Diabetes and COVID-19: Poor blood-glucose control linked to serious COVID-19 outcomes

Two years into the COVID-19 pandemic, we know that certain factors increase the risk of serious COVID-19-related outcomes. Having diabetes is one of them. However, our analysis shows that well-controlled blood-glucose levels and following a diabetes care programme are linked with a lower risk of serious outcomes.
Authors
Shirley Collie (Chief Analytics Actuary at Discovery Health), Sameera Haneef (Senior Actuary at Discovery Health), Claudia Pastellides (Actuary at Discovery Health) and Dr Dave Jacobs (Senior Clinician and Clinical Classification System Architect at Discovery Health)
Summary of insights
Our research considered a group of members of medical schemes administered by Discovery Health.
1. Blood-glucose control
Compared to members with well-controlled blood glucose, members with poor blood-glucose control had a higher risk of:
- Being admitted to hospital for COVID-19 (2.05 times higher)
- Death from COVID-19 (1.64 times higher).
2. Types of medicine
- Members who claimed for insulin (on its own or with oral medicine) had higher COVID-19-related hospital admission and mortality rates than those who claimed for oral medicine only.
- The risk of COVID-19-related hospital admissions and mortality were higher for members who had claimed for any kind of medicine and had poor blood-glucose control (their HbA1c results were out-of-range).
3. Enrolment in Diabetes Care Programme
Compared with members who were not on the Discovery Health Diabetes Care Programme, members on the programme had a lower risk of being admitted to hospital for COVID-19 and a lower mortality risk.
Investigating the risk of serious COVID-19 outcomes for people with diabetes
According to the National Institute of Communicable Diseases, people of any age who have either type 1 or type 2 diabetes are more likely to get severely ill from COVID-19.
To learn more about the links between diabetes and COVID-19 outcomes, we analysed medical scheme member data over 12 months (between 1 January and 31 December 2020).
- Our sample group
From this analysis, we found that 11 695 members who were registered as having diabetes had been diagnosed with COVID-19 (that's 7% of the 163 753 members registered as having diabetes).
These members were the sample group for this analysis: that is, members of all Discovery Health administered medical schemes who had diabetes and were diagnosed with COVID-19 in 2020.
Within the sample group:
- 96% of members had type 2 diabetes and 4% had type 1 diabetes.
- There were 4 656 hospital admissions (36%) and 1 435 deaths (12%) relating to COVID-19.
- Our methodology
For this analysis, we looked at risk factors and COVID-19 outcomes. The risk factors we considered were:
- How well members controlled their blood glucose
- Their medicine regime (use of insulin)
- Their status on the Diabetes Care Programme.
The COVID-19 outcomes we considered were:
- Hospital admissions (being admitted to hospital because of COVID-19)
- Mortality (deaths related to COVID-19).
To make a meaningful comparison between these risks and outcomes, we also considered the impact of members' demographics and clinical profiles. Confounders we considered were:
- The member's age and sex
- The form of diabetes they had (type 1 or type 2)
- Certain co-morbidities that affect the risk of adverse outcomes for COVID-19 (for example, hypercholesterolaemia, chronic renal failure and cancer).
Confounders, or confounding variables, are factors that affect both risks and outcomes. The details of our analysis and findings are set out below.
Higher risk of COVID-19-related hospital admission and mortality linked to poor glucose control
What we analysed
To see how glucose control might be linked to COVID-19-related outcomes, we analysed the haemoglobin A1c (HbA1c) test results of members in the sample in the months before their polymerase chain reaction (PCR) test results came back positive (that is, before they tested positive for COVID-19).
A haemoglobin A1c (HbA1c) test is a blood test that measures the body's average blood-glucose control in the last two to three months. A high level of HbA1c means there is consistently too much sugar in the blood, putting people at risk of developing the serious health complications associated with uncontrolled diabetes.
For our sample, we considered HbA1c results of 7.5% or less as being in-range - that is, a range which shows effective blood-glucose control.
In our sample:
- 20% of members had an in-range HbA1c level (7.5% or less).
- 27% of members had an out-of-range HbA1c level (higher than 7.5%).
- 53% of members had not done an HbA1c test in the six months before they were diagnosed with COVID-19, so there were no results available. (This may be because these members had not done their routine screening checks, something we explore in more detail further on.)
These results are shown in Figure 1.
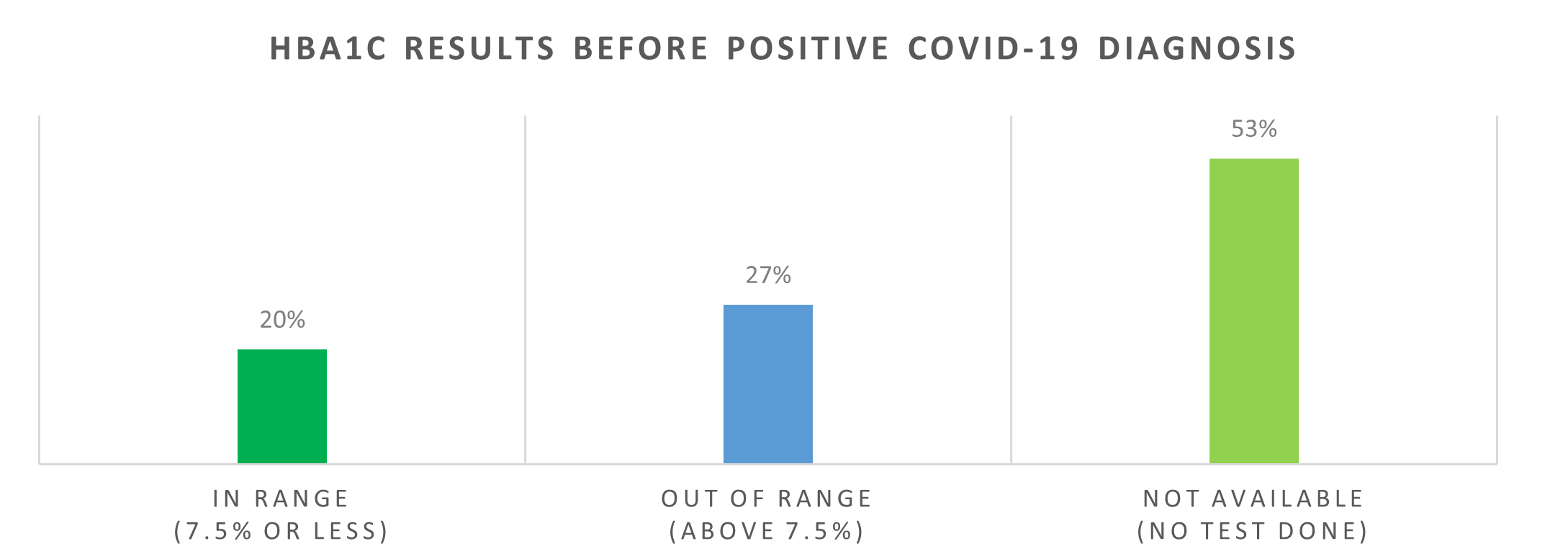
Figure 1: Sample group's HbA1c results before positive COVID-19 diagnosis
Findings from this analysis
Finding 1: Members with poor blood-glucose control had a higher risk of COVID-19-related hospital admissions and death.
When we compared the COVID-19-related outcomes of members who had in-range HbA1c results with the outcomes of those who had out-of-range results, we found that:
- Members with out-of-range results had a 2.05-times higher risk of being admitted to hospital for COVID-19.
- Members with out-of-range results had a 1.64-time higher risk of death of death from COVID-19.
These results were statistically significant at a 95% confidence level (see Figure 2).
Interestingly, the 53% of members who had not done an HbA1c test in the six months before their COVID-19 diagnosis had the lowest hospital admissions and mortality rates in the sample group. The fact that they did not have the test may indicate they did not follow routine screening checks for diabetes.
However, the additional layer of information around their risk of serious outcomes leads us believe that these are people who on average have stable, well-controlled blood glucose levels and therefore are most likely not undergoing six-monthly HbA1c tests.
