COVID-pneumonia linked to higher hospital admission rate and disease severity than non-COVID pneumonia (2020 - 2021)

Compared to non-COVID pneumonia, COVID-pneumonia resulted in a higher number of admissions (including to ICU and requiring ventilation) and longer lengths of hospital stay over the first two years of the COVID-19 pandemic. This trend stabilised in 2022.
Authors
Discovery Health's Matt Zylstra (Senior Actuary), Lizelle Steenkamp (Senior Healthcare Statistician) and Shirley Collie (Chief Research Actuary).
Understanding pneumonia
According to World Health Organization (WHO) estimates, 450 million cases1 of pneumonia were recorded worldwide, every year, as far back as 2002. More recently the WHO reports2 that 'pneumonia is the single largest infectious cause of death in children worldwide. Pneumonia killed 740 180 children under the age of 5 in 2019, accounting for 14% of all deaths of children under 5 years old but 22% of all deaths in children aged 1 to 5 years.'
Pneumonia is a common illness where inflammation and fluid in the lungs makes it difficult to breathe and results in a cough (which may produce mucous), fever, shortness of breath, chest pain and other related symptoms. Some types of pneumonia are contagious. The disease is spread when people talk, sneeze or cough and send respiratory droplets into the air.
Why can pneumonia result from other illnesses - such as flu or COVID-19?
COVID-19 disease (caused by the SARS-CoV-2 virus) was first reported in Wuhan, China, in 2019, and subsequently spread globally to become the fifth documented pandemic since the 1918 flu pandemic3.
Most people infected with COVID-19 experienced mild to moderate respiratory illness and recovered. However, people at high risk of serious COVID illness (such as the elderly, children under age one, pregnant women and immunocompromised people) required medical attention , including admission to an acute hospital facility to treat complications - such as COVID-pneumonia4.
COVID-19 disease severity and admissions differed across South Africa's four main waves of COVID-19 infection. These dynamics were determined by the pathogenicity of variants that drove each wave, vaccination rates and rates of population wide seropositivity at the time of each wave.
- Read our July 2022 analysis on admission rates across South Africa's four waves of infection.
COVID-19 vaccines were developed to reduce morbidity and mortality rates associated with COVID-19 infection. In South Africa these vaccines were rolled out in different phases, from 17 February 20215 in a process prioritising those at greatest risk of severe illness.
This analysis compares COVID-pneumonia to non-COVID pneumonia, across a range of metrics
Our data analysis spans 2020 to 2022 and looks at how admissions to hospital to treat COVID-pneumonia differed from admissions for pneumonias unrelated to COVID-19 (which we call non-COVID pneumonia). We investigate these dynamics within the Discovery Health Medical Scheme (DHMS) member base.
To classify members as vaccinated or unvaccinated we looked at their vaccination status at the time of their admission.
We analysed data relating to all members but also carried out a further sensitivity analysis looking only into unvaccinated DHMS members. We did this so that we could interpret baseline COVID-pneumonia data i.e. without the impact of COVID vaccination on members.
Defining COVID-pneumonia
We defined COVID-pneumonia admissions as those that happened within 14 days of a DHMS member getting confirmation of contracting COVID-19 - either confirmed by PCR test result or where the member was admitted for COVID-19 with confirmation of the disease (where the U07.1 diagnosis code indicated the SARS-CoV-2 virus has been identified through testing).
- Only admissions related directly to COVID-19 and allocated to the pneumonia Diagnosis Related Group (DRG), were considered in this analysis.
- The DRG system is an international classification of admissions based on the reason for admission, necessary procedures and any complications or co-morbid conditions that affect the resources required during the admissions.
- Admissions related to COVID-19 complications - like strokes or heart attacks - or where surgery was performed, were excluded from this analysis as the costs involved in these admissions would skew the data on pneumonia, which we wanted to focus on.
Pneumonia admissions fall under one of three levels of DRG severity
The DRG system assigns each hospital admission to one of three severity levels, which are determined by complications and/or co-morbid conditions that the member has during the admission (as these are expected to impact the admission cost or member's length of stay in hospital).
These severity levels are provided by the hospital using ICD-10 diagnosis codes and are supplemented by the medical scheme with ICD-10 codes related to chronic conditions a member is registered as having:
- Level 1: A member has no complications or comorbidities.
- Level 2: A member has a minor complication or comorbidity, such as epilepsy.
- Level 3: A member has a major complication or comorbidity such as stroke, pulmonary embolism or sepsis.
How did the number of admissions for COVID-pneumonia compare to admissions for non-COVID pneumonia over time?
Figure 1 depicts admission data for DHMS members from 2020 to 2022.
a) For COVID-pneumonia:
- 2020: 14,184 admissions
- 2021: 34,691 admissions
- 2022, a drop to 8,086 admissions.
b) For non-COVID pneumonia:
- 2020: 7,630 admissions
- 2021: 9,508 admissions
- 2022, an increase to 16,431 admissions.
