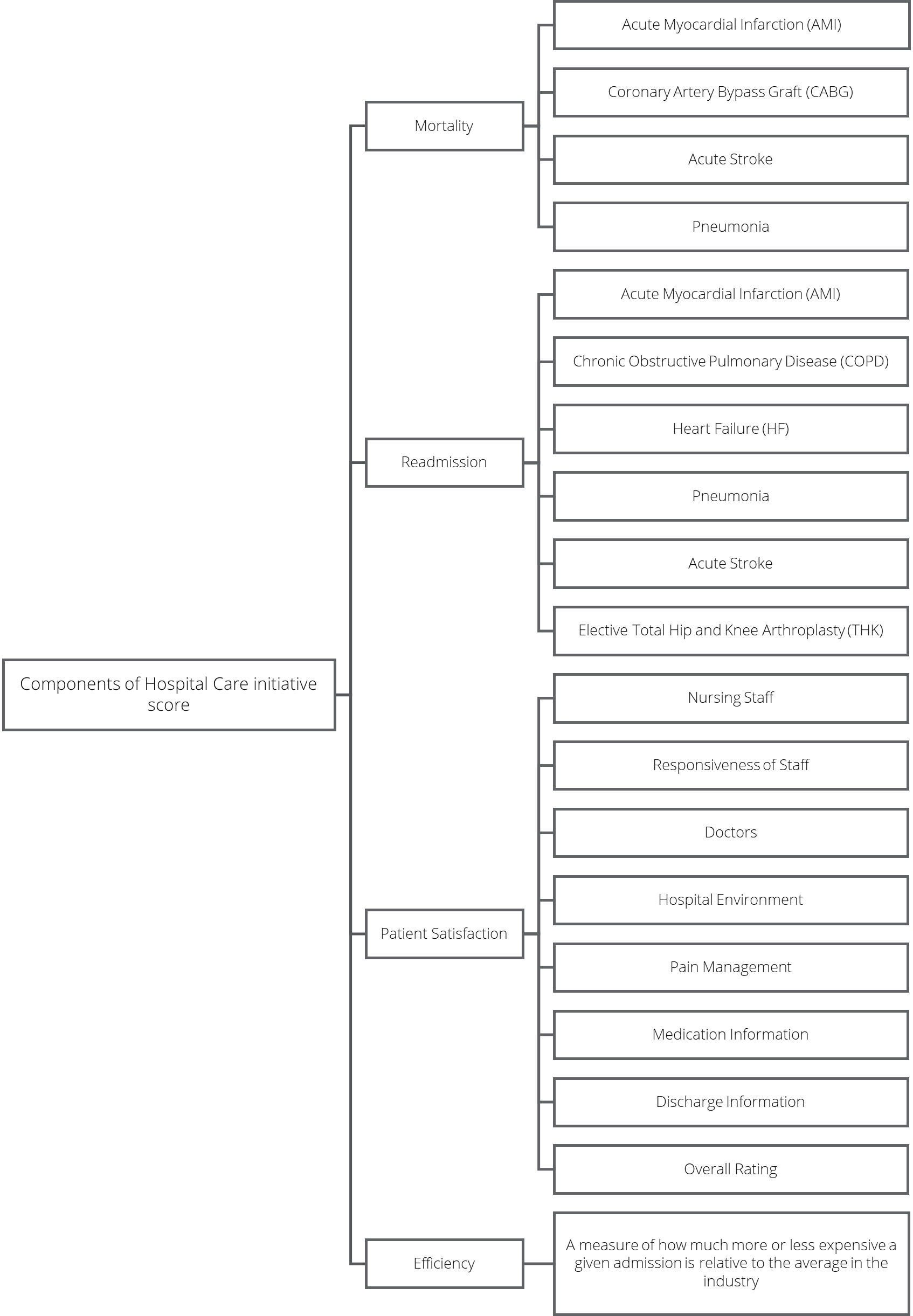
Figure 1: Components included in each of the four categories making up the Hospital Care Initiative score.