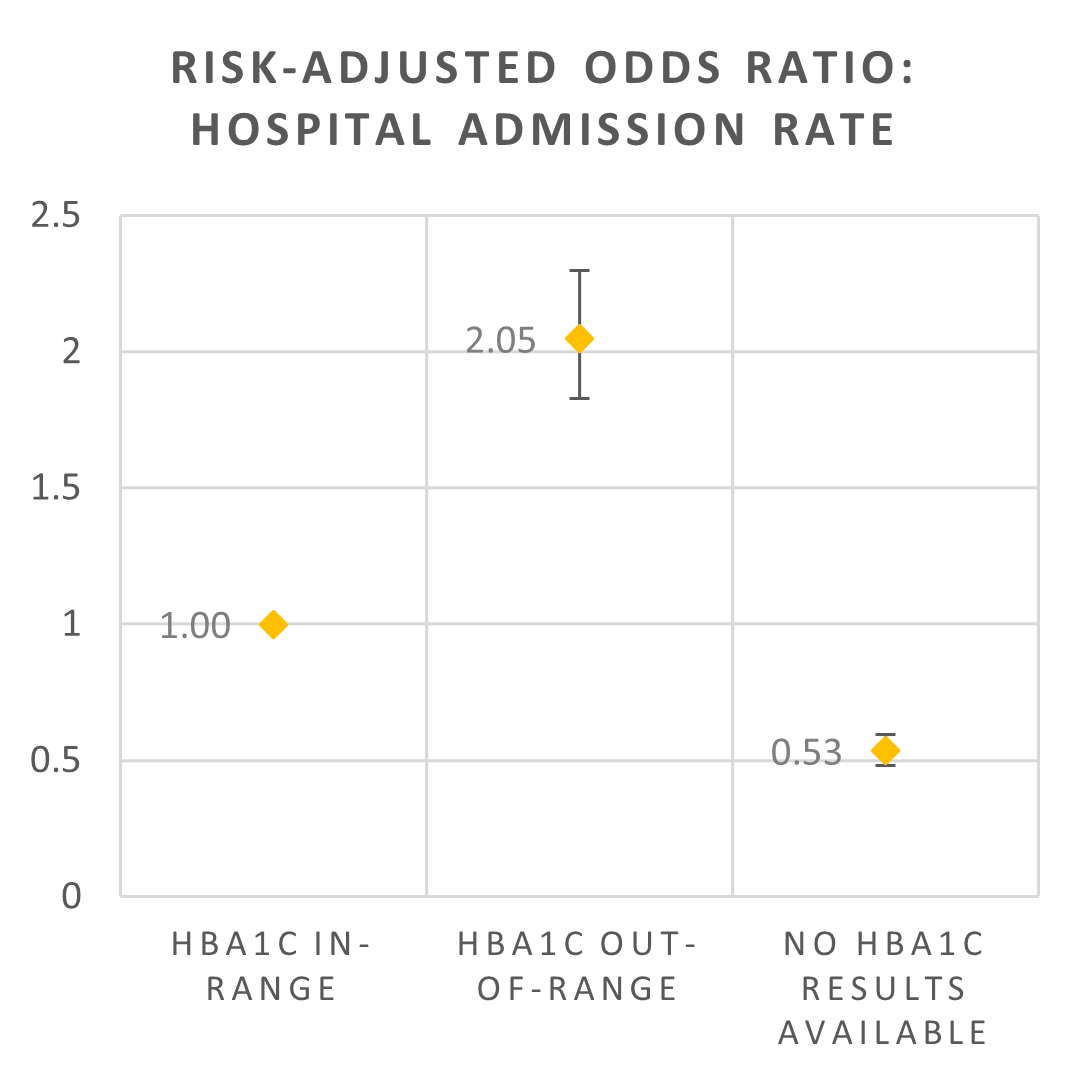
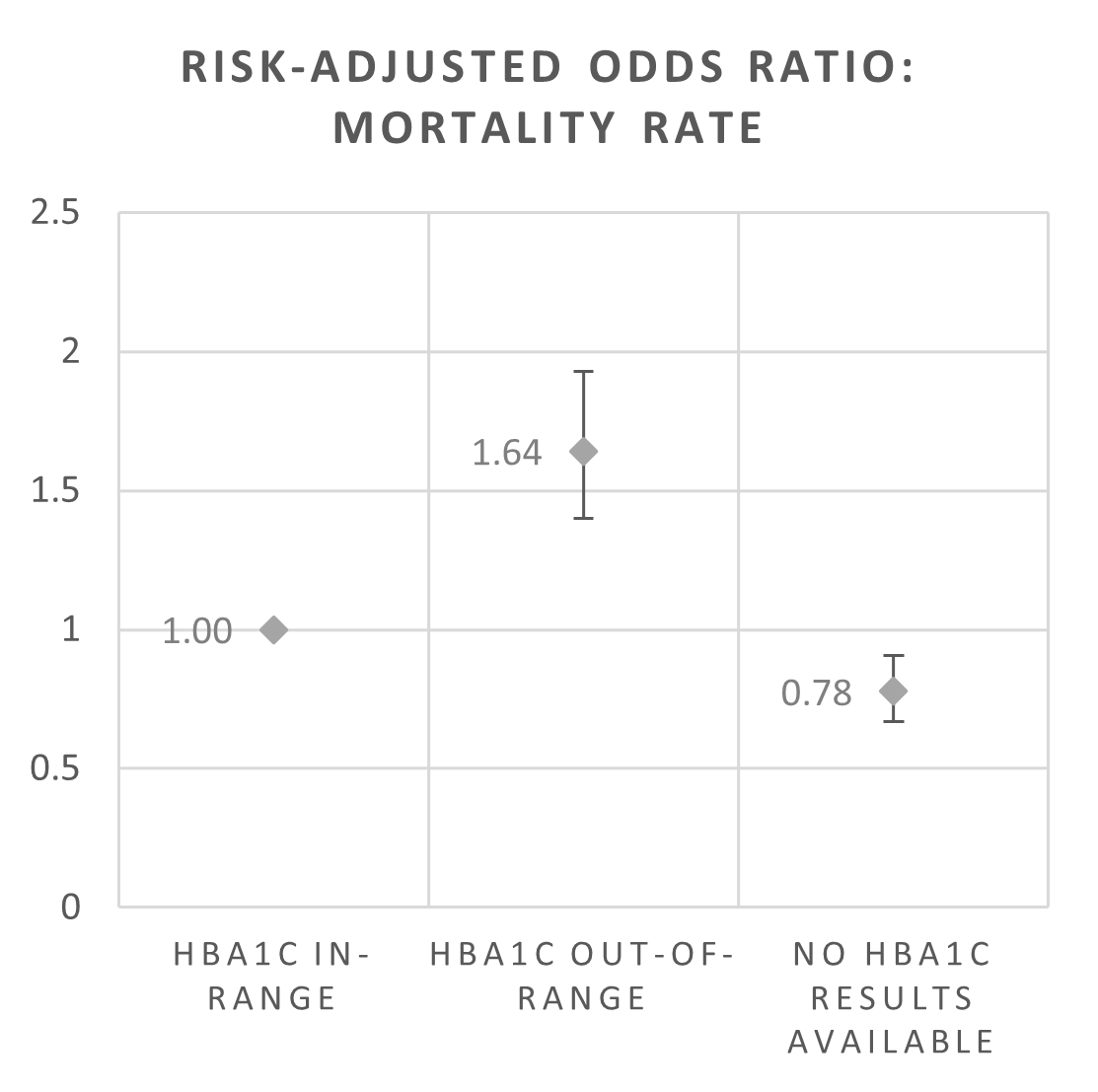
Figure 2: Risk-adjusted odds ratios for COVID-19-related hospital admissions and mortality by HbA1c results
Higher risk of COVID-19-related hospital admission and mortality is linked to poor glucose control at any stage of diabetes
Overview of findings from this analysis
Our analysis shows that more severe stages of diabetes are associated with higher COVID-19-related hospital admissions and mortality rates.
What we analysed
In this section of our analysis, we grouped members in the sample into one of four stages of diabetes. Those in the higher stages have a higher risk profile and more complex illness.
These stages were adapted from the Truven Health Analytics disease staging criteria and were based on specific co-morbidities and complications related to both type 1 and 2 diabetes:
Stage 1: No complications
Stage 2: Micro or macrovascular complications (complications relating to the blood vessels, for example, retinopathy, neuropathy, and vascular disease)
Stage 3: Systemic complications (for example, cellulitis, osteomyelitis, and gangrenous infection)
Stage 4: Affects multiple areas of the body (for example, renal failure, ketoacidosis, acute myocardial infarction (AMI) and sepsis)
In our sample, 73% of members had different stages of complications or co-morbidities (i.e., were categorised as disease stage 2-4).
Figure 3: Sample group's stages of diabetes
Figure 4 shows the COVID-19-related hospital admissions and mortality rates of the sample group across all four stages, before we adjusted for confounding variables such as age, sex, and the number of risk factors for serious COVID-19 illness that a member lives with.
