How have admission rates for five common surgery and diagnostic procedures changed over the past year?

During the COVID-19 pandemic, many elective procedures were deferred. Have rates of these procedures returned to pre-COVID levels yet? We look at changes in admission rates for five high-volume, common surgeries and diagnostic procedures from 2022 to 2023, and share fascinating results and insights.
Authors
Karl Bernhardt (Actuarial Analyst, Discovery Health), Lara Wayburne (Senior Actuary, Discovery Health), Shirley Collie (Chief Research Actuary, Discovery Health)
Recapping our first analysis of shifts in high-volume elective procedure utilisation trends
We previously investigated healthcare utilisation trends from 2019 to June 2022 with a focus on five high volume elective procedures:
- Spinal surgeries
- Cataract surgeries
- Tonsillectomies and adenoidectomies
- Endoscopies
- Cardiac catheterisations (angiograms)
That analysis showed that the COVID-19 pandemic had varying impacts on the way patients and healthcare providers approached different elective surgeries and diagnostic procedures.
A recap of findings from that research:
Relative to 2019 (pre-COVID levels) -
- Admissions for spinal surgery reduced by 11% in 2020 and 8% in 2021. By 2022, admissions had increased by 8%.
- Admissions for cataract surgery reduced by 20% in 2020 but showed strong recovery in 2021, with a marginal decrease of just 4% in 2021. By 2022, admissions had increased by 11%.
- There was a 60% reduction in tonsillectomies and adenoidectomies in 2020 and 46% reduction in 2021, with some recovery in 2022 (14% reduction relative to 2019 rates).
- Endoscopies were down 27% in 2020, 19% in 2021, and had returned to pre-COVID levels in 2022.
- There was a 28% reduction in admissions for cardiac catheterisations (angiograms) over 2020 and 2021. However, the rate of strokes and heart attacks reduced by 21% over 2020 and 2021 in comparison to 2019 (pre-COVID) levels. The drop in invasive angiograms over 2020 and 2021 wasn't paralleled by an (expected) increase in strokes or heart attacks. At the same time, we saw more Computed Tomography Coronary Angiography (CTCA) (non-invasive) take place. This dynamic called into question whether angiograms should be as routine as they are for patients at risk of coronary artery disease or whether patients (low-to medium-risk) could be allocated to CTCA screening more often, where appropriate.
Examining utilisation rates for the same procedures from June 2022 to June 2023
Generally speaking, healthcare system utilisation increased post removal of all restrictions relating to the COVID-19 pandemic. In the next leg of this research, we set out to:
- Examine how admission trends for the same five high volume elective procedures changed from June 2022 to June 2023
- Understand the underlying factors influencing utilisation changes for each procedure.
Our data is based on procedure claims submitted by 3.2 million members of medical schemes administered by Discovery Health and on the latest available data for hospital admissions (through authorisations).
We have focused on the period up to end June of each year (year-to-date or 'YTD', to allow for the seasonal variation in hospital admissions).
Once again, we refer to pre-pandemic levels as the 2019 experience. In some instances, the methodology used to calculate the figures has been updated and therefore some figures might appear different to those previously reported, however all trends have remained consistent.
Our findings: Utilisation trends from June 2022 to June 2023
(a) Two kinds of spinal admissions
- Spinal surgeries
Spinal surgeries experienced a relatively low reduction in volumes during 2020 and 2021 and returned to normal levels relatively quickly during 2022. Admissions for spinal surgeries reduced by 13% in 2020 and 12% in 2021 (compared to 2019 levels). We also observed a decrease in conservative care throughout 2020 and 2021, the initial two years of the COVID-19 pandemic. During this time, there was less utilisation of out-of-hospital physiotherapy, chiropractic, and GP services prior to surgical spinal admissions.
Spinal surgery admissions increased by 7% above 2019 levels in 2022 (1.6% increase per annum) and 13% above 2019 levels in 2023. The 2023 level is equivalent to a 3.2% per annum increase in admissions (Figure 1).
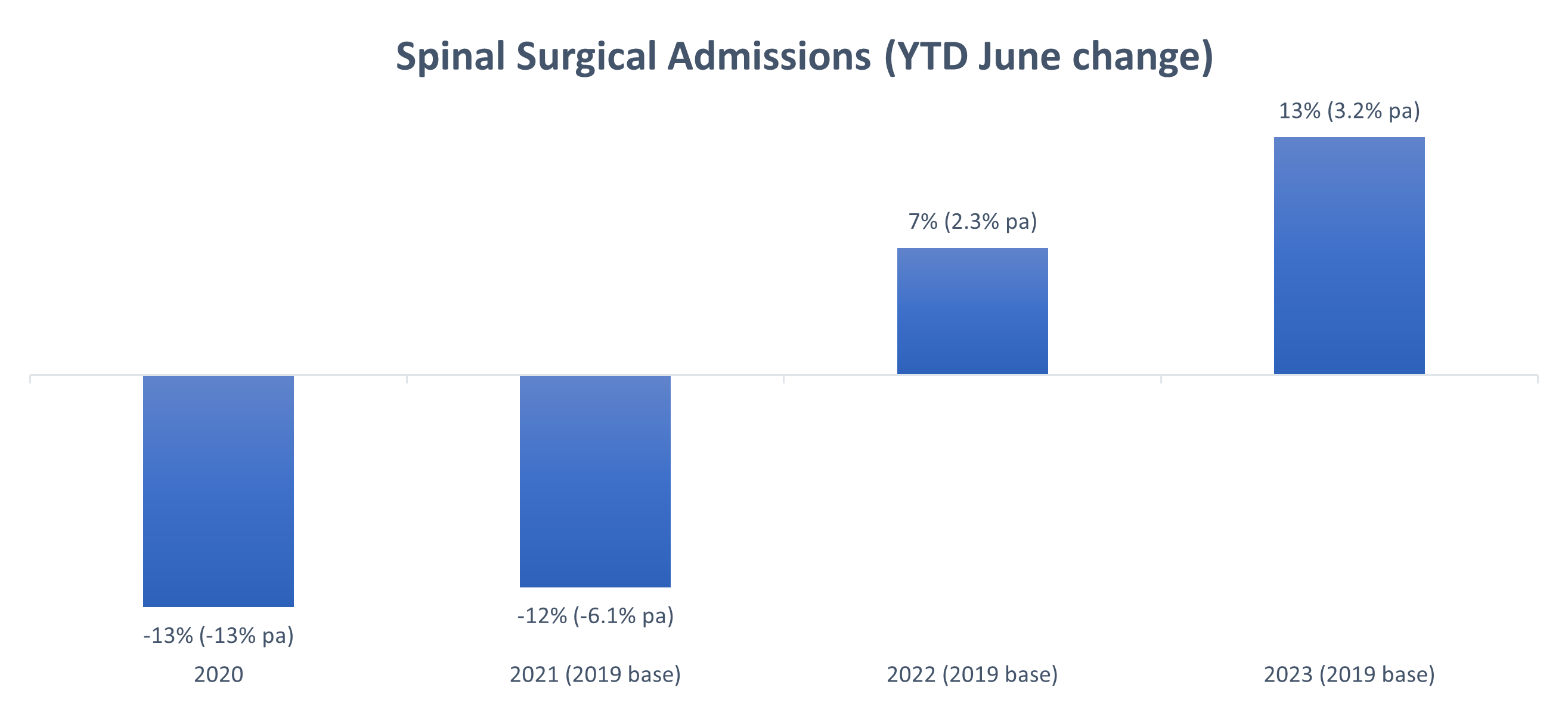
Figure 1: Admission rates for spinal surgeries where the 0% baseline indicates 2019 or (pre-COVID) utilisation rates.
