Discovery Health Activity Index: How has the COVID-19 pandemic shifted health-seeking behaviour for non-COVID-19 healthcare?

Almost 22 months after the discovery of COVID-19, we measure the second-order effects of the impact of this global pandemic. Our data shows the way in which this disease has caused shifts in people's health-seeking behaviour, across a range of non-COVID-19 conditions.
Authors:
Ismail Rasool (Chief Data Officer, Discovery Health) and Jared Champion (Senior Actuary, Discovery Health)
A 33% decline in activity in the healthcare system during Alert Level 5 lockdown
The COVID-19 pandemic has caused disruption across the healthcare spectrum. Discovery Health conducts ongoing analysis into the pandemic's impact on the members of the medical schemes we administer. We do this to understand how their patterns of accessing healthcare have changed since the start of the pandemic - and to respond to the challenges these changes may bring.
Any reduction in access to healthcare poses a risk that scheme members may not access appropriate care when they need it.
At the same time and on the other hand, the restrictions put in place to curb the spread of COVID-19 - that have largely driven the changes in people' accessing of non-COVID-19 healthcare - have also created opportunity for novel ways of accessing and delivering healthcare to gain traction. We also explore this dynamic.
- South Africa went into Alert Level 5 lockdown from midnight 26 March to 30 April 2020. What sort of impact did this have on people's health-seeking behaviour?
Our data shows that during this period, overall activity levels in the healthcare system dropped by 33%. Unpacking this reduction, we see the impact across multiple categories of care and specialities. This article aims to share our insights into the variations in activity we have documented. It also reports on trends we tracked over the course of the pandemic in the following areas:
- Access to general healthcare services
- Access to healthcare services for ear, nose and throat (ENT) conditions; gastrointestinal symptoms; cardiovascular conditions and cancer
- Access to mental healthcare services
Our methodology: Deriving a Health Activity Index
We define a scheme member's 'health activity' as the number of unique encounters they have with the healthcare system each day, such as unique doctor's visits.
We used health activity data dating back to 2019 (pre-pandemic) to set a benchmark against which we could compare activity levels over the course of the COVID-19 pandemic (2020 and 2021).
We adjusted the numbers for relevant demographic factors (such as age, gender, chronic conditions and plan benefits) and applied it to data from 2020 and 2021.
We used our health activity benchmark to compare visits in subsequent years and to derive a Health Activity Index where 1.00 represents the activity baseline set using data from 2019. We adjust this baseline for seasonality patterns and patient risk to ensure accurate monthly measures for tracking.
Our results
Experience over time, taking healthcare access for both COVID-19 and non-COVID-19 care into account
Health Activity Index data shows that in April 2020 (during Alert Level 5 lockdown), activity was at 0.67. This simply means that activity in the healthcare system was down to 67% of levels recorded in April 2019 (as shown in Figure 1). This means that there was a significant drop of 33% in engagement in healthcare in April 2020.
- From this low point in April 2020, the activity levels for the healthcare system increased steadily throughout 2020 and fully recovered to pre-2019 levels by November 2020. The gradual increase in healthcare activity was linked to the first wave peaking in July 2020 and COVID-19 infections tapering off thereafter, allowing non-COVID-19 healthcare access to increase in the months that followed. This was before December 2020 when the second wave of COVID-19 infections began.
- December 2020 saw a 13% higher healthcare activity level (1.13) compared to December 2019. However, this was driven by the second COVID-19 wave of infection, and an increase in COVID-19-related healthcare needs.