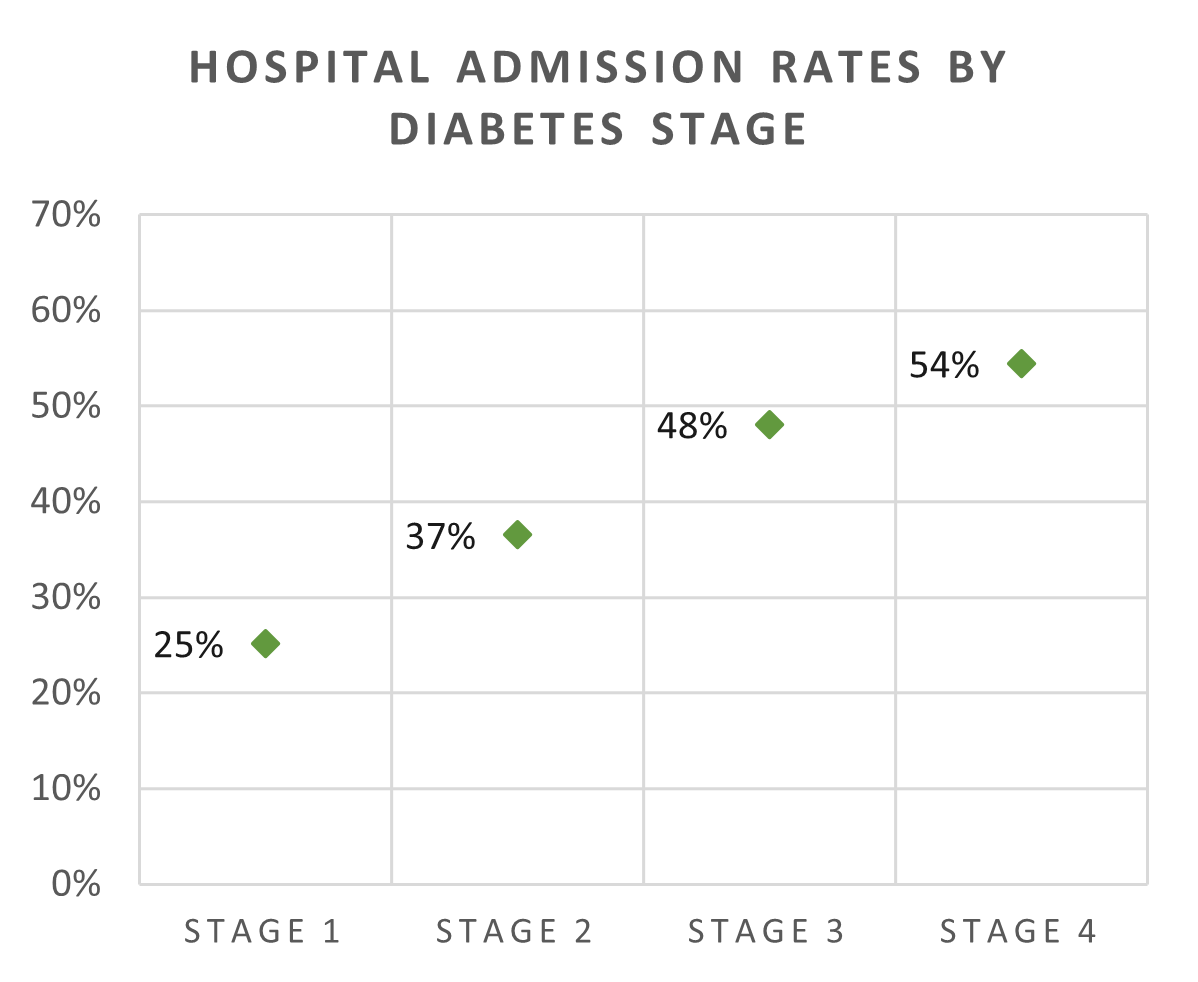
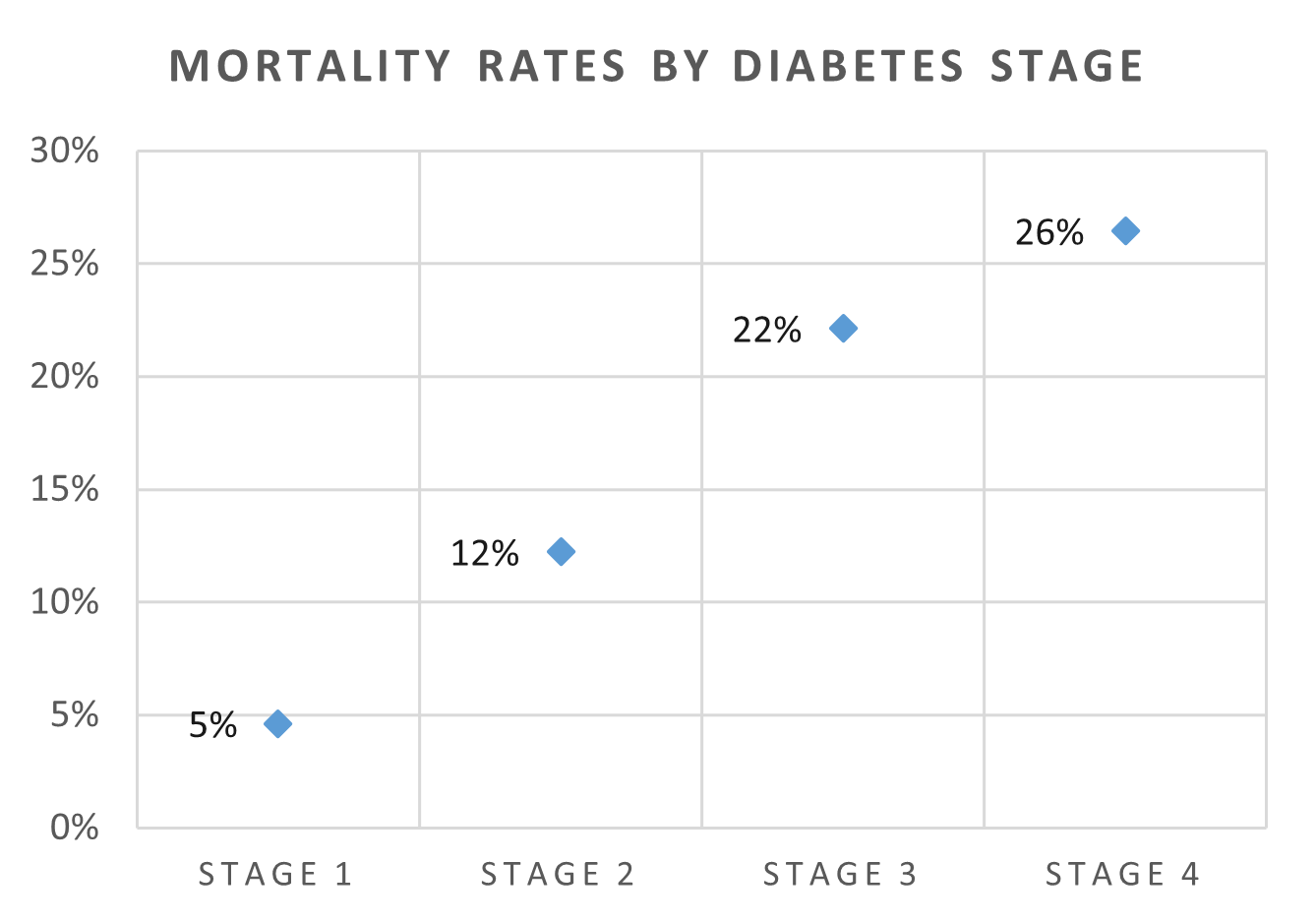
Figure 4: COVID-19-related hospital admission rates and mortality rates by diabetes stage (not adjusted for confounding variables)
Findings from this analysis
Finding 2: Members in stages 1, 2 and 3 with poor glucose control (their HbA1c levels were out-of-range) had a higher risk of COVID-19-related hospital admissions than those with who had-controlled blood glucose.
After adjusting for confounding variables and other differences between in-range and out-of-range members within each stage (Figure 5), we see that members with out-of-range HbA1c levels had a higher risk of COVID-19-related hospital admissions than those with in-range levels:
- Stage 1: 2.56 times higher
- Stage 2: 2.06 times higher
- Stage 3: 1.79 times higher
At stage 4, hospital admission rates were similar for in-range and out-of-range members.