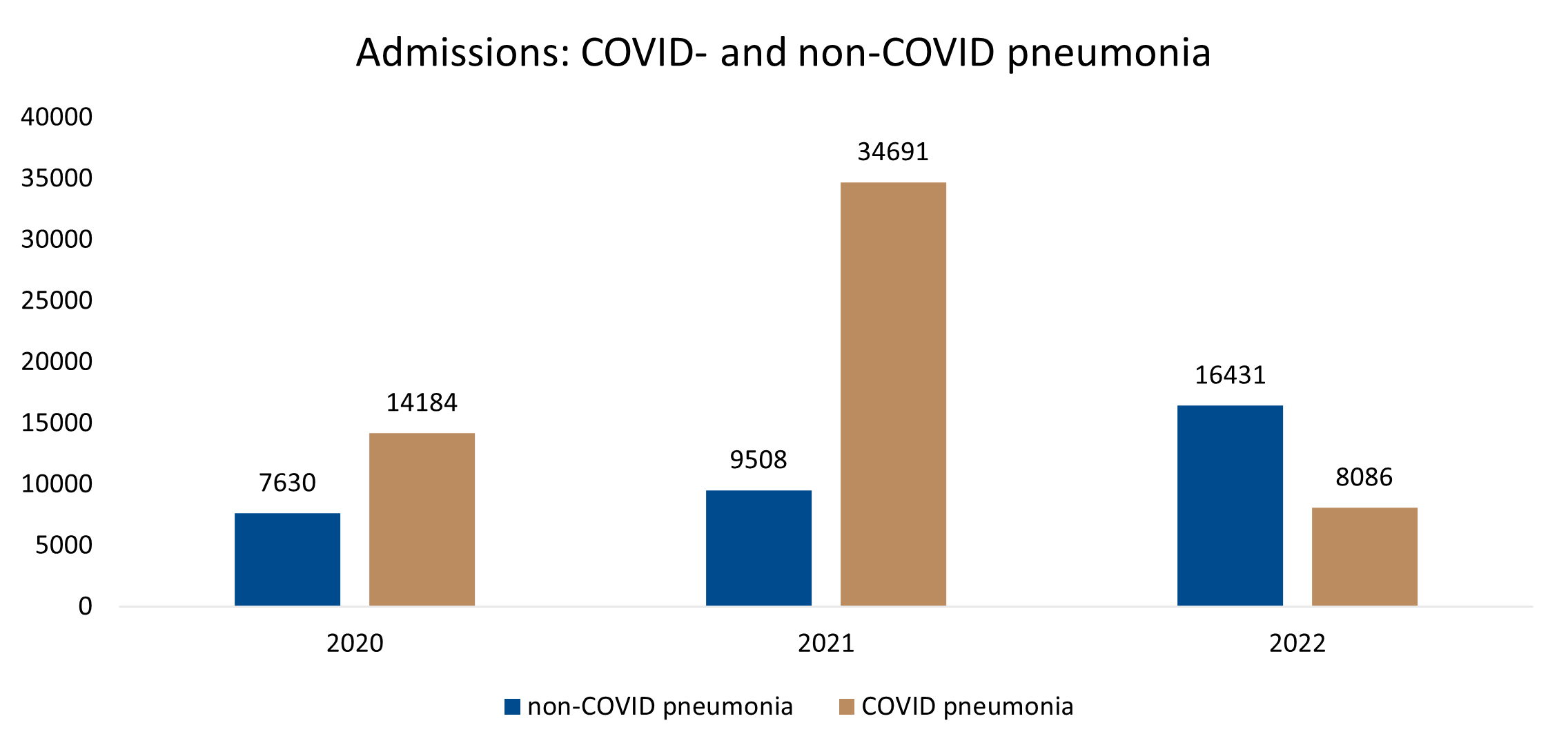
Figure 1 : Number of DHMS members admitted to treat COVID- and non-COVID pneumonia from 2020 to 2022
Our sensitivity analysis showed that as more and more members were vaccinated over time, the proportion of unvaccinated members admitted for COVID-pneumonia decreased from 100% in 2020 (at the start of the pandemic), to 77% in 2021, and to 42% of overall COVID-pneumonia admissions in 2022 (Figure 2).
This is because as more people became eligible for and received COVID-19 vaccines, the proportion of unvaccinated DHMS members decreased overall.
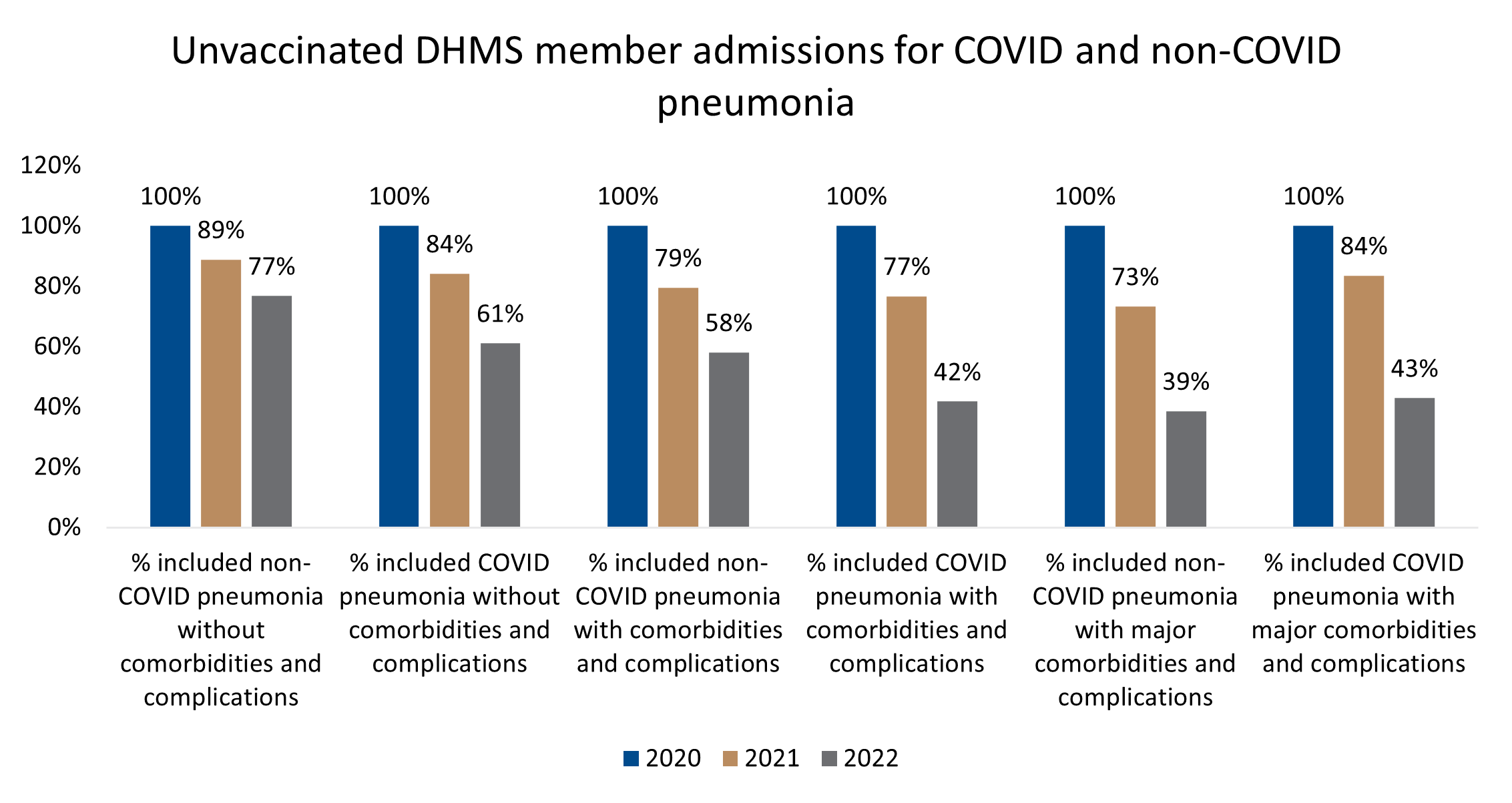
Figure 2 : Unvaccinated DHMS member admissions across severity groups and over time, for COVID-pneumonia and non-COVID pneumonia.