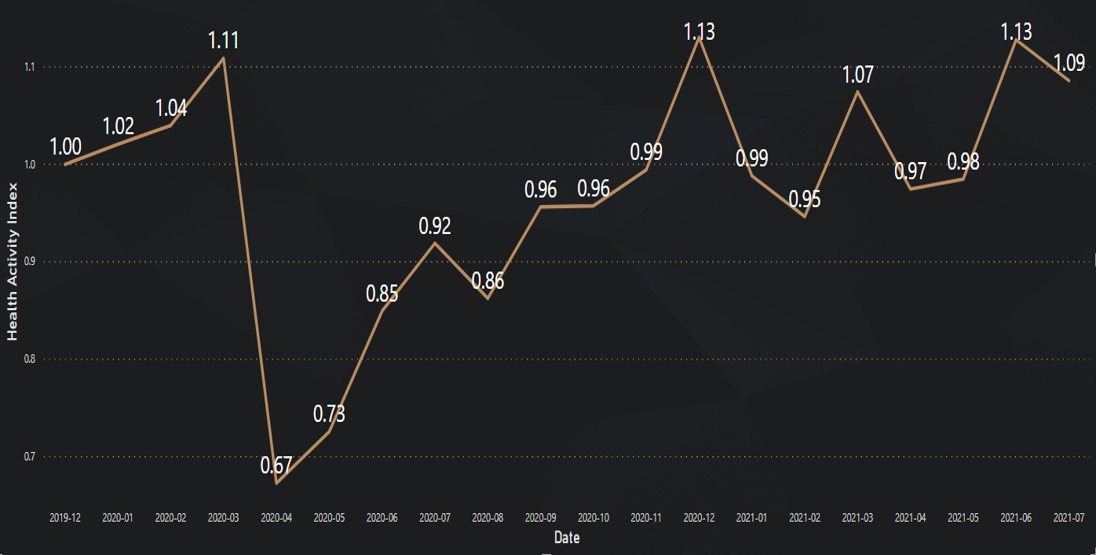
Figure 1: Overall Health Activity Index over time
South Africa experienced a first wave of COVID-19 infection from June 2020 to October 2020 and a second wave of infection from Dec 2020 to February 2021.
- Taking both COVID-19 and non-COVID-19 care into account:
We see a three-fold and six-fold increase respectively in overall healthcare access activity (compared to the same periods in 2019) at the peak of each wave. We also see trough periods at levels 1.5 times the 2019 activity level recorded (Figure 2).
The third wave of infection (from June to September 2021) resulted in a 9.47-fold increase in healthcare activity in July 2021.
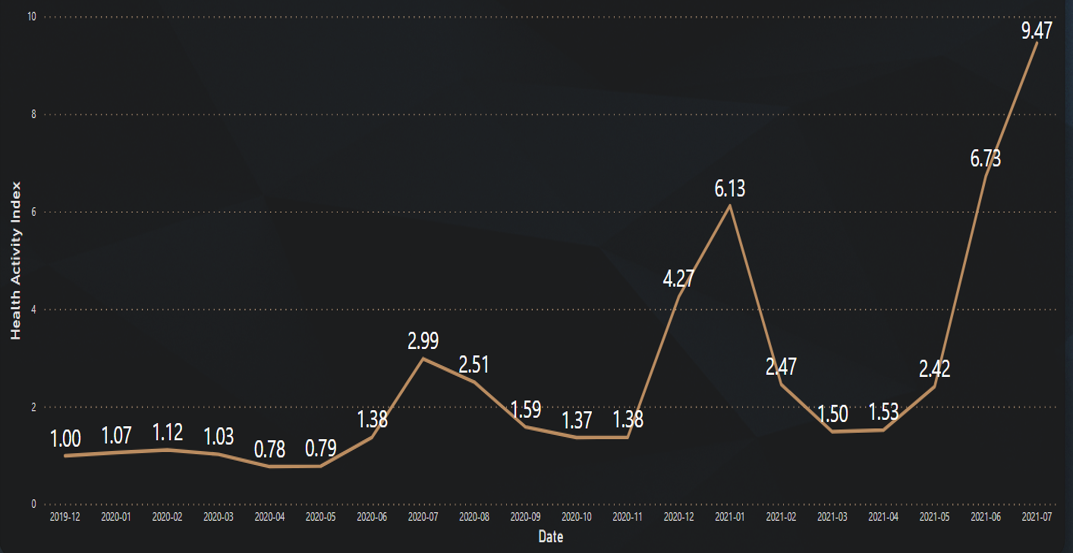
Figure 2: Discovery episode grouper infections (which includes COVID-19 infection) Health Activity Index over time.
Pandemic affects healthcare activity differently across disease categories
We have covered the fact that the lowest point of activity (access to healthcare) across the spectrum was noted during Alert Level 5 (hard lockdown) in April 2020. Figure 3 shows this once more. Looking at specific disease categories, we now note that access to care for ENT (ear, nose and throat) and gastrointestinal conditions decreased significantly (63% and 46% activity decrease respectively) in April 2020. This is when we compare it to access to care for cardiovascular conditions and cancers (17% and 30% activity decrease respectively, in April 2020).