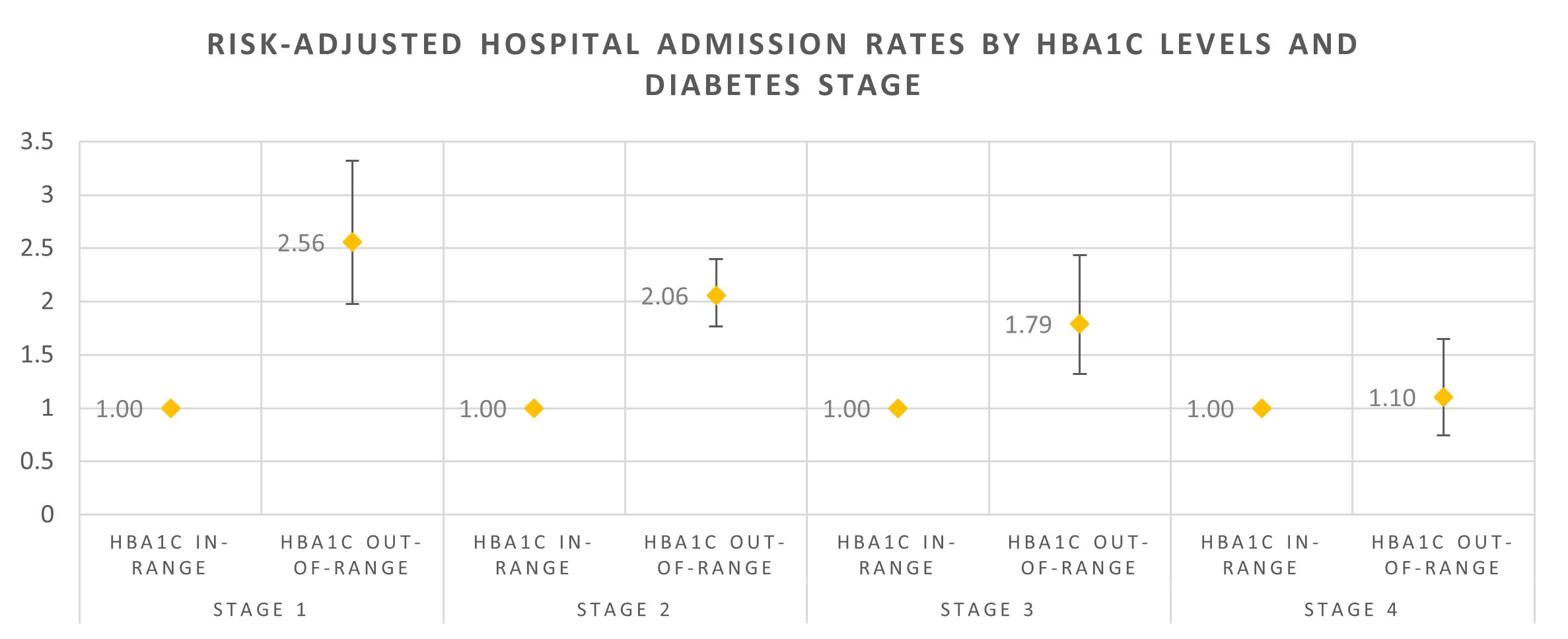
Figure 5: Risk-adjusted odds ratios for COVID-19-related hospital admissions by HbA1c results and diabetes stage
Note: Figure 5 compares the risk faced by members whose HbA1c levels are in-range with those whose HbA1c levels are out-of-range, at each of the four stages. A comparison of risk across the four disease stages cannot be drawn directly from this figure.
Finding 3: Stage 2 diabetes (with vascular complications) was associated with a higher COVID-19-related mortality risk for members with poor blood-glucose control (their HbA1c results were out-of-range).
We also adjusted for confounding variables for in-range and out-of-range members at each stage, (Figure 6). We found that members at stage 2 who had poor blood-glucose control had a 2.04-times higher risk of COVID-19 mortality than those with in-range HbA1c results (good blood-glucose control) - the highest seen across disease stages. Stage 2 which is associated with microvascular and macrovascular complications (complications relating to the blood vessels).
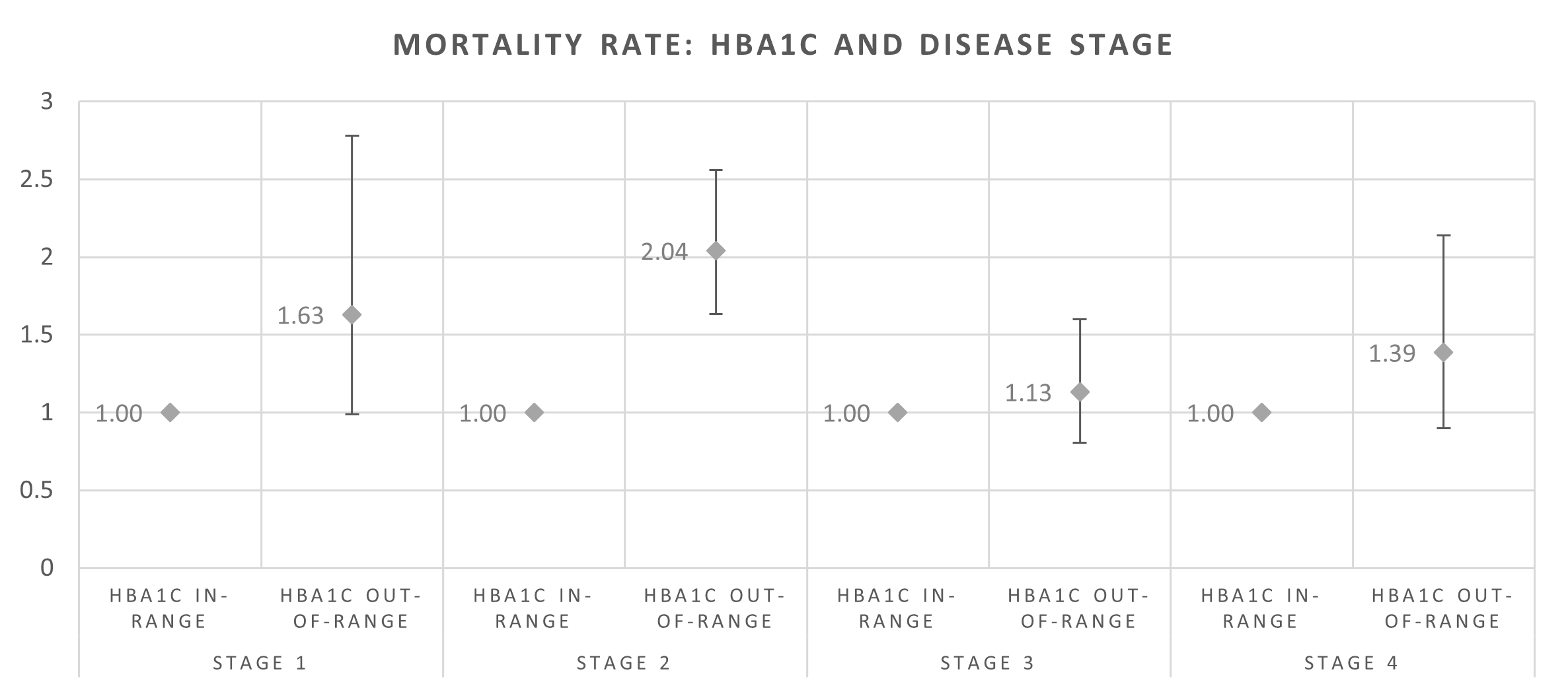
Figure 6: Risk-adjusted odds ratios for COVID-19 mortality by HbA1c results and diabetes stage
Note: Figure 6 compares the risk faced by members whose HbA1c levels are in-range with those whose HbA1c levels are out-of-range, at each of the four stages. A comparison of risk across the four disease stages cannot be drawn directly from this figure.
Claims for insulin medicine were associated with a higher risk of COVID-19-related hospital admission and mortality
What we analysed
The majority (96%) of members in our analysis had type 2 diabetes. And 91% of diabetic members (type 1 and type 2) sent claims to their medical scheme for glucose-lowering medicine in the time of our analysis (1 January to 31 December 2020). Here is a breakdown of those claims:
- 56% claimed for oral medicine only
- 38% claimed for both oral medicine and insulin
- 6% claimed for insulin only.