It's important to note that this data cannot be used to inform an assessment of COVID-19 vaccine effectiveness. It does not take into account the number of DHMS members who were vaccinated, nor the disease burden differences between those vaccinated and unvaccinated.
- For more information on vaccine effectiveness, refer to our past analyses:
- Discovery Health releases at-scale real-world analysis of Omicron outbreak; including collaboration with the SA Medical Research Council (SAMRC) to analyse vaccine effectiveness
- Discovery Health contributes key control group to first at-scale, real-world study of J&J COVID-19 vaccine's effectiveness (published in Lancet journal).
- 2 doses of the J&J or 2 doses of the Pfizer COVID-19 vaccine? New research out of South Africa reveals they're equally effective against serious illness caused by the Omicron variant.
How did the cost of admissions for COVID-pneumonia compare to admissions for non-COVID pneumonia, over time?
Comparing the average cost of admissions shows COVID-pneumonia admission costs were significantly higher than costs for non-COVID pneumonias in 2020 and 2021. This is evident across all levels of severity for these years.
COVID-pneumonia admission costs were higher by 40.2% to 85.9% in 2020 and 38.9% to 57.5% in 2021.
However, in 2022 the cost of treating COVID-pneumonia decreased to less than the cost of treating non-COVID pneumonia (Figure 3, which shows the percentage difference in average cost).
And, this trend was consistent in the unvaccinated Scheme member base too (Figure 4).
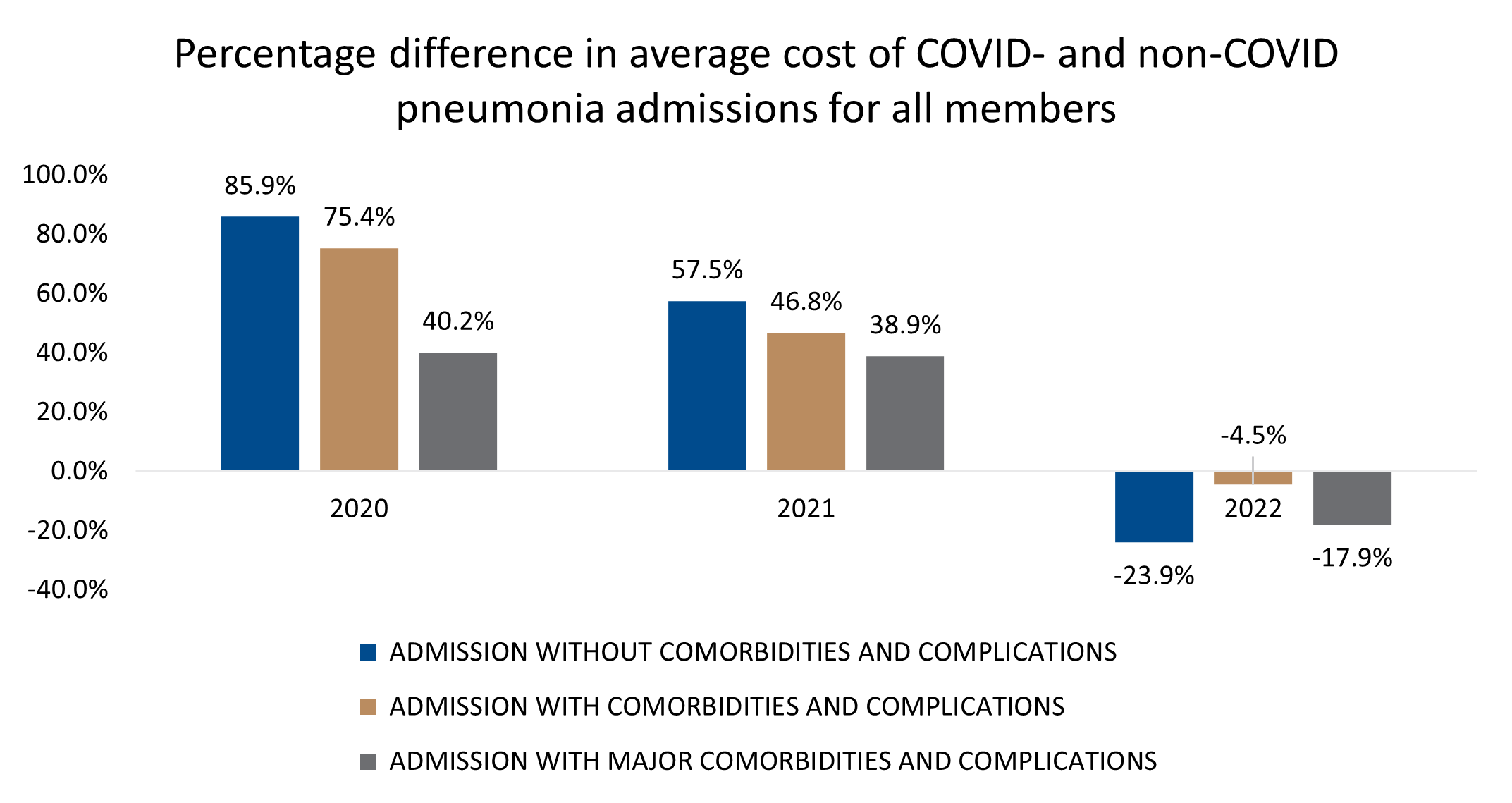
Figure 3 : Percentage difference in average cost of treatment for COVID- and non-COVID pneumonia over time (2020-2022).