The disease categories in which we see significant decreases (ENT and gastrointestinal) in healthcare activity also show a slower rate of recovery compared to the rate at which healthcare activity resumes for cardiovascular conditions and cancers. The latter fully recovered to baseline expected activity levels by September 2020.
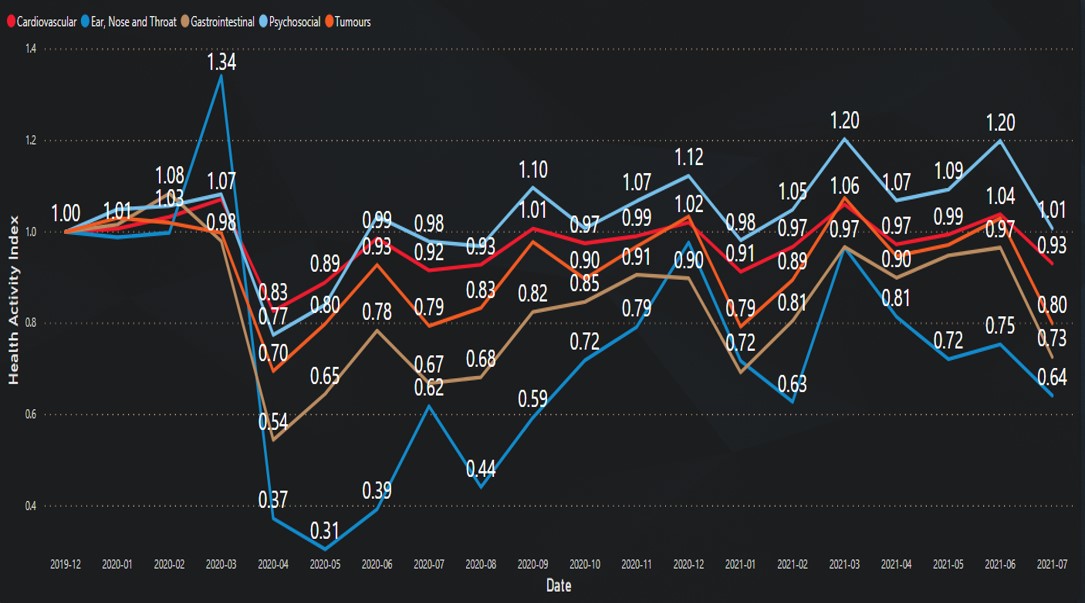
Figure 3: Health Activity Index split by levels of access to care for cardiovascular, ENT (ear, nose and throat), gastrointestinal, psychosocial and cancer conditions
Access to mental healthcare services defies the trends noted for other conditions
In April 2020, within a month of the first recorded case of COVID-19 infection in South Africa (on 5 March 2020), access to mental healthcare services had decreased by 23% (compared to April 2019).
However, levels of access to mental healthcare service had recovered to 2019 activity levels by June 2020. This was by far the quickest recovery seen across conditions considered in our analysis.
From June 2020 to August 2020, mental healthcare activity was close to 2019 levels. However, mental healthcare activity increased significantly above 2019 levels from September 2020 onwards, reaching a noticeable peak activity level (20% increase) in March 2021.
This increase in access to mental healthcare services is most likely explained by (but not limited to) the following pandemic-driven pressures on people's mental health and wellbeing:
- Increased overall mortality rates due to COVID-19
- Direct impact of COVID-19 infection on an individual and their loved ones
- Increased rates of stress and burnout, both for essential workers who were based in the workplace, and for people who found themselves working from home or remotely, for months on end.
Another factor that could possibly be behind the noted increase in access to mental healthcare services, is that mental healthcare services could be accessed through digital channels - so through telemedicine or virtual consultations with healthcare providers. This allowed for continuity of care at a time when mental healthcare services were needed most over the course of the pandemic.
Shifts in patterns of access to healthcare services, in- and out-of-hospital
Scrutiny of the relatively fast pace of recovery of mental healthcare access activity also shows that there has been a clear shift of care from in-hospital services to out-of-hospital services.
Figure 4 shows mental healthcare access activity. Each point represents a certain month from December 2019 to July 2021, split to show in- and out-of-hospital care. The blue lines represent the 2019 activity index. For the time considered, out-of-hospital activity was significantly higher than in 2019 with an observed increase of between 10% and 25%. Most in-hospital mental healthcare activity decreased below 2019 levels (blue line) for all months - it decreased by between 5% and 40%.