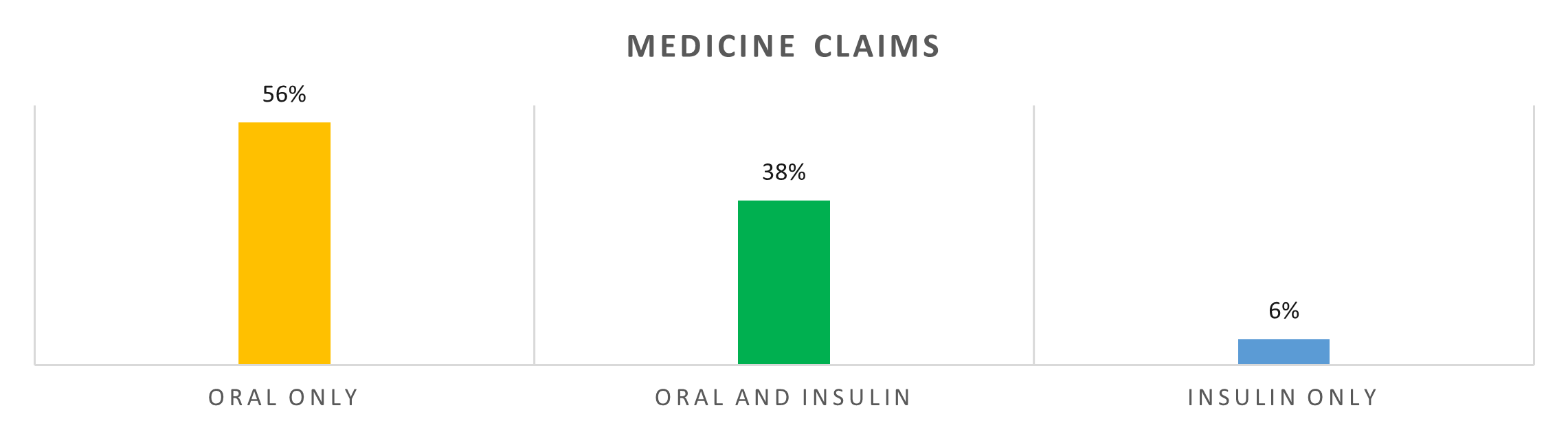
Figure 7: Sample group's medicine claims
The COVID-19-related outcomes for each of these subgroups is shown in Figure 8
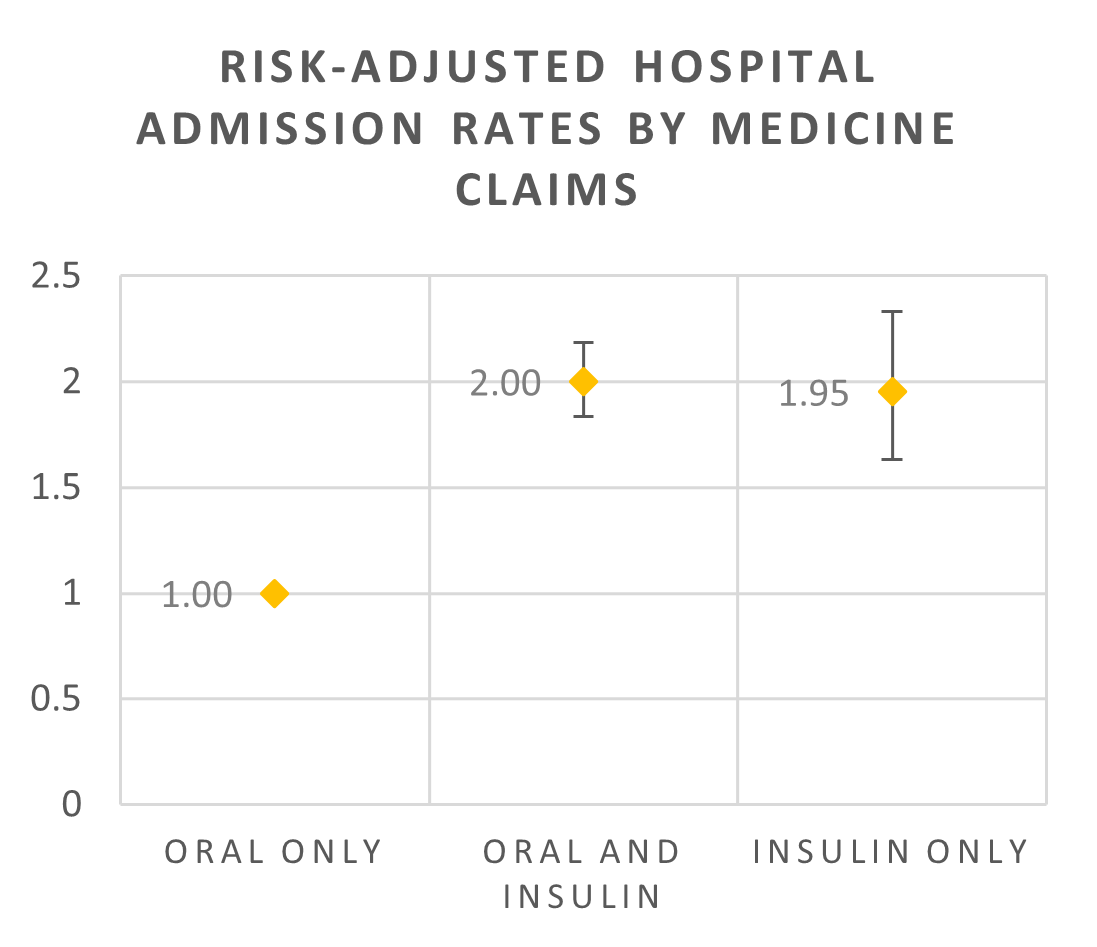
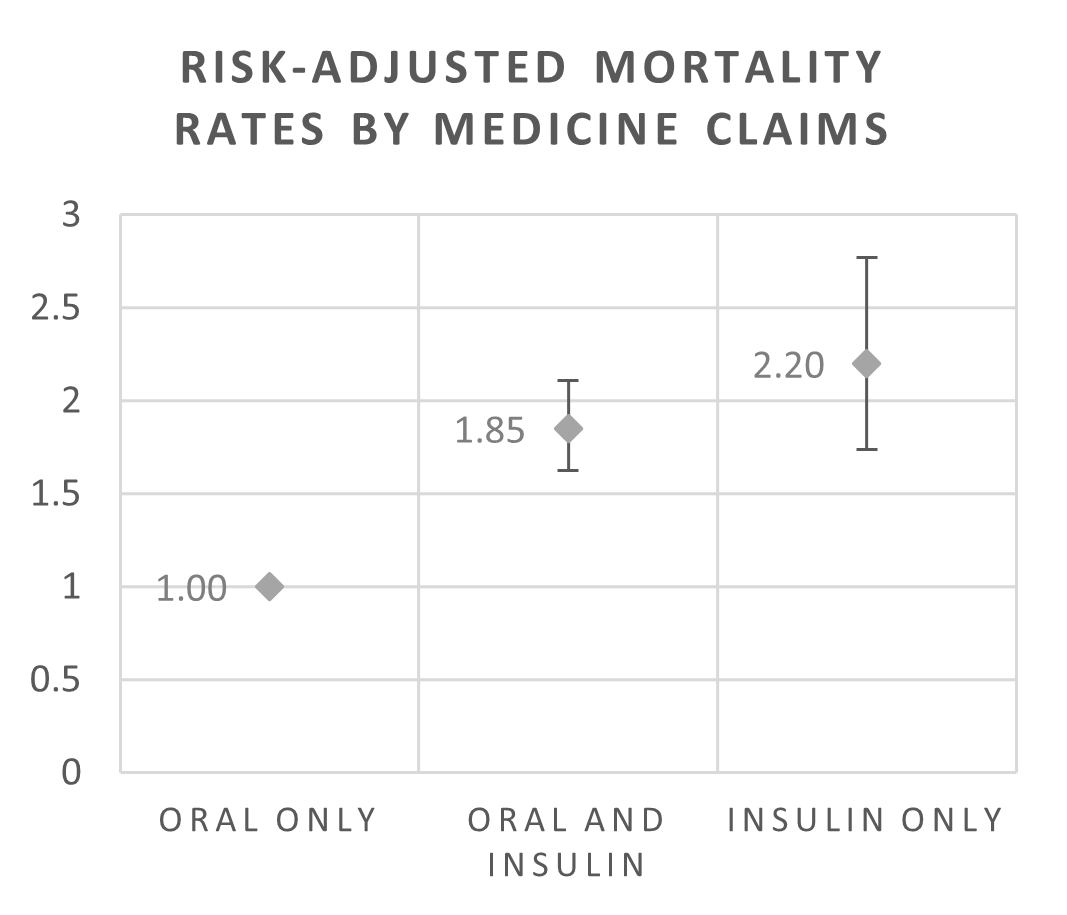
Figure 8: Risk-adjusted odds ratios for COVID-19-related hospital admissions and mortality by medicine claims
Findings from this analysis
Finding 4: Members who claimed for insulin (on its own or with oral medicine) had higher COVID-19-related hospital admission and mortality rates than those who claimed for oral medicine only.