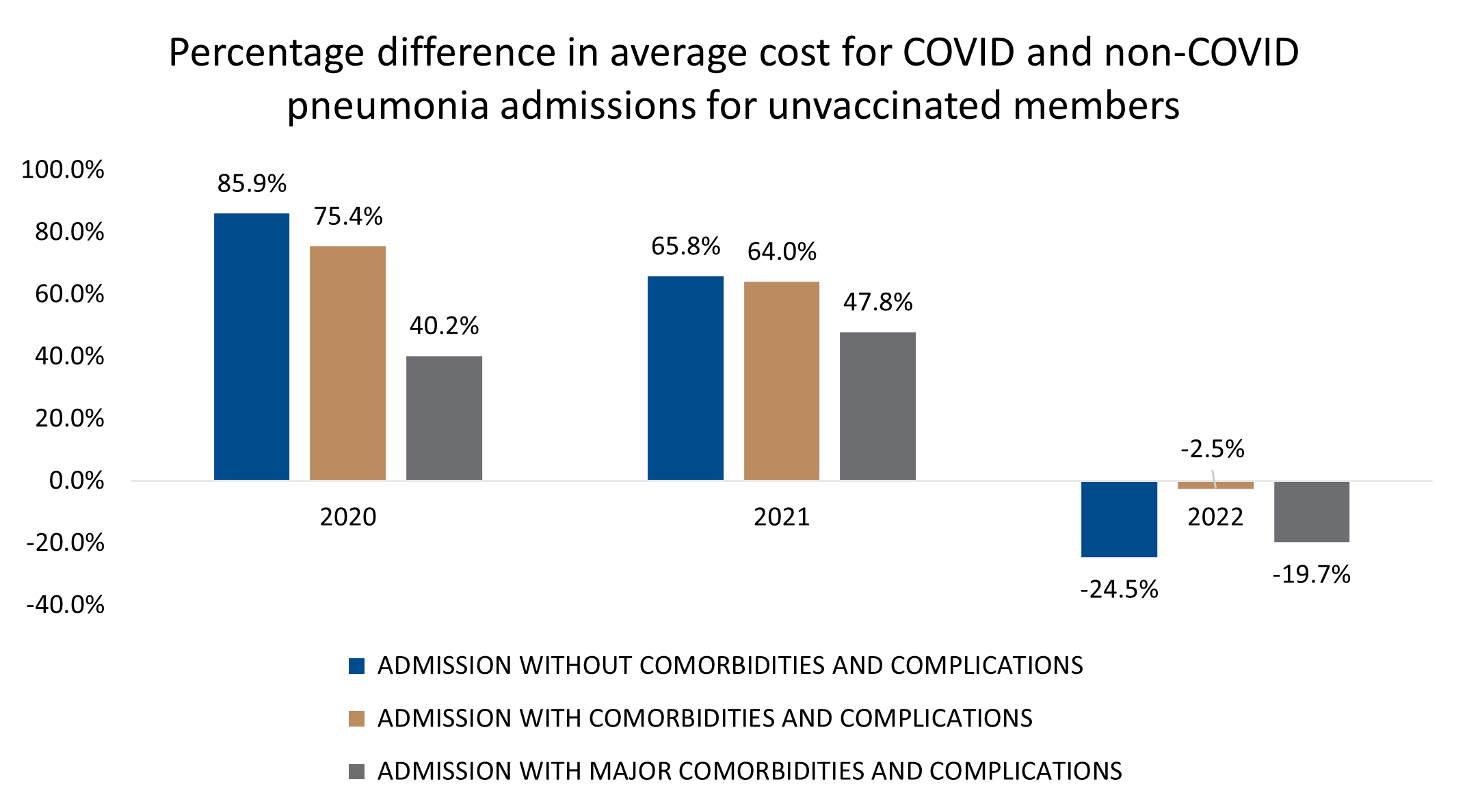
Figure 4 : Percentage difference in average cost of treatment for COVID- and non-COVID pneumonia over time (2020-2022), in unvaccinated DHMS members.
How did DHMS members' length of stay in hospital for COVID-pneumonia compare to non-COVID pneumonia, over time?
Comparing average length of stay in hospital for a COVID- and non-COVID pneumonia admissions, we see that in 2020 and 2021, COVID-pneumonia admissions led to significantly longer stays in hospital, at all three severity levels. This ranged from 12.0% to 52.7% longer length of stay in 2020 and 8.9% to 34.1% longer length of stay in 2021.
This trend is once again completely different in 2022 where the average length of stay for COVID-pneumonia admissions was lower than for non-COVID pneumonia admissions (Figure 5).
The trend was consistent for the unvaccinated population (Figure 6).