- Spinal medical admissions
Compared to admissions for spinal surgery, spinal medical admissions (admissions for medical back pain management, including epidural injections) showed a larger decrease in volume during the 2020 to 2022 (COVID-19) period. The largest reduction occurred in 2021 with a 35% drop. Since 2021, admissions have significantly increased, with YTD June 2023 figures at 11% (2.6% per annum) above 2019 rates (Figure 2).
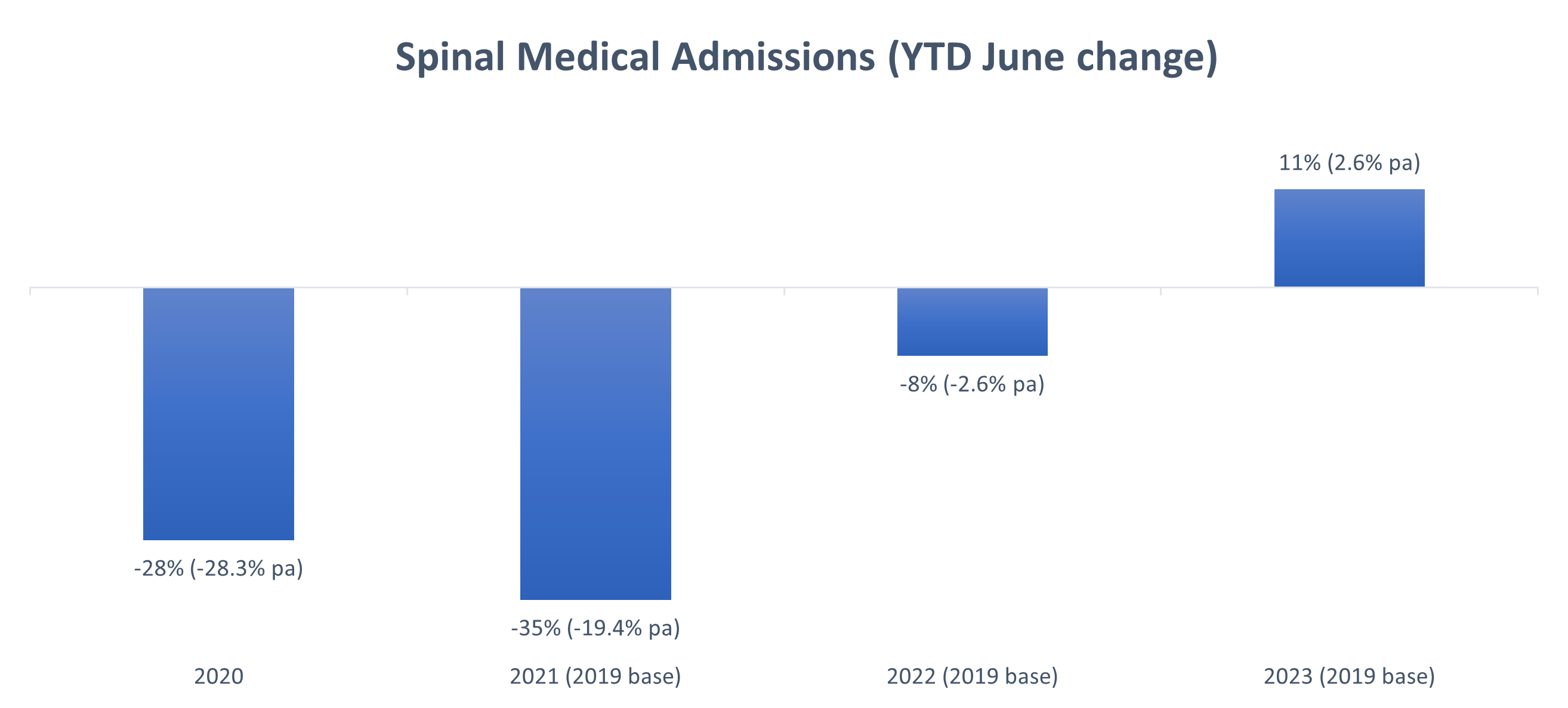
Figure 2: Admission rates for spinal medical admissions where the 0% baseline indicates 2019 (or pre-COVID) utilisation rates.
Cataract surgeries
By 2022, cataract surgery rates had returned to and exceeded pre-pandemic levels.
Admissions for cataract surgeries reduced by more than spinal surgeries (which reduced 13%) during the first year of the pandemic - a reduction of 26% in 2020.
Admissions increased quickly post 2021, with 2022 and 2023 levels surpassing 2019 levels by 6% and 12% respectively. Overall, the rate of cataract surgeries has increased by 2.9% per annum since 2019, indicating a continued increase in the demand for these procedures (Figure 3).