In addition, for members who had claimed for any kind of medicine and had poor blood-glucose control (their HbA1c results were out-of-range):
- The risk of COVID-19-related hospital admissions was 1.75 to 2.02 times higher than for members who claimed but had well-controlled blood glucose (their HbA1c results were in-range)
- The risk of COVID-19-related mortality was 1.16 to 1.9 times higher than for members who claimed but had well-controlled blood glucose (their HbA1c results were in-range).
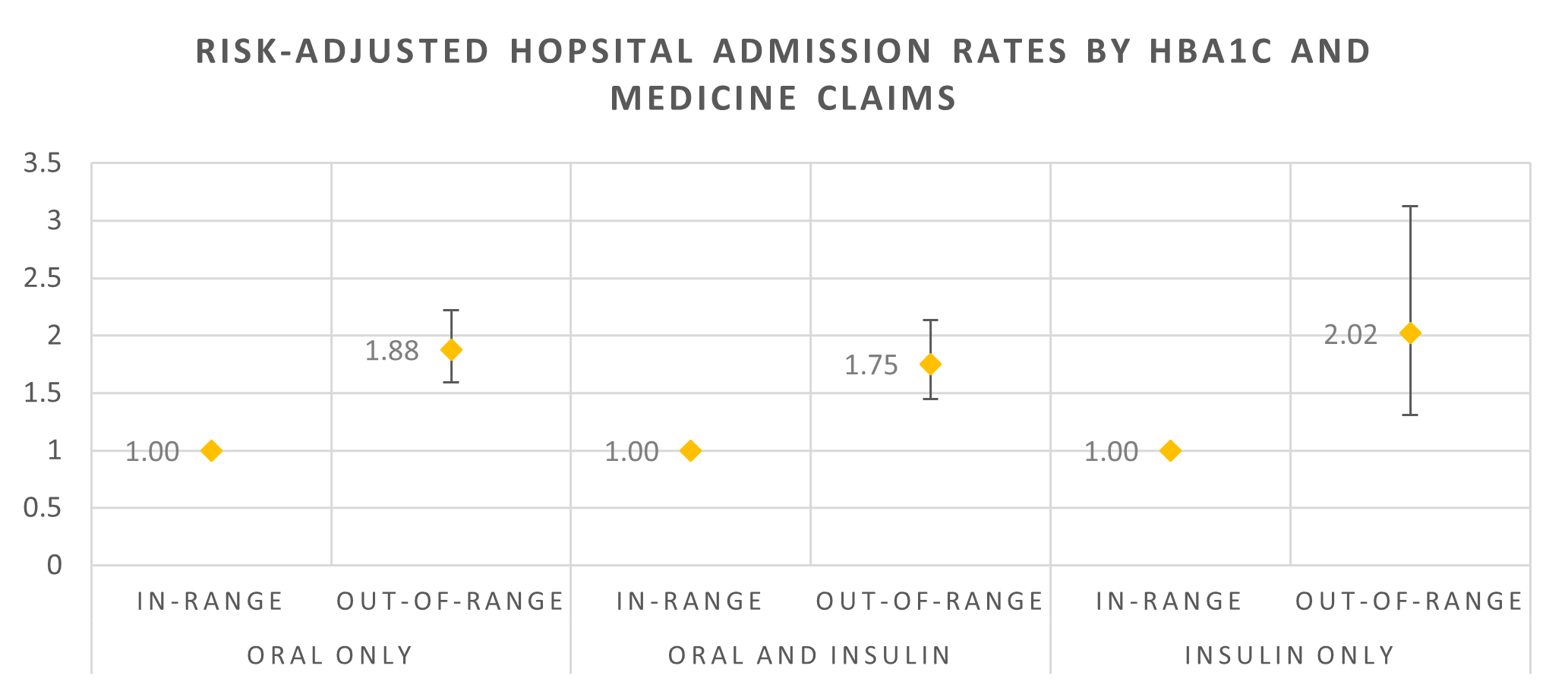
Figure 9: Risk-adjusted odds ratios for COVID-19-related hospital admissions by HbA1c results and medicine claims
*Note: A comparison of risk across different medicine groups cannot be directly drawn from this figure, but rather a comparison of risk relative to in-range members within each medicine group.
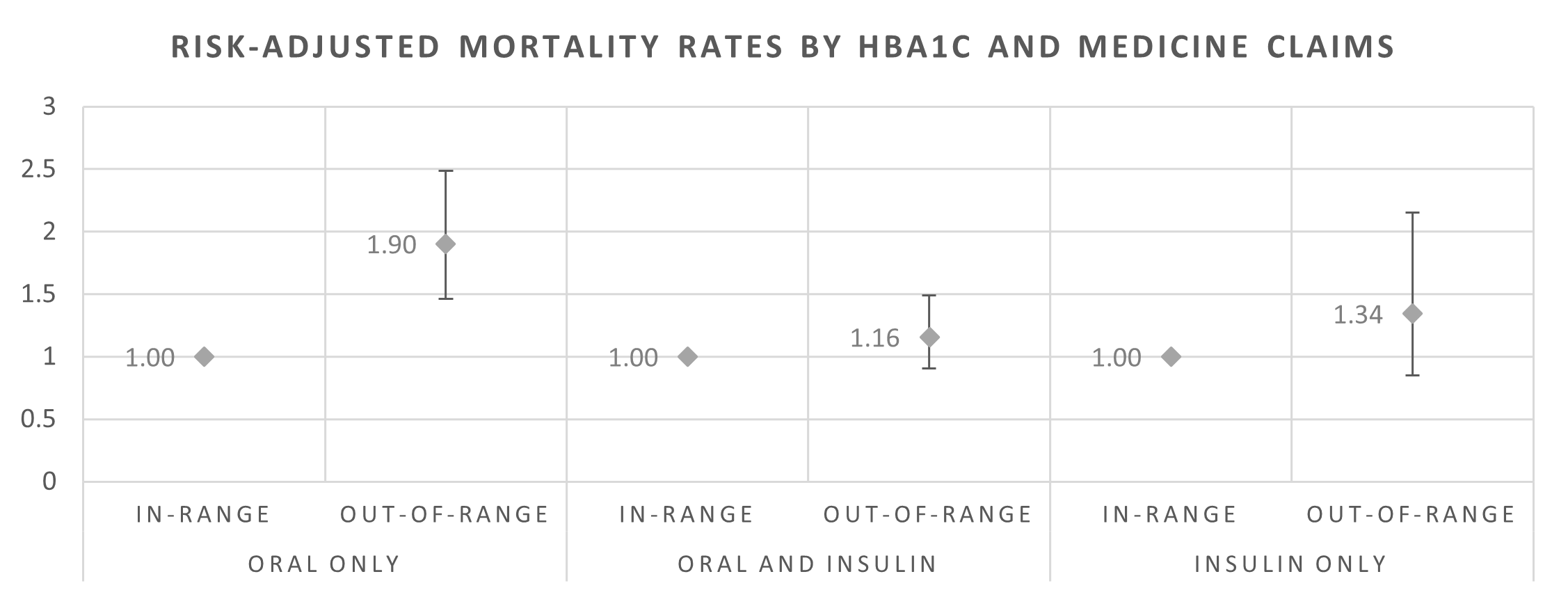
Figure 10: Risk-adjusted odds ratios for COVID-19-related mortality by HbA1c results and medicine claims
*Note: A comparison of risk across different medicine groups cannot be directly drawn from this figure, but rather a comparison of risk relative to in-range members within each medicine group.
Medical scheme members enrolled on Discovery Health's Diabetes Care Programme had more favourable COVID-19 outcomes
What we analysed
The Discovery Health Diabetes Care Programme is offered to members of 11 Discovery Health-administered schemes (all schemes included in this analysis). The programme optimises both their diabetes cover and care. It gives members and Premier Plus GPs access to various tools to manage and monitor the condition to ensure the best outcomes for the member.
The member and healthcare provider can agree on key goals and track their progress on a personalised dashboard on Discovery HealthID (a system for doctors), which shows the member's Diabetes Management Score.
Diabetes Care members also have additional cover for:
- A biokineticist consultation to optimise their approach to physical activity
- An additional consultation with a dietitian to optimise their approach to nutrition
- Additional blood-glucose test strips each year
- A diabetes educator to help the member with their day-to-day diabetes management.
Findings from this analysis
In our sample, 28% of members were enrolled on the Diabetes Care Programme. Compared to those not on the programme, these members:
- Had slightly higher levels of glucose control (44% had an HbA1c result in-range compared with 41% of members not on the programme)
- Had a 12% lower risk of being admitted to hospital for COVID-19 and a 19% lower mortality risk (Figure 11).