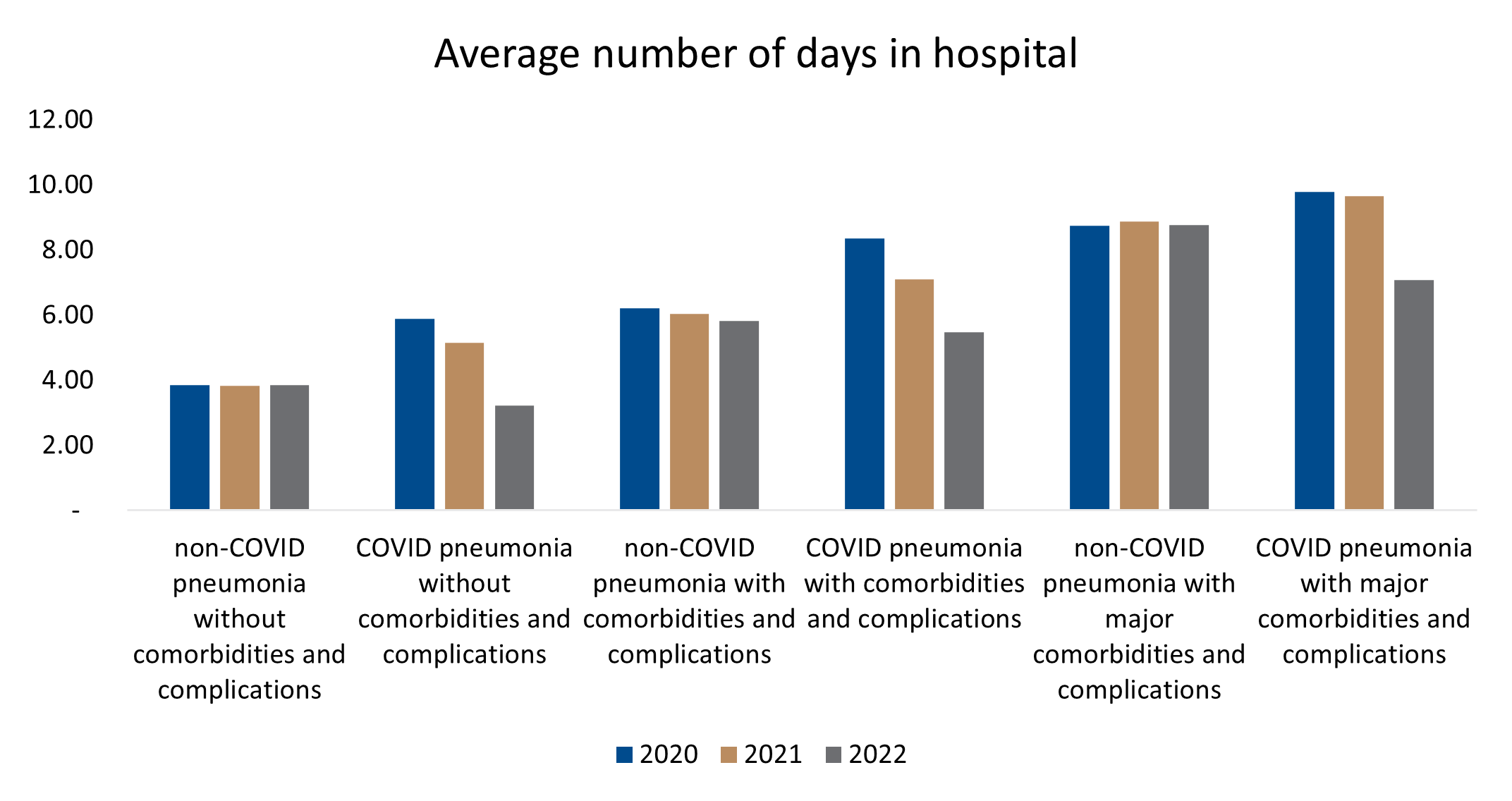
Figure 5 : Difference in average length of stay related to admissions for COVID- and non-COVID-pneumonia, across severity levels and over time (2020 to 2022).
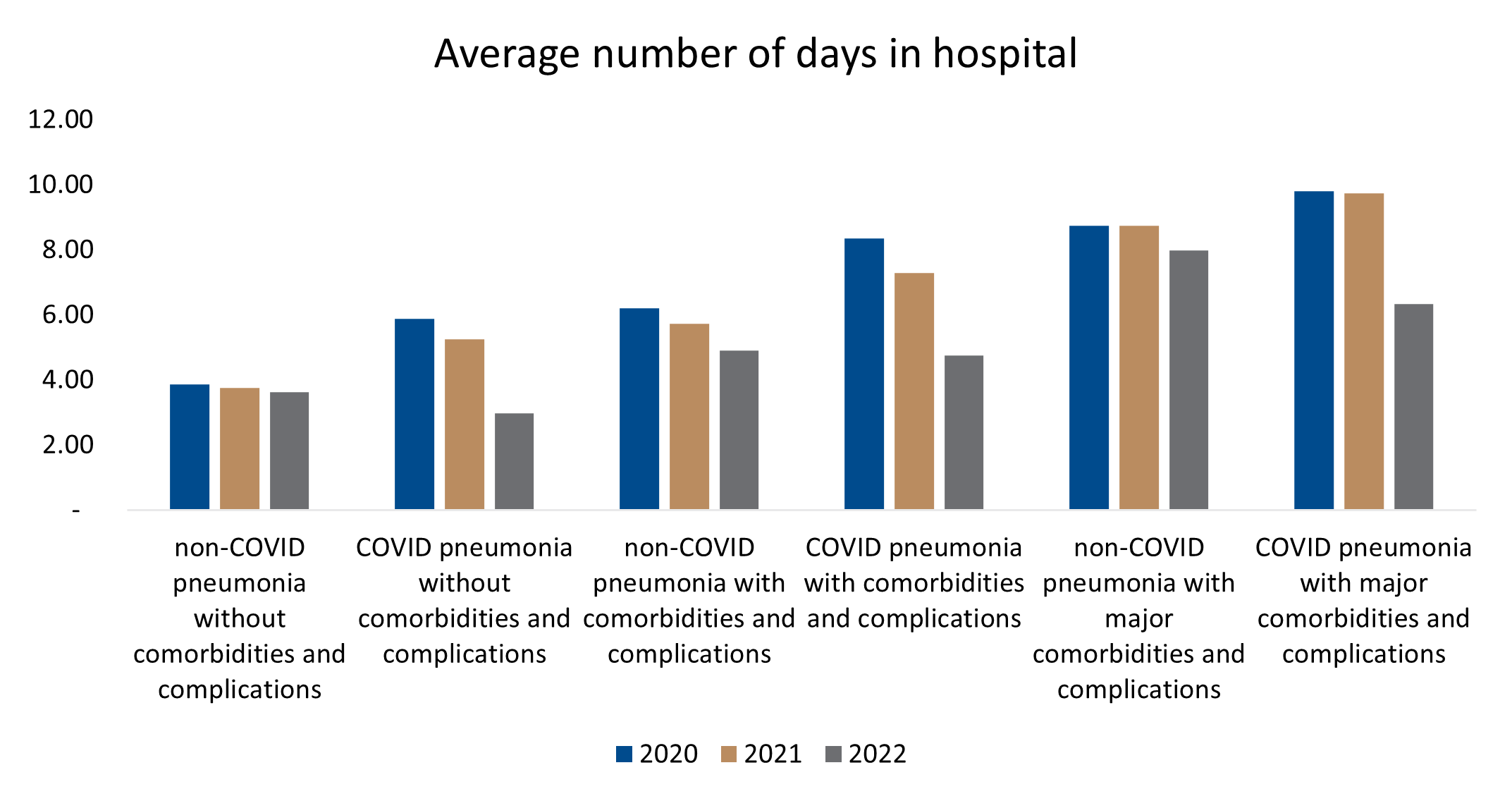
Figure 6 : Difference in average length of stay related to admissions for COVID- and non-COVID-pneumonia, across severity levels and over time (2020 to 2022), in unvaccinated DHMS members.