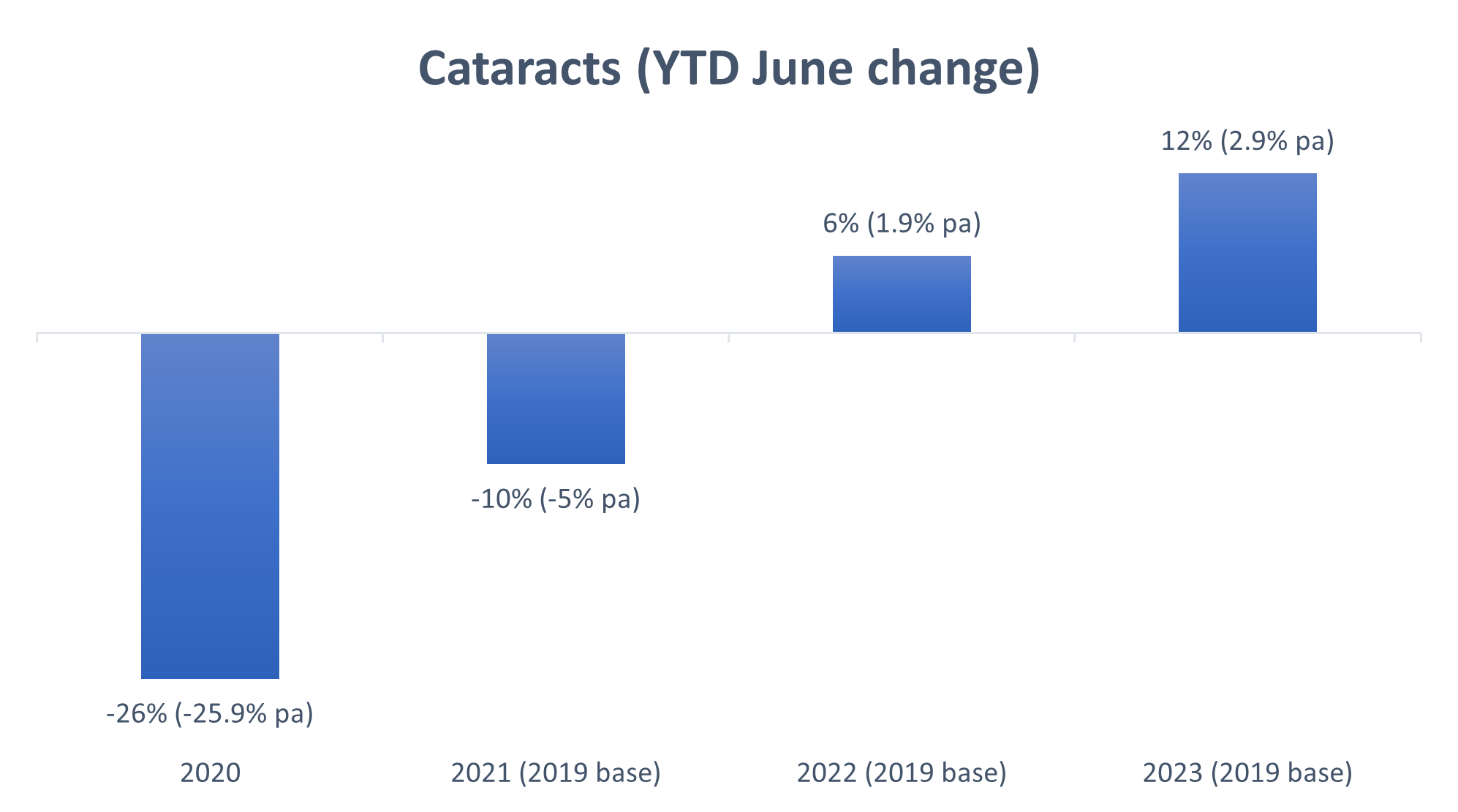
Figure 3: Admission rates for cataract surgeries where the 0% baseline indicates 2019 (or pre-COVID) utilisation rates.
As members of medical schemes administered by Discovery Health grow older (the Scheme population ages yearly), we do expect cataract surgery volumes to increase year-on-year.
However, the increase in cataract surgeries noted in our research exceeds what is attributable to an ageing member population. We investigated the average age of members having surgeries post the pandemic period to see if members were having surgeries that had been postponed due to COVID-19.
- Since 2012, so for the past 10 years, the average age of members going for cataract surgery has consistently been at above 67.5 years.
- The only exception was in 2020 (the first year of the COVID-19 pandemic), when this dropped to 67.2 years.
- In 2019 (pre-COVID), the average age at which people had cataract surgery was 67.8.
- In 2021, it was 67.7 years of age.
- In 2022 it was 68.1 years of age.
- In 2023 it was 67 years of age.
This suggests that cataract surgeries were in fact delayed due to the COVID-19 pandemic, by between four to 11 months on average (Figure 4).
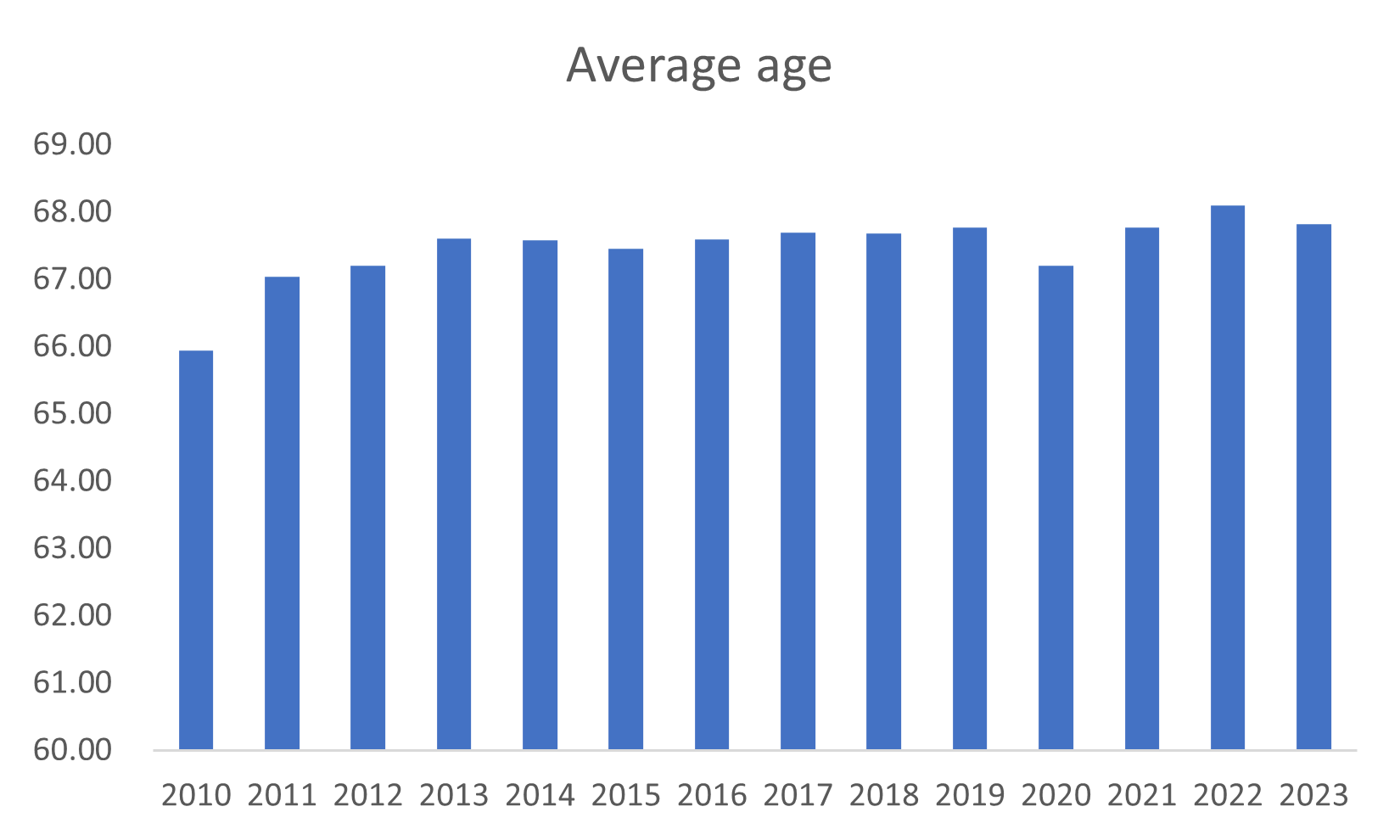
Figure 4: Average age of members undergoing cataract surgery year-on-year, between 2010 and 2023.