Death rates and readmission rates were taken as a proxy for quality of care. Death rates were evaluated for four common conditions:
- Acute myocardial infarction, or heart attacks,
- Acute (sudden) stroke,
- Pneumonia, a serious form of lung infection; and
- Coronary artery bypass graft surgery, a procedure in which blood vessels from another part of the body are removed and attached to the coronary artery to redirect blood around a section of blocked artery.
Deaths were included if they occurred within 30 days of admission and regardless of if they happened in- or out-of-hospital Thirty days post admission was considered an appropriate time frame in which a death could reasonably be attributed to the quality of care received in hospital.Also, as explained in a 2019 study by colleagues and published in the South African Medical Journal, many current hospital interventions are known to decrease the risk of death within 30 days of an admission.
To calculate readmission rates, we looked at unplanned readmissions within 30 days of discharge for six conditions: heart attack, sudden stroke, pneumonia as well as heart failure and elective knee and hip replacements. We also evaluated readmission rates for chronic obstructive pulmonary disease, which includes conditions such as emphysema and chronic bronchitis that make it difficult to breathe.
Facilities had to have a minimum number of cases to be included in the sample to allow for accurate comparison. Moreover, hospitals needed to have death and readmission data for at least two conditions in each category to be evaluated as part of the rankings. For this reason, specialist hospitals focusing on certain conditions were not included.
What patients think matters
Next, patient satisfaction was gauged using member post-discharge survey data on eight categories:
- Nursing staff;
- Doctors;
- Staff responsiveness;
- Pain management;
- How well staff were able to explain medication given to patients;
- Hospital environment;
- The quality of aftercare information provided on discharge; and
- Overall patient experience.
Lastly, hospital efficiency was calculated by comparing the cost of admissions to the industry average, taking into consideration diagnoses and procedures.
Measuring performance and incentivising improvement
After adjusting for possible bias, we converted the rates for each of the four categories - death rates, readmission rates, efficiency and patient experience - into a score from 0 - 10, where 10 represents a perfect score. Scores were determined relative to the upper and lower bounds of rates in the sample - almost like if a professor assigned marks based on a class curve.
We then further adjusted scores, through a process called normalisation, to account for hospital caseloads. This ensured that larger hospitals with more cases and thus more condition-specific categories of deaths or readmissions were not unfairly penalised for this.
Next, scores across the four categories were averaged together alongside an additional mark for "consistency" to create a final composite score for each hospital. Hospitals' consistency scores were determined by their lowest score across the four categories and comprised 10% of a hospital's final mark (Figure 2). The consistency adjustment ensures that hospitals are encouraged to achieve consistently across all categories.
This ensures that those high achieving hospitals are achieving across all measurement categories and are not being driven up the rankings because of a single high performing category, which compensates for poor performance in another category.