To what extent did members admitted for COVID- or non-COVID pneumonia require admission to ICU?
In 2020 and 2021, a significantly higher percentage of patients were admitted to ICU for COVID-pneumonia than for non-COVID pneumonia. This is evident across all three levels of disease severity.
In 2020, 1.6% of Level 1 non-COVID pneumonias (where patients had no comorbidities and/or complications) were admitted to ICU, compared to 4.2% of COVID-19-related pneumonias at this severity level admitted to ICU.
Consistent trends were seen in higher severity groups.
These trend changed in 2022, where ICU admissions for COVID-pneumonias were lower than for non-COVID pneumonias (Figure 7).
Again, a similar trend was evident in the unvaccinated population (Figure 8).
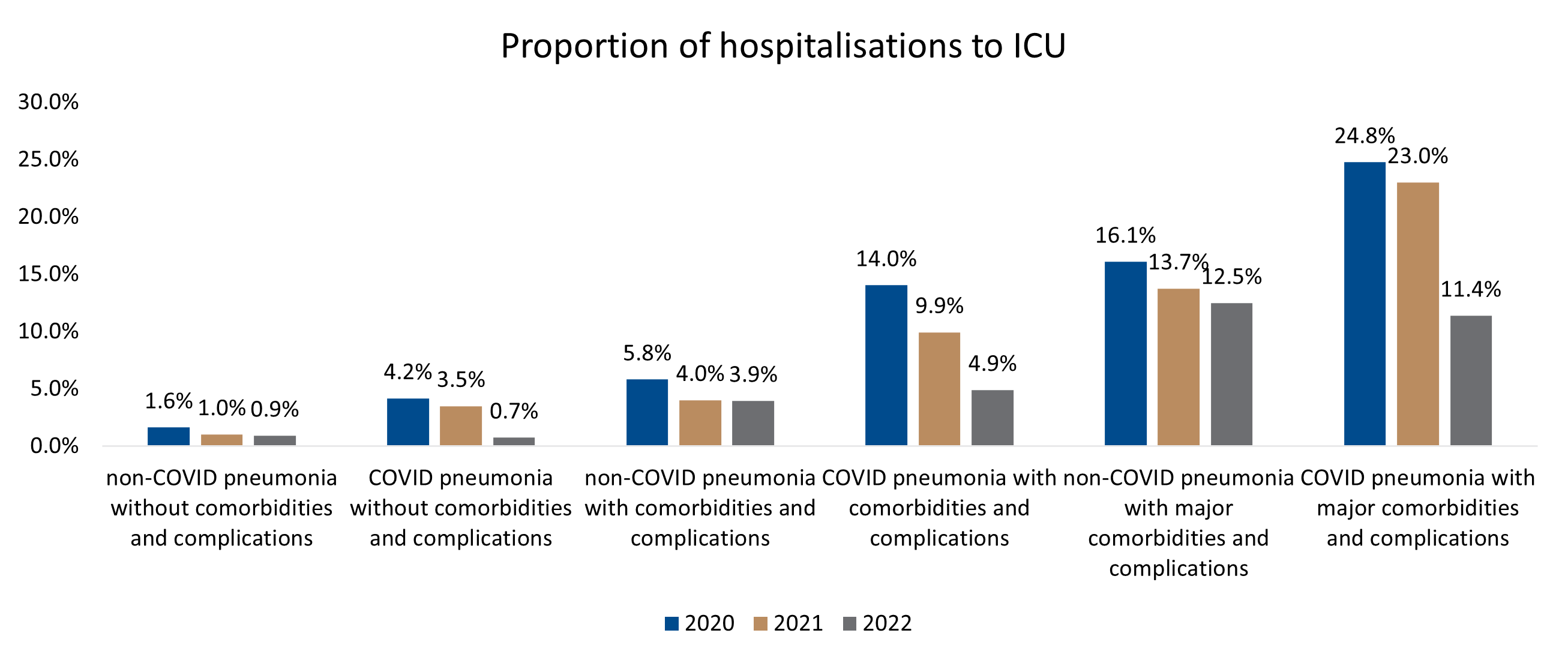
Figure 7 : Proportion of DHMS members admitted to ICU for treatment of COVID- and non-COVID pneumonia over time.