In 2020, the average age of those having cataract surgery dropped from 67.3 years to 65.2 years in April, at the onset of the pandemic.
The average increased over the course of the year suggesting that older lives were more likely to postpone or cancel surgery (Figure 5).
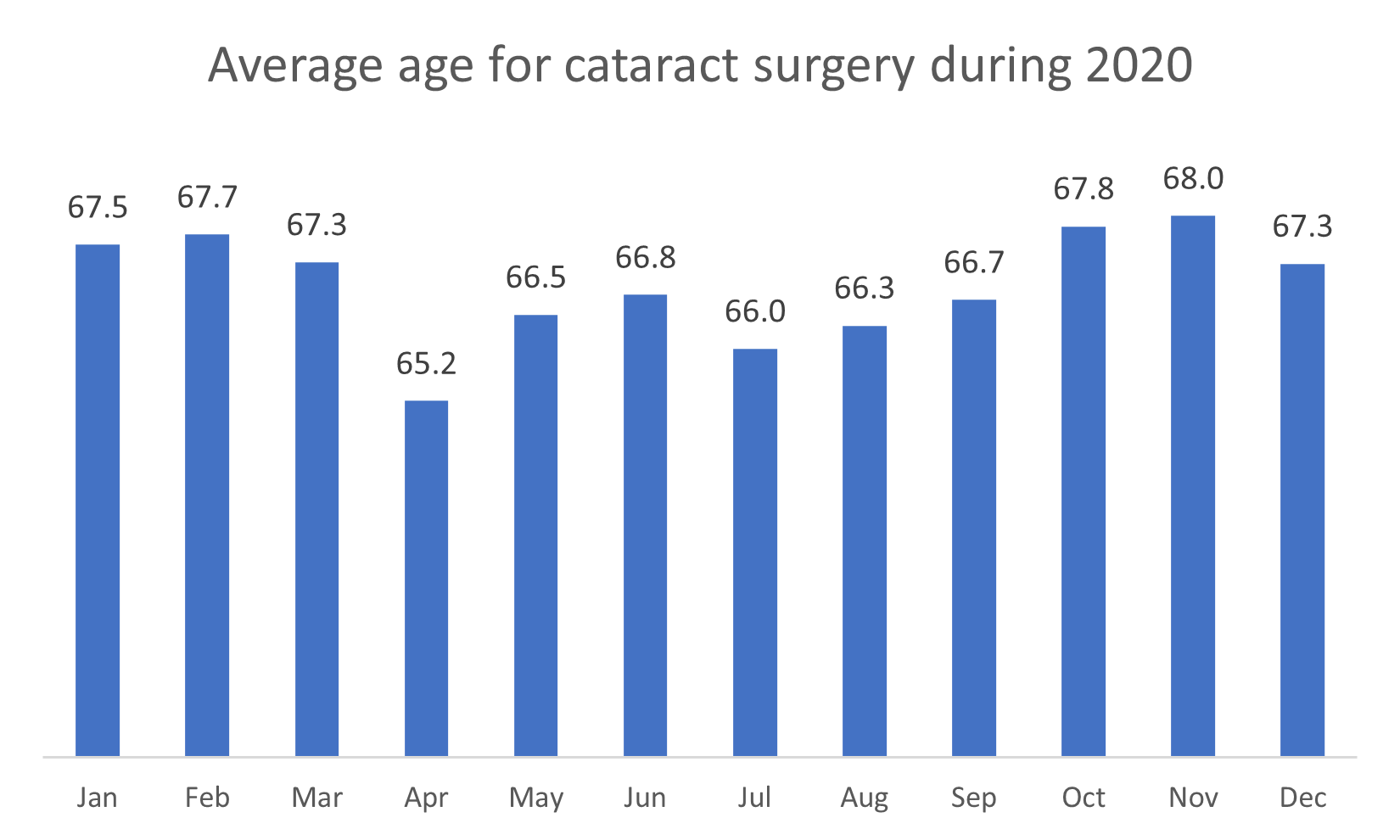
Figure 5: Average age of members undergoing cataract surgery through 2020.
Tonsillectomies and adenoidectomies
Of the five procedures analysed, tonsillectomies and adenoidectomies had the largest reduction in utilisation over 2020 and 2021 - a 51% reduction. This trend continued late into 2021. However, as social circumstances began returning to pre-pandemic norms, utilisation began to recover in 2022 but at lower levels than those recorded in 2019. By end June 2023, admissions for tonsillectomies and adenoidectomies recovered to only 2% below 2019 levels (Figure 6).
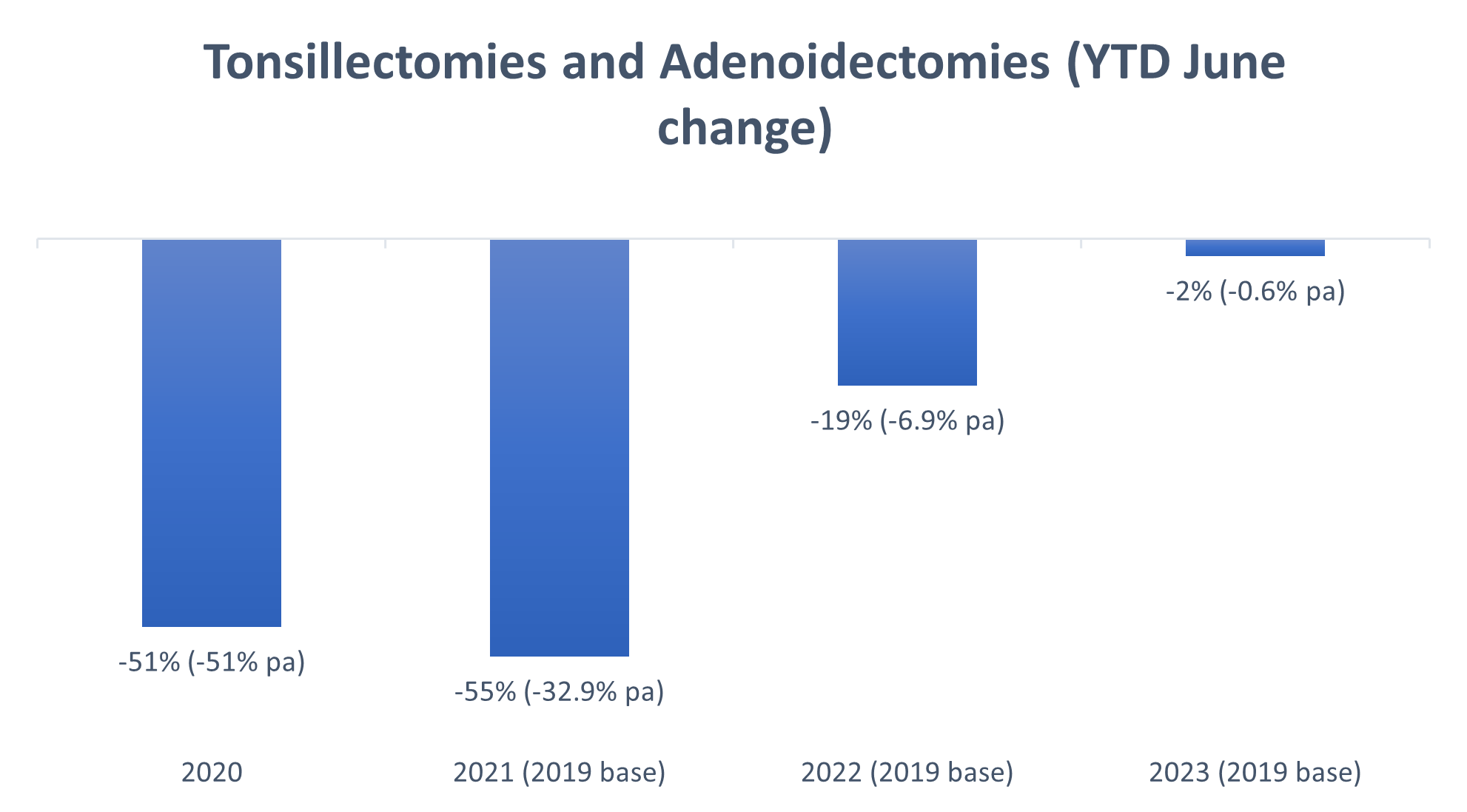
Figure 6: Admission rates for tonsillectomies and adenoidectomies in 2020, 2021, 2022 and early 2023. The 0% baseline indicates 2019 levels, pre-COVID-19.