April 2020 saw a marked decrease of almost 50% both for in- and out-of-hospital care. This was due to Alert Level 5 lockdown restrictions.
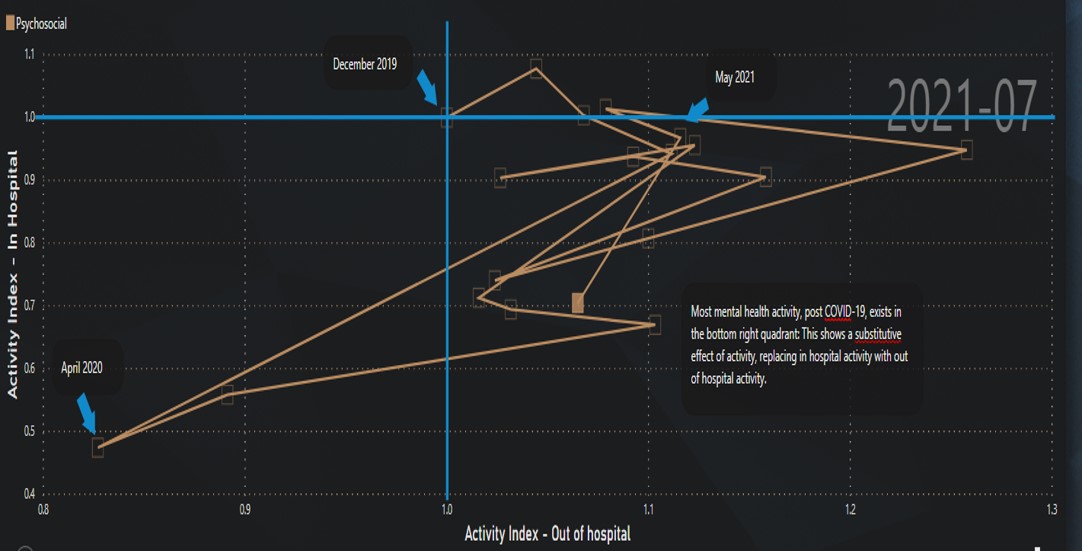
Figure 4: Psychosocial activity rate index for in- and out-of-hospital care over time
Overall, the evidence strongly suggests that over the course of the COVID-19 pandemic, mental healthcare services shifted materially from in-hospital care to out-of-hospital care. Evidence also shows that overall levels of care stayed close to those seen the year before the pandemic (2019) or increased.
- We also noted this switch from in-hospital to out-of-hospital in the case of care for cardiovascular conditions and cancers.
- ENT and gastrointestinal conditions saw no such switch, with levels of healthcare activity decreasing for both in- and out-of-hospital care.
- Maternity and obstetric care saw no level of sustained decrease in either in- or out-of-hospital care compared to 2019 (including out-of-hospital care such as antenatal visits).
Overall, we see three shifts:
- Substitutive activity: Where in-hospital activity was substituted by out-of-hospital activity, as is the case for cardiovascular conditions, cancers and mental health.
- Lost activity: Where both in- and out-of-hospital activity decreased over the course of the COVID-19 pandemic, as is the case for ENT and gastrointestinal conditions.
- Unchanged activity: Where both in- and out-of-hospital activity remained at the same rates seen in 2019, as is the case with access to maternity and obstetric care.
What did the picture look like by the middle of 2021?
In July 2021, activity in the healthcare system was 9% higher than it was in July 2019. However, this activity includes care for COVID-19. Excluding COVID-19 infections, activity in the healthcare system was on average similar to the levels for 2019:
- Out-of-hospital activity is up 6.5% (Table 1).
- In-hospital activity comes down 36%. (As COVID-19 infections increased over the course of the third wave of infection in South Africa, which peaked in July 2021, normal in-hospital activity decreased significantly, showing the impact of the pandemic on non-COVID-19 healthcare).