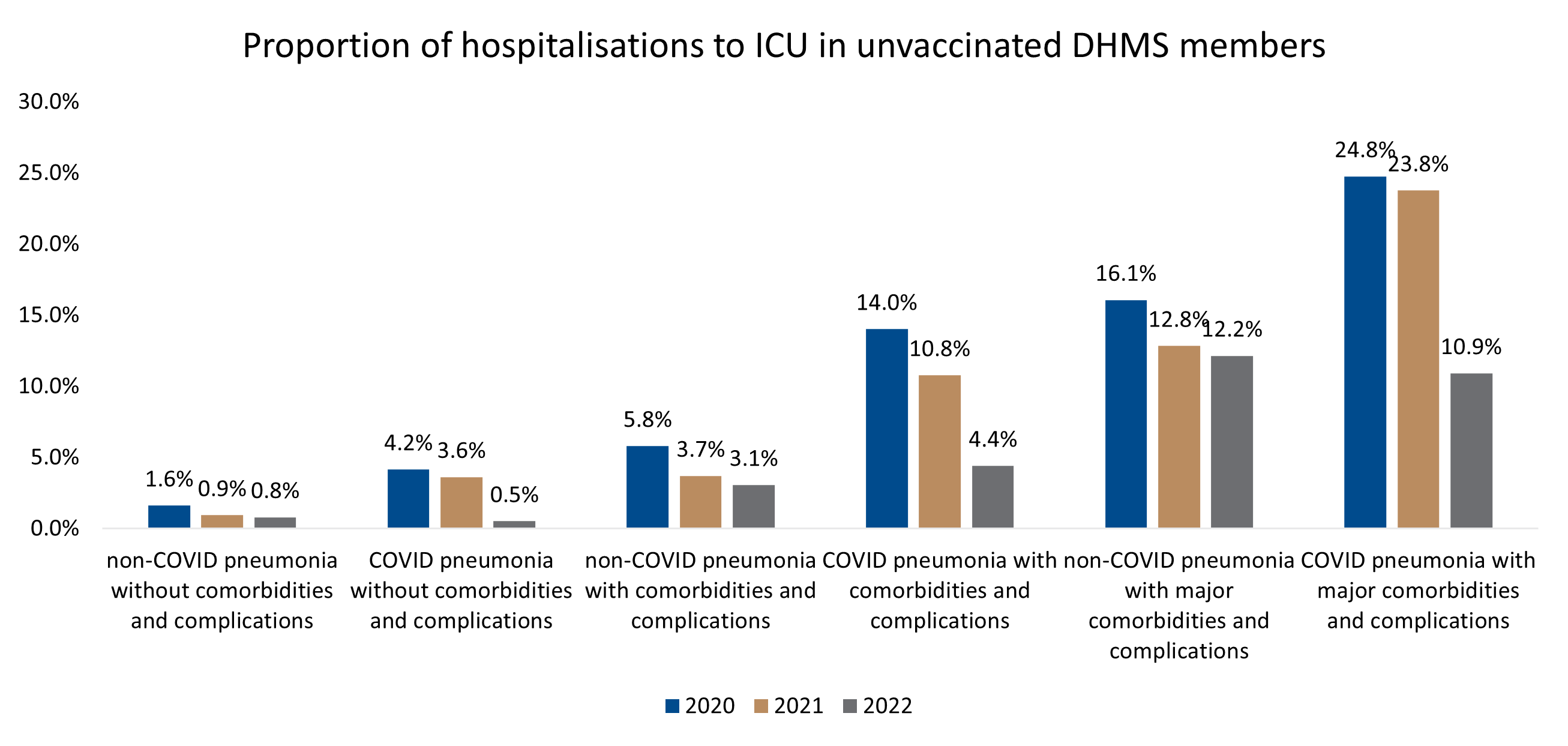
Figure 8 : Proportion of DHMS members admitted to ICU for treatment of COVID- and non-COVID pneumonia over time, in the unvaccinated member population.
To what extent did members admitted to ICU for COVID- or non-COVID pneumonia need ventilation?
Across all three levels of disease severity, in 2020 and 2021 a significantly higher percentage of DHMS members admitted to ICU for COVID-pneumonia needed ventilation, than did members admitted for non-COVID pneumonia.
In 2022, the trend reversed (Figure 9).
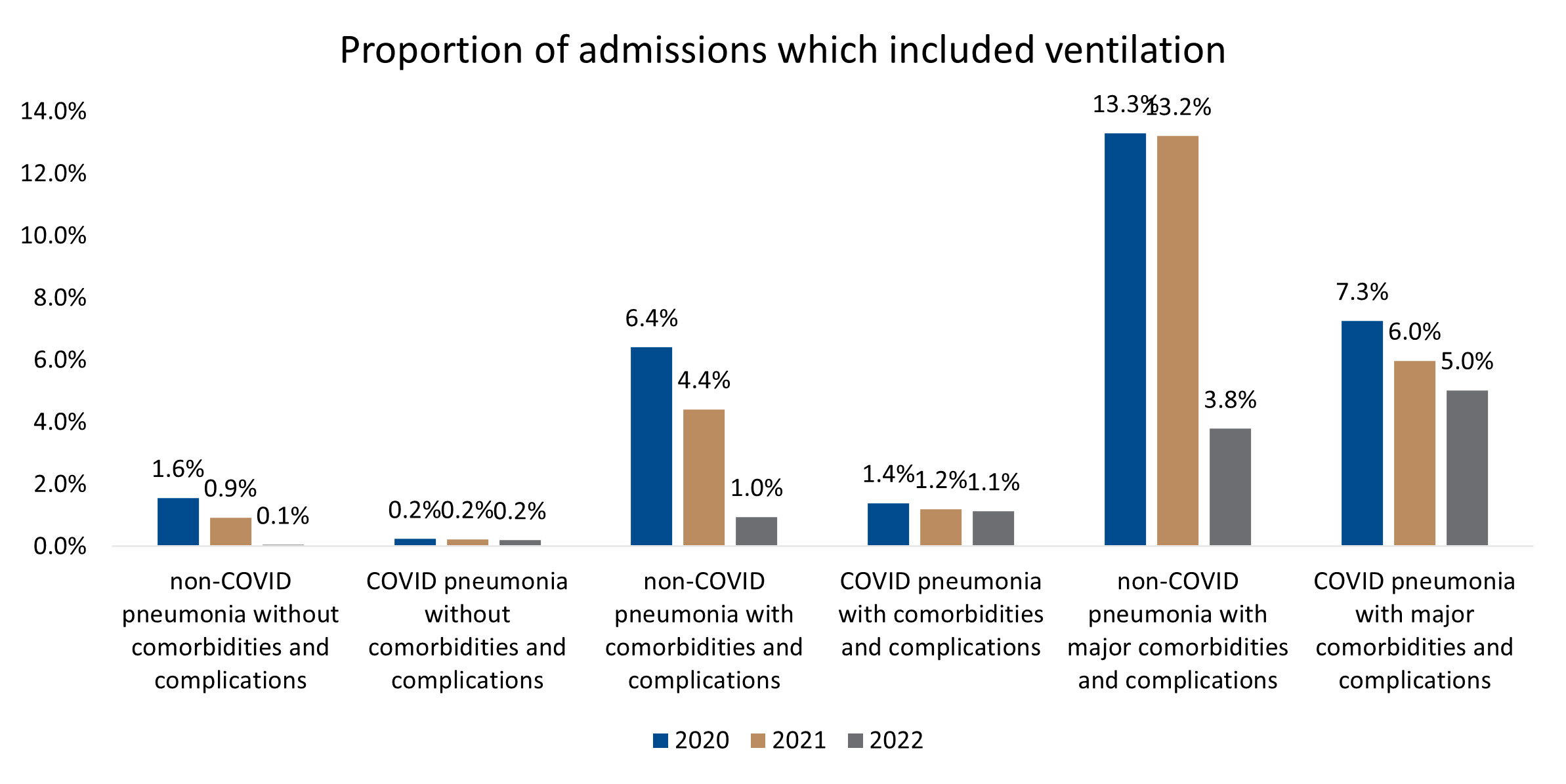
Figure 9 : Proportion of patients needing ventilation for COVID- and non-COVID pneumonia over time (2020-2022).