Endoscopies
Diagnostic and screening procedures were also severely impacted over the course of the COVID-19 pandemic. Of course, this raises concerns about the long-term consequences of medical scheme members not getting either the diagnoses or medical care they need, on time.
For endoscopies, there was a more obvious reduction in the hospital and day clinic setting, compared to endoscopies performed in doctors' rooms. This reflects both people's reluctance to go to healthcare facilities for fear of contracting COVID-19 over the course of the pandemic, and the prioritisation of COVID-related care in hospitals over the course of the pandemic.
Interestingly even into 2023 more endoscopies are being done in doctors' rooms and day clinics compared to acute facilities.
We see that the return to pre-COVID-19 endoscopy levels has been gradual with admission rates remaining suppressed throughout 2021. Pre-COVID-19 levels were only surpassed early in 2022 as some deferred procedures were caught up and new procedures carried out.
Most endoscopies performed in 2022 were new procedures as several endoscopies that were cancelled in 2020 may no longer have been required in 2022. This could be due to members experiencing an improvement or resolution of symptoms or having sought alternative forms of care.
By end June 2023, the utilisation of scopes had surpassed 2022 and 2019 levels with an overall increase of 10% over the four-year period, or 2.4% per annum since 2019. However, the rate of recovery has varied according to endoscopy type. In 2023, gastroscopies were still below 2019 rates. The largest increase has been observed for bi-directional endoscopies, with an increase of 26.1% compared to 2019.
We are seeing an increasing preference for bi-directional scopes, with a corresponding reduction in uni-directional scopes - gastroscopies and colonoscopies (Figure 7).
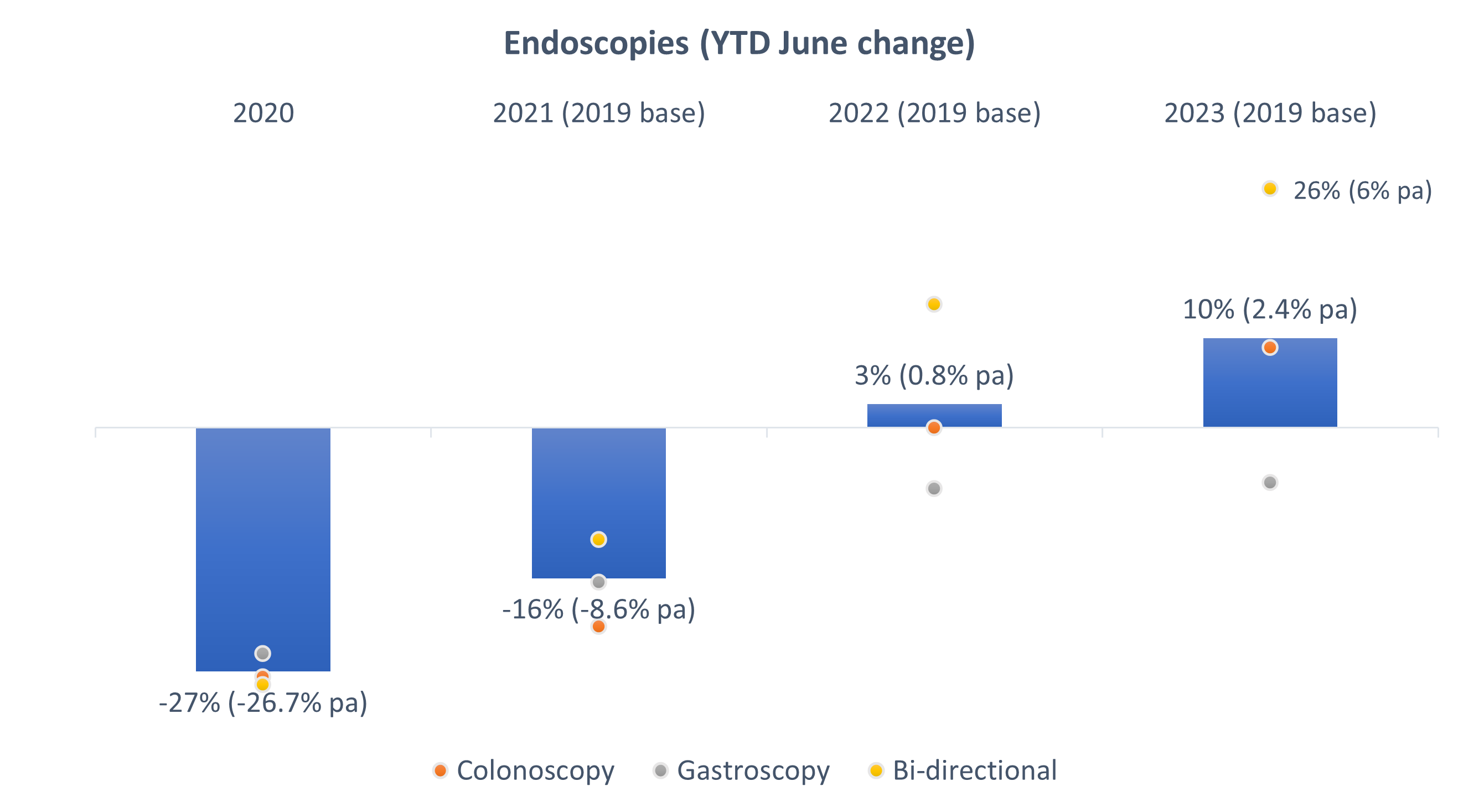
Figure 7: Admission rates for endoscopies in 2020, 2021, 2022 and 2023. The 0% baseline indicates 2019 levels, pre-COVID-19.