| July 2021 | Overall | In-hospital care | Out-of-hospital care | |||
|---|---|---|---|---|---|---|
| Health Activity Index | % change | Health Activity Index | % change | Health Activity Index | % change | |
| Overall | 1.09 | 8.6% | 1.04 | 3.6% | 1.10 | 9.6% |
| Overall (excluding infections) | 1.00 | -0.2% | 0.64 | -36.0% | 1.06 | 6.5% |
| Condition | ||||||
| Trauma | 0.70 | -30.1% | 0.74 | -26.2% | 0.66 | -33.6% |
| Mental health | 1.01 | 0.8% | 0.68 | -31.5% | 1.06 | 6.5% |
| Provider | ||||||
| GP | - | - | - | - | 1.09 | 9.4% |
| Pharmacy | - | - | - | - | 1.12 | 12.1% |
| Chronic | - | - | - | - | 0.97 | -2.5% |
| Acute | - | - | - | - | 1.33 | 32.9% |
| Pathology | 1.46 | 45.9% | 1.10 | 9.5% | 1.70 | 69.6% |
| Radiology | 0.87 | -13.1% | 0.95 | -4.7% | 0.82 | -18.1% |
Table 1: Health Activity Index and % change across different conditions and healthcare providers split by in- and out-of-hospital care
Looking at trends and activity levels by discipline:
- Both pharmacies and general practitioners experienced increased activity levels compared to 2019 with acute medicine up 32.9%. This is most likely due to increased use of acute medicine to treat COVID-19 infection.
- Pathology activity - clearly due to COVID-19 testing demand - is at significantly higher (69.6%) levels.
- Radiology is, however, at 18.1% lower than 2019 levels due to lower levels of hospital admissions (tightly linked to radiology usage).
Final thoughts
COVID-19 has brought about significant change in the way in which we access healthcare, both to treat COVID-19 disease and other healthcare conditions.
Our analysis shows varying impact on access to care according to the condition considered - with two trends noted:
- Substituting in-hospital with out-of-hospital activity for vital services, such as cardiovascular and oncology care. This ensured medical scheme members received necessary care at times when hospitals were predominantly focused on managing COVID-19.
- Increase in mental healthcare demand, mostly due to the impact of the COVID-19 pandemic and leveraging the option to access this care in a virtual, out-of-hospital setting.
We must still see whether these two trends will continue into the future. While these activity trends provide some insight into the changing landscape of healthcare access, work still needs to be done to understand how pandemic-driven disruptions to healthcare access will affect medium- to long-term quality of care outcomes.
We hope that the substitutive out-of-hospital care noted was qualitatively sufficient to make up for any lost overall activity or decreased access to healthcare, and that the lower-than-expected activity will not lead to any long-term adverse effects on the member population of Discovery Health administered medical schemes.
We will continue to monitor the recovery of healthcare activity and report back on our findings in due course.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and any further context required.
Did you find this post useful?
You may also be interested in reading our recent post on the Pfizer-BioNtech COVID-19 vaccine's real-world effectiveness in protecting against COVID-19 admission and mortality in the Discovery Health client population. This report on the protective effects of COVID 19 vaccination follows a massive analysis of millions of data points across the comprehensive wellness, healthcare and vaccine data encompassing 2,1 million adult scheme members, administered by Discovery Health.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only the data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.

Pfizer vaccine's real-world effectiveness in protecting against COVID-19 admission and death in the Discovery Health client population
03 November 2021
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health) and Jared Champion (Senior Actuary, Discovery Health)
Discovery Health's investigation into the Pfizer COVID-19 vaccine's real-world vaccine effectiveness shows a 92% effectiveness in reducing COVID-19 hospital admission risk and 94% effectiveness in preventing the risk of COVID-19 death, between 14 days and 3 months after receiving the second dose.

Super immunity? Discovery Health data analysis shows 98% drop in risk of COVID admission for people who have both recovered from COVID-19 and who are fully vaccinated (Pfizer two-dose vaccine)
03 November 2021
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health) and Jared Champion (Senior Actuary, Discovery Health)
Discovery Health's investigation into the Pfizer COVID-19 vaccine's real-world effectiveness takes a closer look at the impact of full vaccination on those who have recovered from COVID-19. Our investigation shows that for people in this group, the absolute risk of COVID-19 admission is reduced by 98%.

Getting COVID-19 puts a person at equal or much higher risk of adverse events than COVID-19 vaccination
03 November 2021
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health), Lizelle Steenkamp (Head of Risk Intelligence, Discovery Health) and Jared Champion (Senior Actuary, Discovery Health), Tommy Chen (Actuary, Discovery Health)
Discovery Health's investigation into the risk of adverse events, either following COVID-19 vaccination or when infected with COVID-19 disease. We show that contracting COVID-19 carries the highest risk by far, of experiencing adverse conditions.