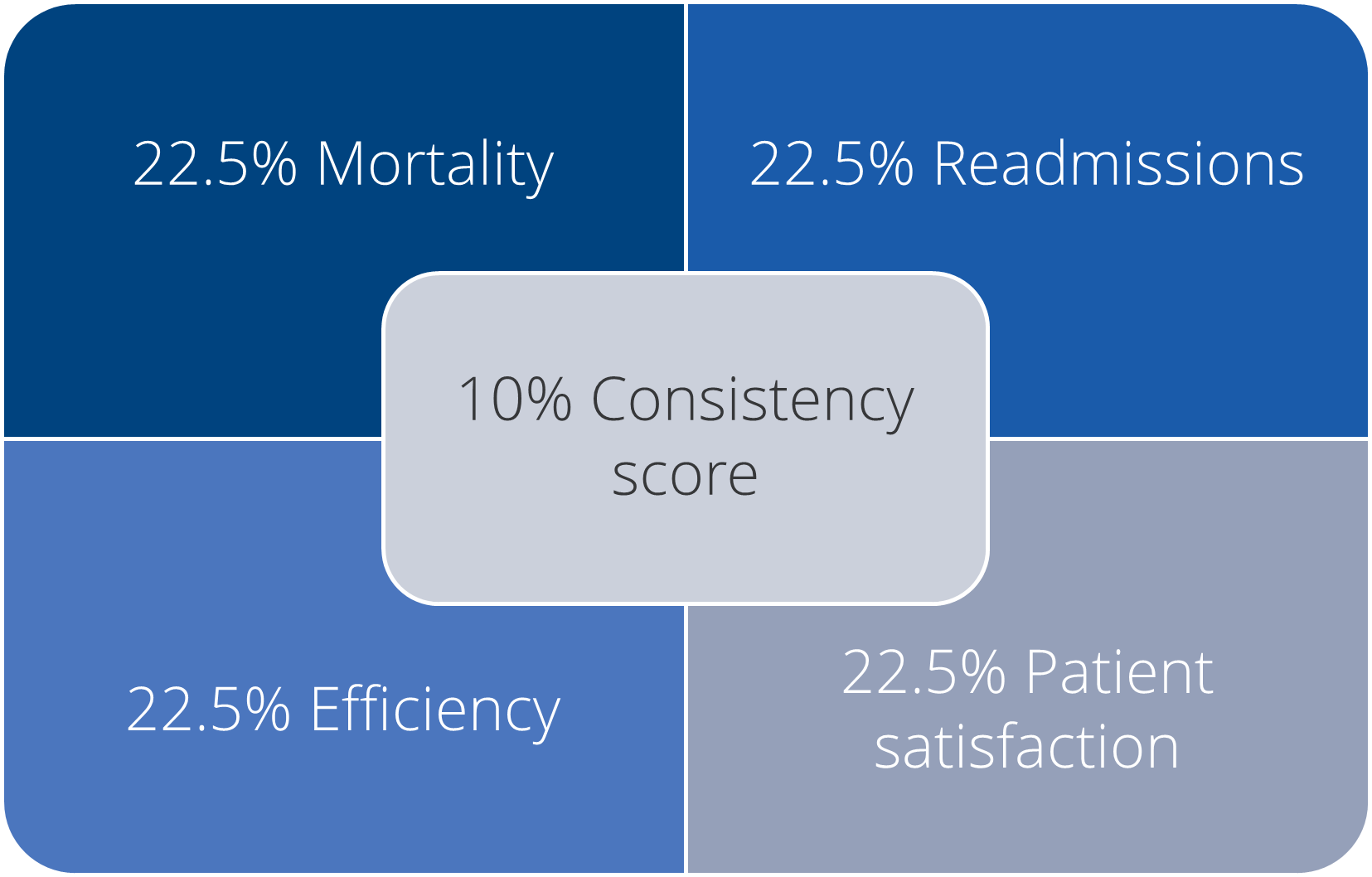
Figure 2: Weighting of each category in the overall score calculation
Finally, normalised category and overall scores were broken up into five different rating bands by their averages in a process called k-means clustering. The cut offs determined through k-means clustering will be the starting point for future years' distributions. Rather than publishing the results in the form of 5 clusters, we grouped them into 3 categories. This was done, in part, to more easily communicate the meaning of scores to the public. (Figure 3)
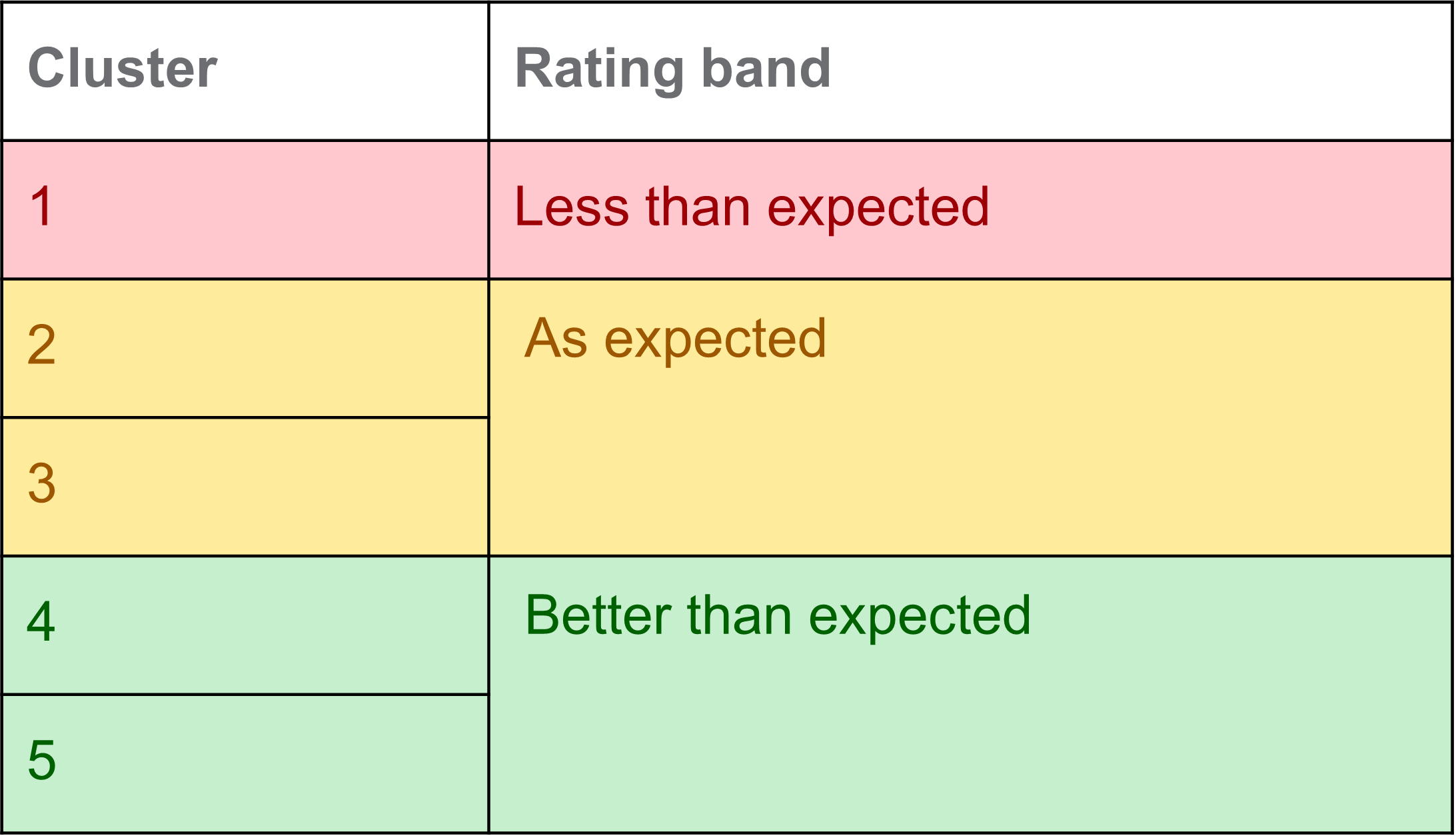
Figure 3: Grouping of clusters into rating bands
So how did South African private hospitals fare?
Ultimately, Discovery's Hospital Care Initiative scored a total of 148 hospitals nationwide. More than a third of hospitals measured are "better than expected" and the majority of hospitals fall into the "as expected" category. About one in 10 (14%) had below-average scores or performed less well than expected. (Figure 4)

Figure 4: Hospital Care Initiative results
Consistency Score
Interestingly, we found that the addition of a consistency metric, weighted as 10% of hospitals' overall score, served its intended purpose. Including consistency, taken as the lowest normalised score across the four categories, meaningfully changed a hospital's overall score enough that we believe it will incentivise facilities to achieve better scores across all categories.