Cardiac catheterisations (angiograms)
Looking at claims data for all medical schemes administered by Discovery Health, we see a 23% reduction in admissions for cardiac catheterisations over the past two years, once again relative to pre-COVID-19 levels (Figure 8).
In our previous article, we explored the alternatives for cardiac catheterisation admissions. This included the clinical recommendations for less invasive interventions, such as computed tomography coronary angiographies (CTCAs), for patients with low- to intermediate-risk of cardiovascular disease.
Our data show that utilisation of CTCAs increased over the COVID-19 period (a 44% increase in 2021, from 2019). And, the latest June 2023 year-to-date data show just over a tripling of CTCA utilisation rates relative to the corresponding year-to-date period in 2019 - which corresponds to a 218% increase (Figure 9).
We used the incidence of strokes and acute myocardial infarctions (heart attacks) to determine whether patients deteriorated because they were not accessing cardiac catheterisations over the past two years.
Our data show that the rate of strokes and heart attacks actually reduced by approximately 21% and 13% respectively over 2020 and 2021 in comparison to 2019 levels. Then rates rose again in 2022 and 2023, to levels experienced before the COVID-19 pandemic (Figures 10 and 11).
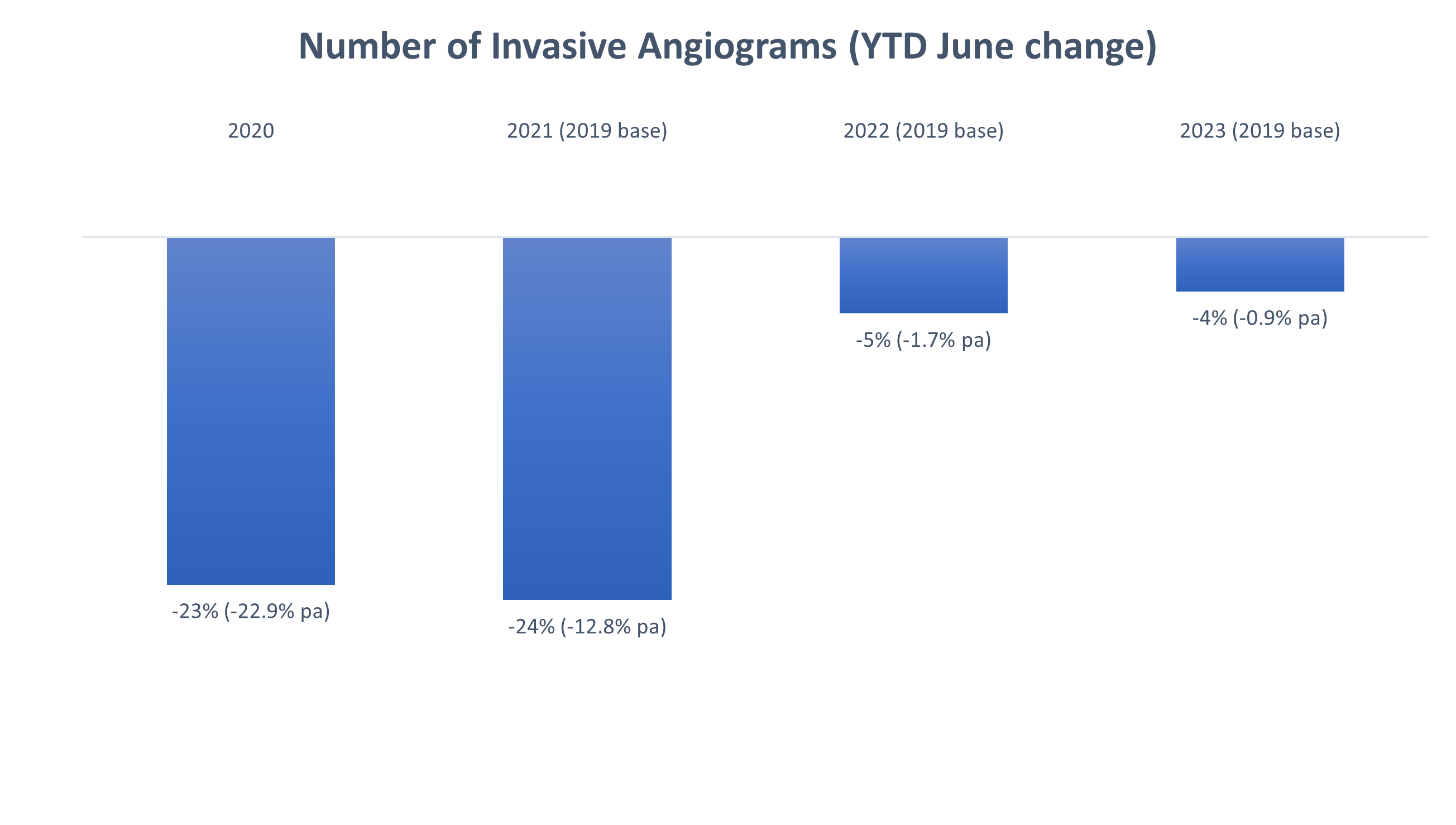
Figure 8: Reduction in admission rates for invasive angiograms from 2019-2020, 2019-2021, 2019-2022 and 2019-2023.