- Had lower hospital admission and mortality risks across all medicine claims (Figure 12 and Figure 13).
These results can be explained in part by:
- The higher proportion of members on the programme having in-range HbA1c results
- The programme's holistic approach to diabetes management, and the support and interventions available, which have an impact on a member's lifestyle and behaviour.
That said, further analysis is needed to understand the factors behind these favourable outcomes for programme members. HbA1C results, disease stage and medicine claims alone do not explain why these risks were lower for Diabetes Care programme members.
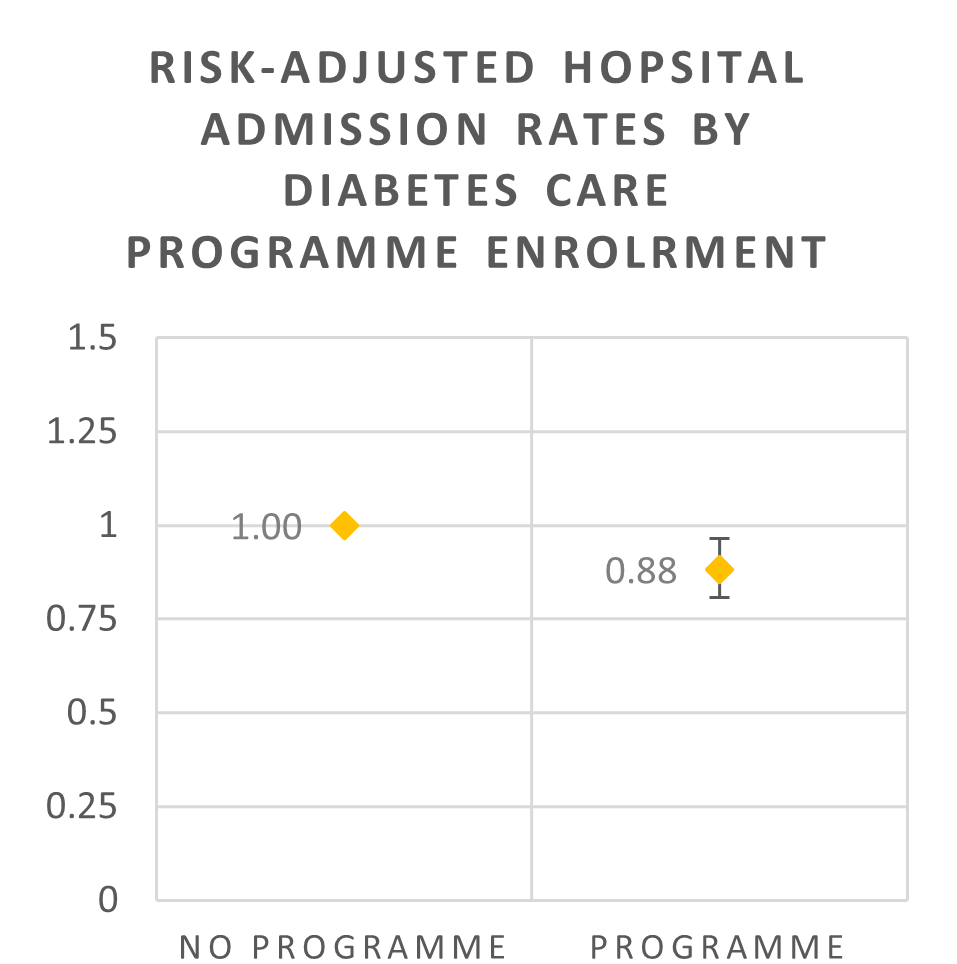
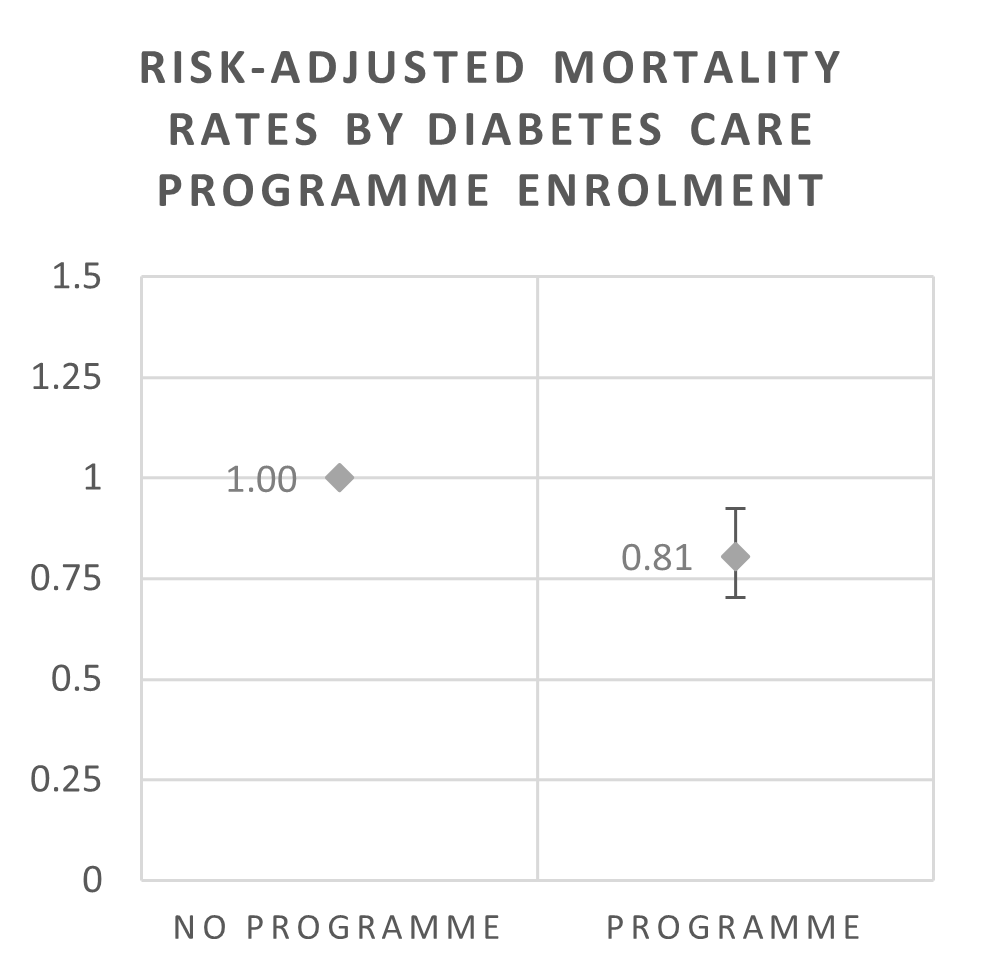
Figure 11: Risk-adjusted odds ratios for COVID-19-related hospital admissions and mortality by enrolment in the Diabetes Care Programme
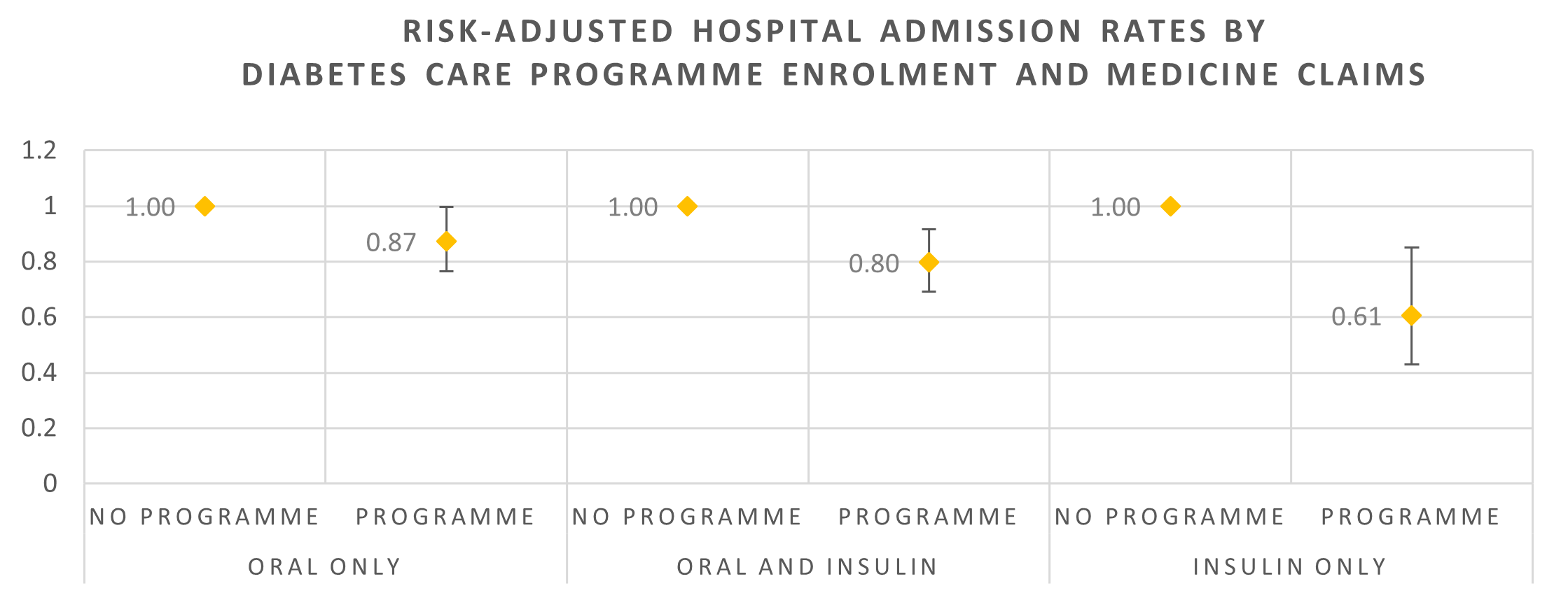
Figure 12: Risk-adjusted odds ratio for COVID-19-related hospital admissions by enrolment in the Diabetes Care Programme and medicine claims
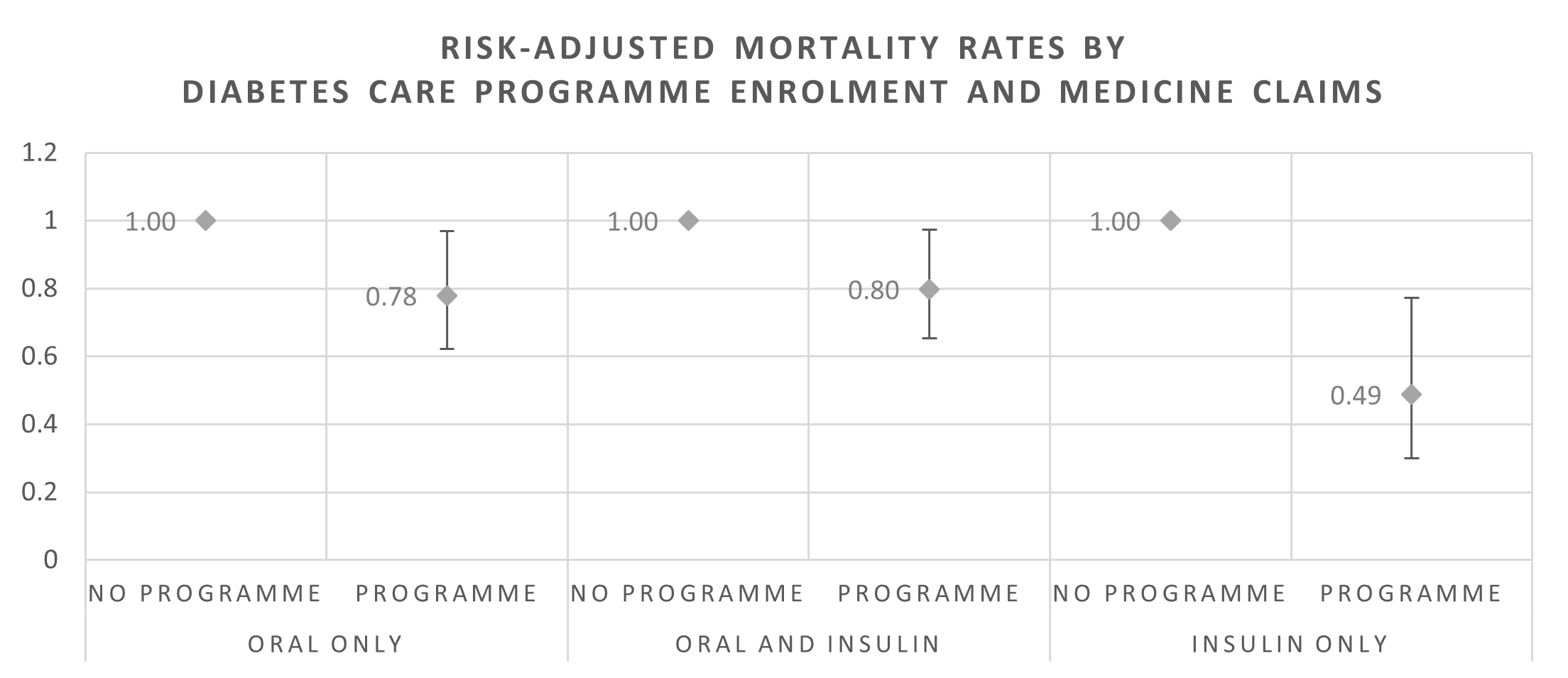
Figure 13: Risk-adjusted odds ratio for COVID-19-related mortality rates by enrolment in the Diabetes Care Programme and medicine claims
Note: Figure 12 and Figure 13 compare the risks of members on the Diabetes Care Programme with those who were not enrolled in the programme by medicine claims made. A comparison of risk across medicine regimes cannot be drawn directly from this figure.
Final thoughts
Our analysis shows a statistically significant relationship between poor glucose control and a higher risk of COVID-19-related hospital admissions and mortality (p <0.0001). This result is dependent on members who had an HbA1c test result, which constituted 47% of the study sample. Further analysis is required to understand the variation in COVID-19 admission and mortality risk across waves and variants. It should also be noted that the data used in this analysis was from medical aid records and was not structured as a clinical trial from the outset.
We also found there is a relationship between COVID-19 outcomes and a member's medicine treatment plan and enrolment on the Diabetes Care Programme. Our analysis showed that members who claimed for insulin only and were not enrolled in the Diabetes Care Programme had a higher risk of serious COVID-19-related outcomes.
All in all, from those members with an HbA1c test result available, those with in-range HbA1c results have better outcomes when they contract COVID-19 than those whose results are out-of-range.
Medical scheme members who have diabetes with diabetic vasculopathy (chronic damage to their small blood vessels) and, who have out-of-range HbA1c results, are at greater risk of more serious outcomes when they get COVID-19. This is probably due the activation of Angiotensin-converting enzyme (ACE) receptors on the blood vessels as this can affect their blood clotting functions which may lead to further damage to their blood vessels and other organs.