Results nationally
Of the 148 hospitals measured, the overwhelming majority were located in Gauteng, KwaZulu-Natal and the Western Cape. (Figure 5). It is encouraging to see that nationally there is a wide coverage of hospitals in the "better than expected" category and there is no single province with the majority of hospitals falling into the "less than expected" category.
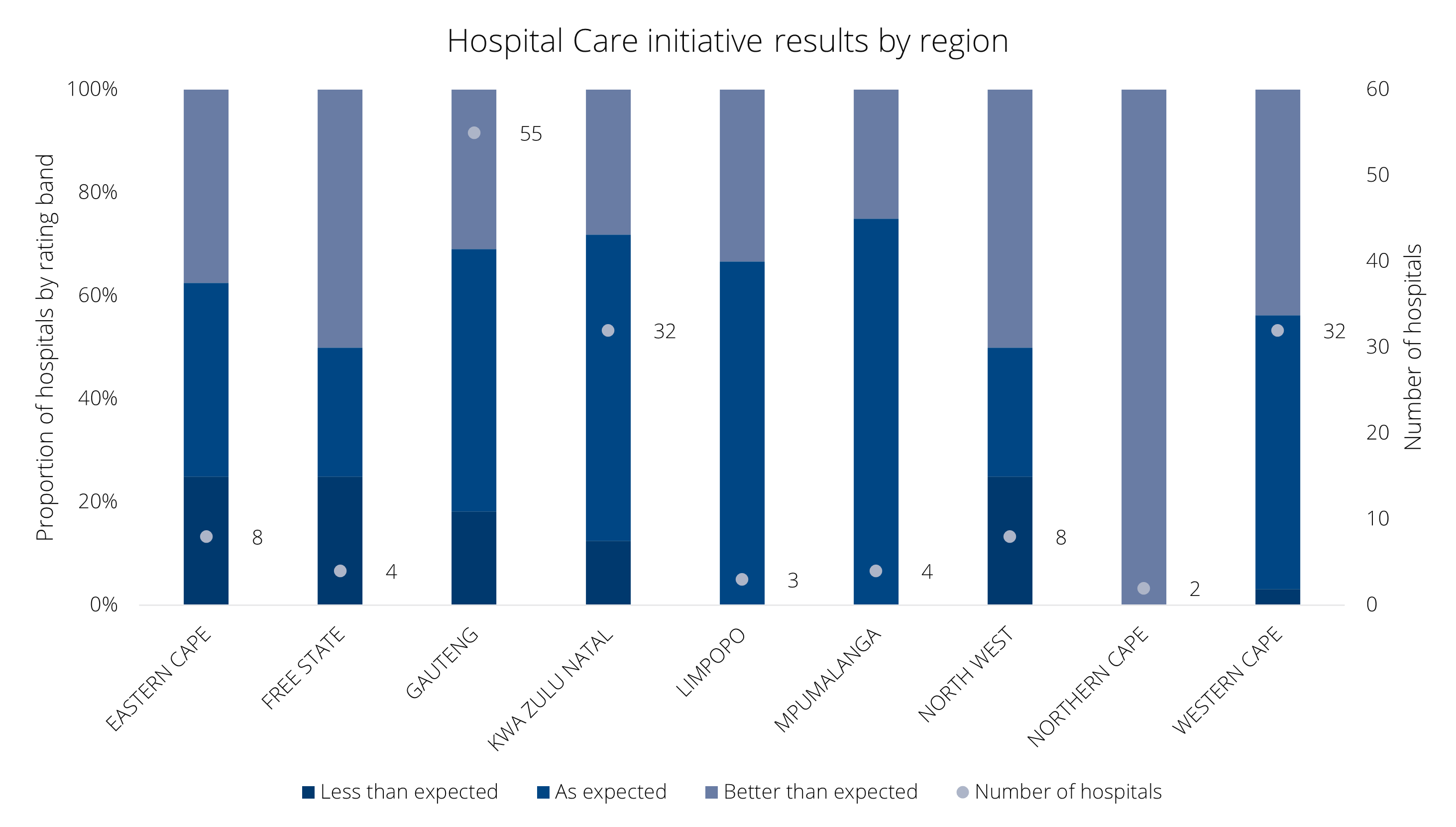
Figure 5: Distribution of hospitals by rating
Discussion and conclusion
Discovery Health's Hospital Care Initiative adapted international quality of care measures and applied them to a wealth of member data across the schemes to produce meaningful measures of quality, cost and patient satisfaction within private hospital care.