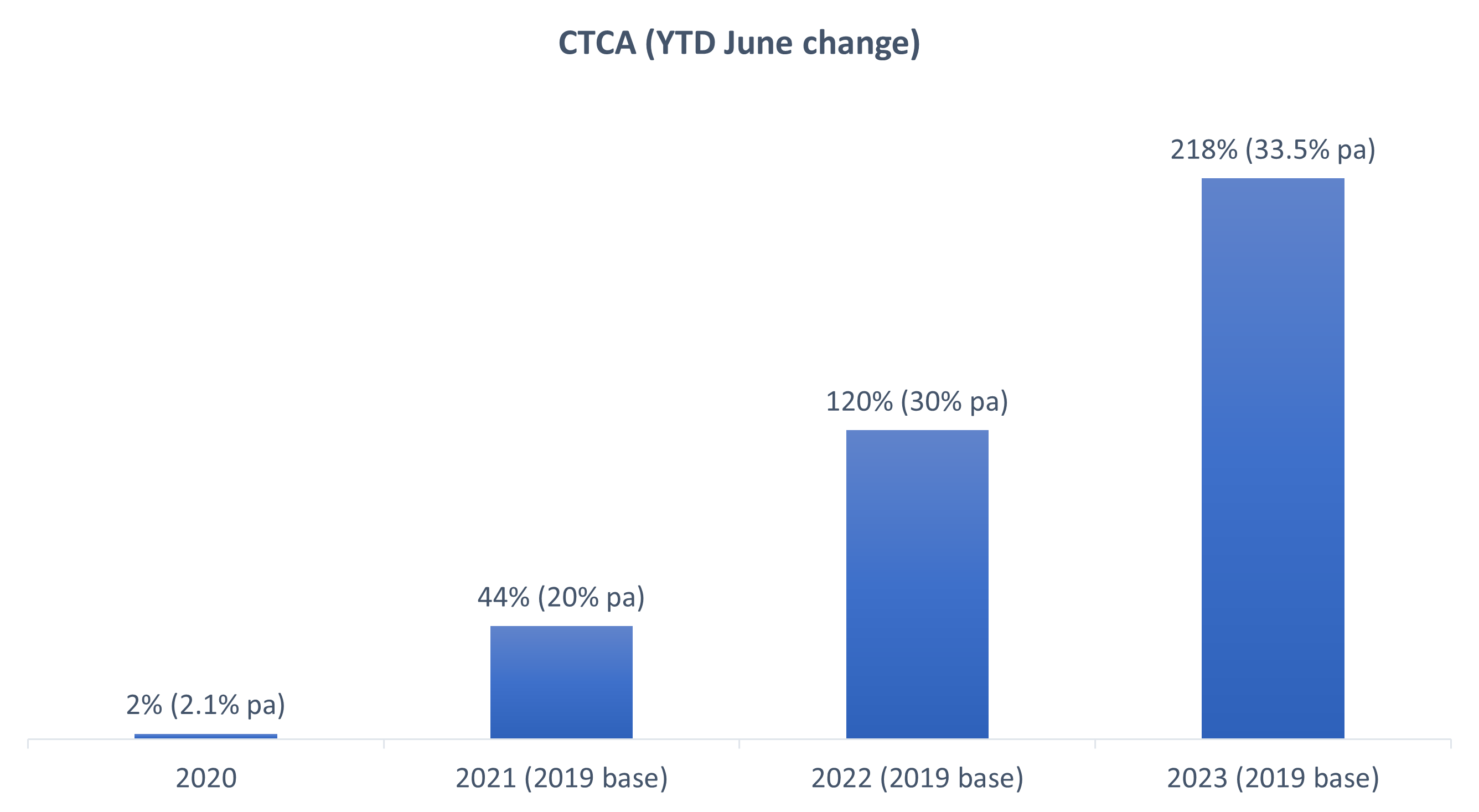
Figure 9: Increase in CTCAs over 2020, 2021, 2022 and 2023 (compared to 2019). The 0% baseline indicates 2019 levels, pre-COVID-19.
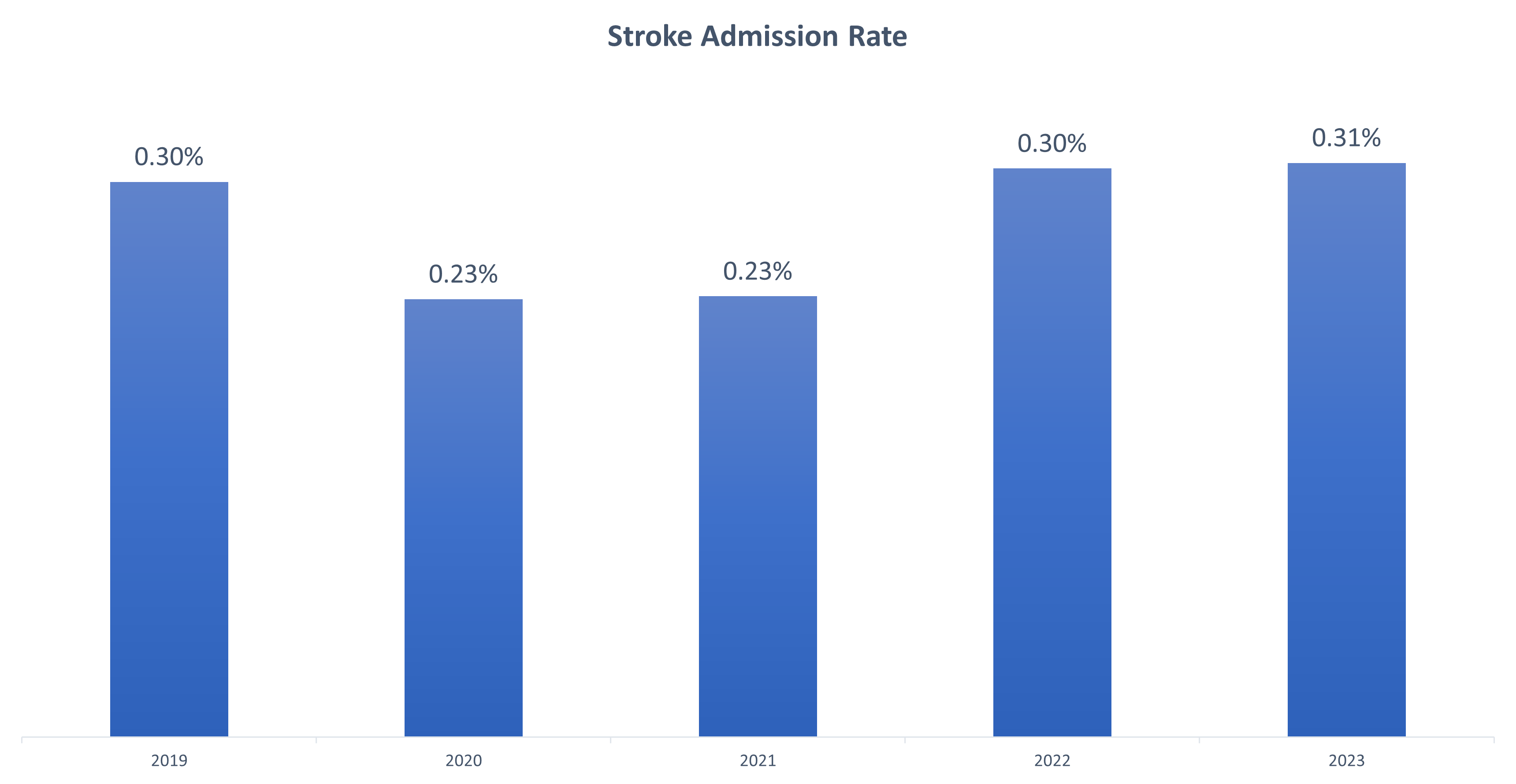
Figure 10: Admissions to treat strokes over 2020, 2021, 2022 and 2023 (compared to 2019 baseline).