These findings strengthen the argument for the importance of well-controlled blood glucose and providing effective care for people with diabetes - particularly during the COVID-19 pandemic. A condition like diabetes can result in serious outcomes when poorly managed and found in combination with COVID-19 disease.
We will soon extend this analysis to cover the period of the Omicron-led fourth wave of infection and the factors driving favourable COVID-19 outcomes for members enrolled on the Diabetes Care Programme.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za for updated data and more information on the context of this analysis.
Did you find this post interesting?
You may also be interested in reading our recent post explaining the results of Discovery Health's at-scale, real-world analysis of the Omicron outbreak (published on 14 December 2021). In collaboration with the South African Medical Research Council (SAMRC), we analysed vaccine effectiveness over the Omicron-led fourth wave of infection.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only the data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.

Discovery Health releases at-scale real-world analysis of Omicron outbreak; including collaboration with the SA Medical Research Council (SAMRC) to analyse vaccine effectiveness
14 December 2021
Discovery Health, South Africa's largest private health insurance administrator, releases at-scale real-world analysis of Omicron outbreak based on 211 000 COVID-19 test results in South Africa, including collaboration with the SA Medical Research Council (SAMRC) to analyse vaccine effectiveness.

Pfizer vaccine's real-world effectiveness in protecting against COVID-19 admission and death in the Discovery Health client population
03 November 2021
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health) and Jared Champion (Senior Actuary, Discovery Health)
Discovery Health's investigation into the Pfizer COVID-19 vaccine's real-world vaccine effectiveness shows a 92% effectiveness in reducing COVID-19 hospital admission risk and 94% effectiveness in preventing the risk of COVID-19 death, between 14 days and 3 months after receiving the second dose.

Comparing severity of Gauteng's first, second and third waves of COVID-19 infection by investigating hospital admission rates
21 July 2021
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health) and Tommy Chen (Actuary, Discovery Health)
The highly transmissible Delta variant has driven an exponential rise in COVID-19 cases in South Africa's third wave of infection, and in Gauteng in particular - the province that is the focus of this analysis. Encouragingly, our initial data shows that compared to the second wave of infection, COVID-19 infections in the third wave are not associated with increased risk of hospital admission.