Hospital ratings are based on measures representative of the quality of care from that facility for particular procedures, our members' experience at hospitals, and cost efficiency, which influences the cost of medical aid cover.
For consumers, we have converted our measures into understandable, practical information that members can use to make more informed choices when accessing care.
For hospitals, knowledge of relative performance across a range of measures compared with the industry can encourage improvement and quality control. We anticipate that in the future, additional quality indicators will be added, for instance, the rate of hospital-acquired infections.
Members should also consider multiple factors when choosing a hospital, such as location and provider availability. Still, we feel that the Hospital Care Initiative is a positive step in empowering members to make informed choices about care, and increasing transparency and accountability in private healthcare.
Acknowledgements
Acknowledgements for this work span the past 20 years and include both colleagues still and no longer at Discovery Health: Dr Ryan Noach, Dr Jonathan Broomberg, Dr Dave Jacobs, Dr Brian Ruff, Riedwaan Jabaar, Ismail Rasool, Dr Roshini Moodley Naidoo, Dr Geraldine Timothy, Dr Dianne Walker, Luisa Whitelaw, Fundi Maqula, Penny Mekgwe, Lizelle Steenkamp, Chipo Maraire, Thando Ncube, Natasha Rakocija, Tommy Chen, Matt Zylstra, Rob Kirk, Aldu Duminy, Nabeelah Coovadia, Wanja Matthews, Sharon Naidoo, Andy Khoza, Tanya Michas, Jon Crawford, Gary Kantor, Marianne Nel and Dumani Kula. We are incredibly grateful for their contributions that have finally resulted in the seminal publication of healthcare quality outcomes at private hospitals in South Africa
- 1. Hospital Value-Based Purchasing. Centers for Medicare and Medicaid Services (CMS). 2021. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HVBP/Hospital-Value-Based-Purchasing
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Read our related post on how Discovery Health is developing new ways of measuring the quality of hospital care
All information shared on this page is based on perspectives gained from analysis of figures and trends emanating from Discovery Health's data pool. The analysis, which is conducted by Discovery Health's actuarial and data scientist team, aims to encourage industry dialogue. This content is shared for educational and informational purposes only. It does not constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions.

Deep dive: Admission rates across South Africa's four COVID-19 waves confirm Omicron-driven fourth wave's lower severity, and more.
07 July 2022
Authors: Chana Suttner (Actuary, Discovery Health),Michael Cohen (Actuarial Analyst, Discovery Health), Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health

Long COVID symptoms, impact on carrying out daily activities: Survey of just over 7,000 medical scheme members reveals key insights
16 June 2022
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health), Lizelle Steenkamp (Senior Healthcare Statistician, Discovery Health), Lebohang Radebe (Data Scientist, Discovery Health), Dr Smybinn Mathews (Clinician, Discovery Health) and Dr Dave Jacobs (Senior Clinician and Clinical Classification System Architect, Discovery Health)

Discovery's COVID-19 personal resilience index predicts an individual's resilience to serious COVID-19 illness
23 May 2022
Authors: Lizelle Steenkamp (Senior Healthcare Statistician at Discovery Health), Tommy Chen (Actuary at Discovery Health), Jared Champion (Senior Actuary at Discovery Health) and Donald Ntjana (Senior Data Scientist at Discovery Health)