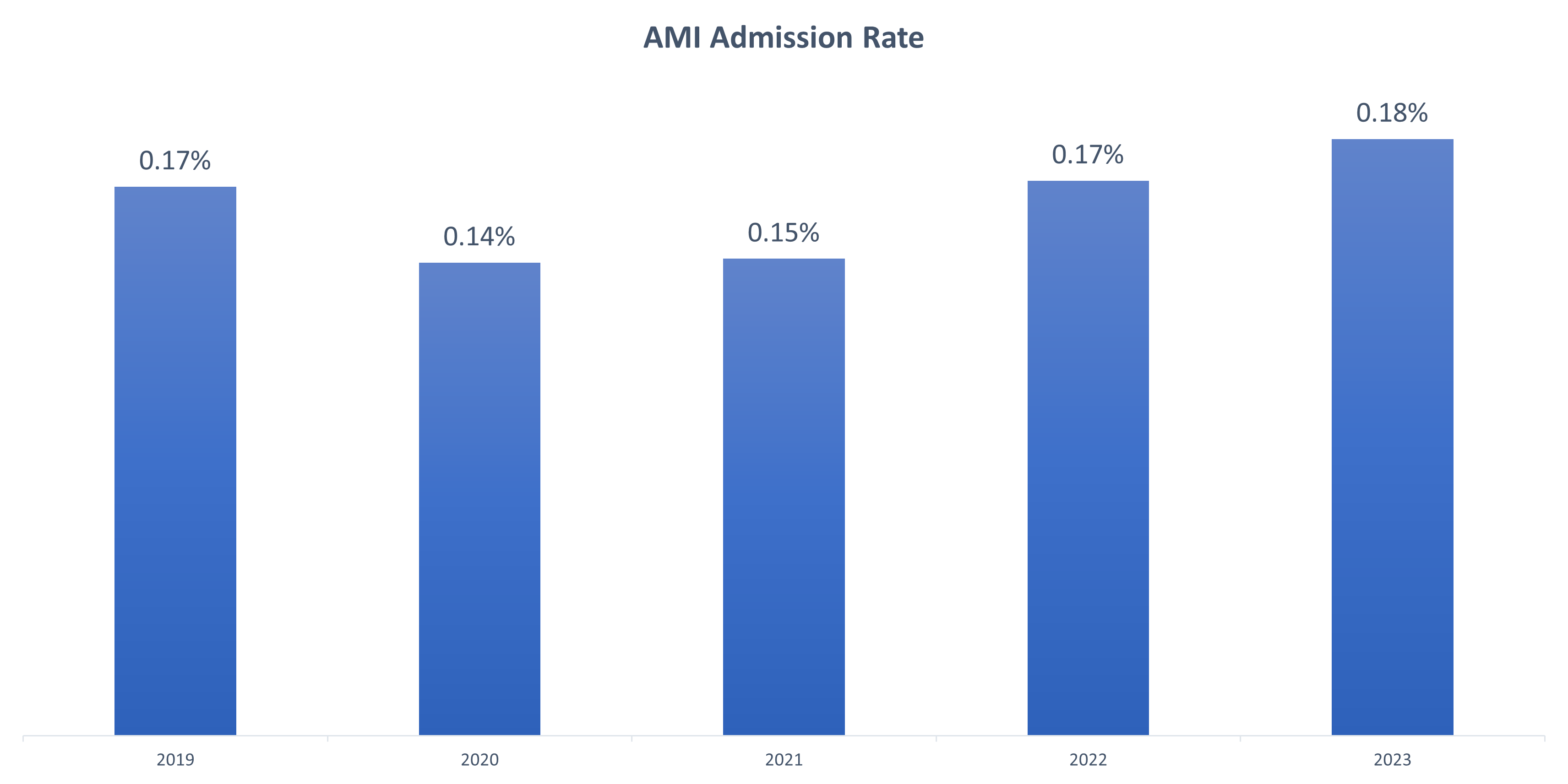
Figure 11: Acute Myocardial Infarction (AMI or heart attack) admission rate over 2020, 2021, 2022 and 2023 (compared to 2019).
Discussion and conclusion
The COVID-19 pandemic changed the way patients and healthcare providers approached elective surgeries and diagnostic procedures.
We've summarised the trends for each medical intervention according to the disruptive impact of COVID-19, how quickly utilisation reverted to pre-pandemic levels, and how utilisation rates in 2023 compare to pre-pandemic levels
|
Medical intervention |
COVID-19 utilisation disruption impact |
Speed of utilisation reversion |
2023 utilisation levels vs pre-pandemic |
|
Spinal - surgical |
Low |
Fast |
Higher |
|
Spinal - medical |
Medium |
Medium |
Higher |
|
Cataract |
Medium |
Fast |
Higher |
|
Tonsillectomies |
High |
Slow |
Consistent |
|
Endoscopies |
Medium |
Medium |
Higher |
|
Invasive angiograms |
Medium |
Medium |
Lower |
The long-term impact of the pandemic's disruptions on the health and wellbeing of the DHMS medical scheme member population is yet to be fully understood or quantified. We continue monitoring this impact.
In summary:
- By 2022, spinal and cataract surgeries experienced a relatively quick recovery to pre-pandemic admission levels. Admissions for these procedures continued to increase into 2023. This suggests that patients who would have undergone surgeries in 2020 and 2021, if not for the COVID-19 pandemic, did not experience improvement in their condition and had surgery when feasible.
- By June 2023, endoscopies increased to above pre-COVID-19 levels. As endoscopies are performed for both screening and diagnostic purposes, it's encouraging to see these trends.
- By June 2023, the volume of cataract surgeries taking place increased compared to both 2019 and 2022 levels - reflecting the medical scheme member base ageing year-year and deferred procedures being caught up.
- By June 2023, tonsillectomies were just under pre-pandemic levels, without evidence of catch-up procedures happening. These trends suggest that, in contrast to spinal and cataract procedures, patients who would have undergone tonsillectomies had they not needed to postpone them, may not have needed them later on.
- This may indicate that these surgical interventions are performed for patients who in fact have self-limiting symptoms. This is supported by a 2014 Cochrane review, which found marginal benefits in the recurrence of sore throats in children post tonsillectomy and adenoidectomy. Authors note, 'It is clear that some children get better without any surgery, and that whilst removing the tonsils will always prevent 'tonsillitis', the impact of the procedure on 'sore throats' due to pharyngitis is much less predictable. Insufficient information is available on the effectiveness of adeno-/tonsillectomy versus non-surgical treatment in adults to draw a firm conclusion. The impact of surgery, as demonstrated in the included studies, is modest'. It is likely that procedures recorded in 2023 are mostly new cases.
- It is very interesting that the drop in invasive angiograms over 2020 and 2021 wasn't paralleled by an (expected) increase in strokes and heart attacks during the pandemic. Invasive angiograms are still suppressed compared to the 2019 volumes, encouragingly substituted by less invasive CTCA scans.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes.
Burton MJ, Glasziou PP, Chong LY, Venekamp RP. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database Syst Rev. 2014 Nov 19;2014(11):CD001802. doi: 10.1002/14651858.CD001802.pub3. PMID: 25407135; PMCID: PMC7075105. https://pubmed.ncbi.nlm.nih.gov/25407135/
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only the data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.