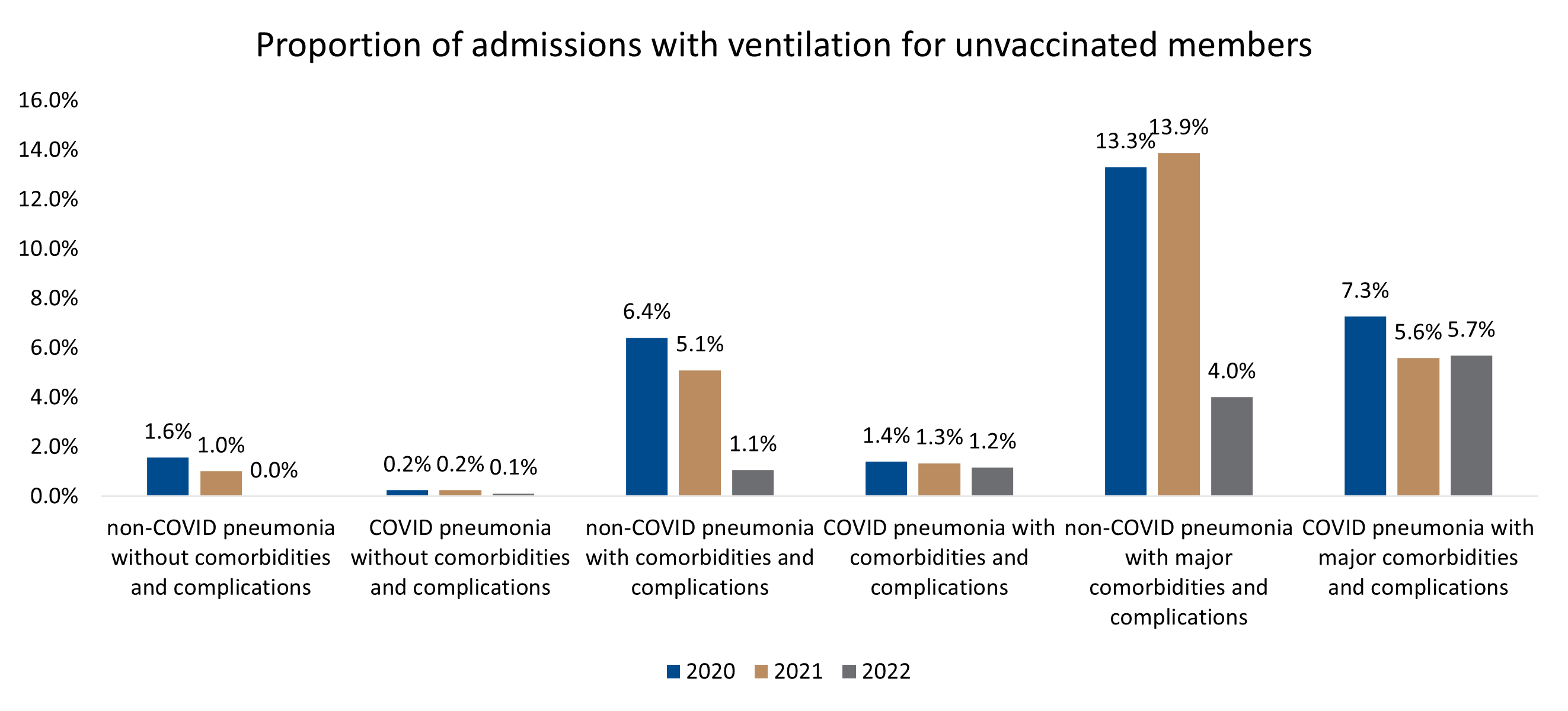
Figure 10 : Proportion of patients needing ventilation for COVID- and for non-COVID pneumonia, over time (2020-2022), in the unvaccinated DHMS member population.
Conclusion
COVID-pneumonia resulted in a higher number of admissions (also to ICU and requiring ventilation), higher admission costs and longer lengths of hospital stay over the first two years of the COVID-19 pandemic.
COVID-19 disease severity reduced over time due to the emergence of less pathogenic variants, increasing COVID-19 vaccine penetration and also seropositivity in the DHMS and South African population.
In earlier waves of infection those admitted for COVID-pneumonia experienced higher levels of morbidity and required more hospital resources (ICU, ventilators, and total length of stays) to treat non-COVID pneumonia.
While admissions for non-COVID pneumonia were lower during the peak pandemic years (2020 and 2021) than admissions for COVID-pneumonia, the consequent use of hospital resources for non-COVID pneumonia remained fairly stable over the analysis period.
In 2022, COVID-19 pneumonia admissions reduced relative to 2020 and 2021 and resulted in the use of fewer hospital resources, than for non-COVID pneumonia.
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7138033/
2. https://www.who.int/health-topics/coronavirus#tab=tab_1
3. https://www.sciencedirect.com/science/article/pii/S2319417020300445
4. https://www.who.int/health-topics/coronavirus#tab=tab_1
5. https://www.discovery.co.za/corporate/covid-19-understanding-sa-vaccine-rollout-plan
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only the data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.