Experiences of a cardiopulmonary centre

Dr Angelique Coetzee shares the impact that non-communicable diseases (NCDs) will have on our healthcare system.
Background
The Moot Cardiopulmonary Centre opened in 2014. This abstract serves as a snap shot of our collective experience in the cardiopulmonary centre. Traditional non-communicable diseases (NCDs) are becoming increasingly more prevalent worldwide and this phenomenon is evident in the South African context as well. The prevalence of these diseases is increasing as a direct result of societal norms around food, industry and lifestyle.
The diabetes, hypertension and hypercholesterolaemia trifactor in NCDs have a devastating effect on our health care system. Incidence of asthma and chronic obstructive pulmonary disease (COPD) are also on the rise and are also alarmingly accompanying the classical NCDs trifactor. The synergistic effect of these NCDs on cardiovascular incidence is utterly devastating. Patients that are uncontrolled or ineffectively manage just one of the trifactors often end up with the poorest outcomes, placing considerable pressures on the health care system’s resources. A siloed approach to management of these patients has been proven to lead to worse patient outcomes and an increased cost to the health care system.
When there is more than one of the trifactor present, outcomes and quality of life suffers even further. This places an even higher burden on the resources of the health care system. This process is further exacerbated by the presence of both asthma and COPD, albeit COPD has worse outcomes than asthma when occurring concurrently with other NCDs.
The resultant quandary is that it becomes increasingly more arduous to manage patients with more than one NCD, as they require constant revaluation as to efficacy of the treatment plan in terms of medication and patient education. The role of a multidisciplinary team for effective management in such a scenario is not to be overlooked. The formation of strategic cardiopulmonary centres is the future for the management of NCDs. A singular cardiopulmonary centre can service the needs of communities over a large geographical area. This modelled approach lightens the burden of disease to the patient and decreases the burden on the health care system. Services that should be included as standard for cardiopulmonary centres include pre and post bronchodilation; ECG: Resting, Stress, Holter ECG’s; and Ambulatory blood pressure monitoring.
What we are finding
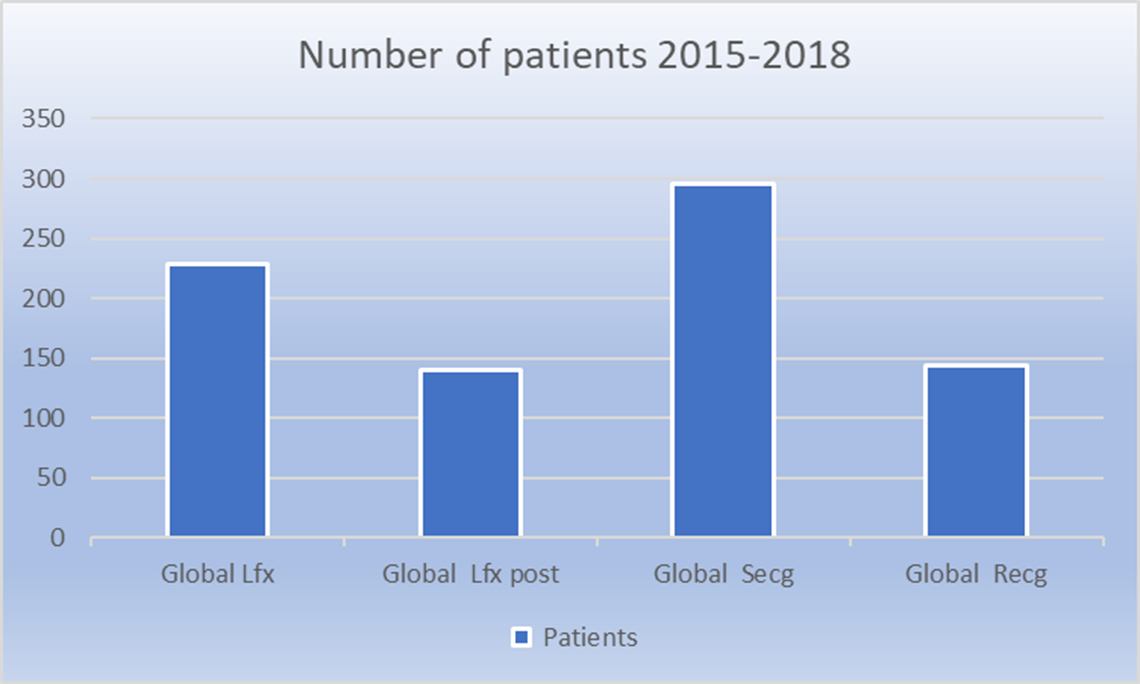
The experience in the Moot Cardiopulmonary Centre for the period of June 2017 to June 2018 has been documented. Some 56% of patients had been evaluated with stress ECGs, only 9% had a resting ECG, pre-lung function test was at 15%, pre and post lung functions were 20%.
The stress ECG tests resulted in a referral of seventeen patients for angiograms. These patients were all on chronic medication for one of the NCDs trifactor diseases (PMB) and the co-morbidities present were variable. Some 80% of these patients had an intervention in the cath-lab.
Ambulatory blood pressure monitoring resulted in the identification of hypertension in 74 patients (33%) and nocte hypertension in 52 patients. The number of patients that suffered from stress induced hypertension was 96 in total. Thirty of the patients were already on medication for hypertension and required further titration of their medication.
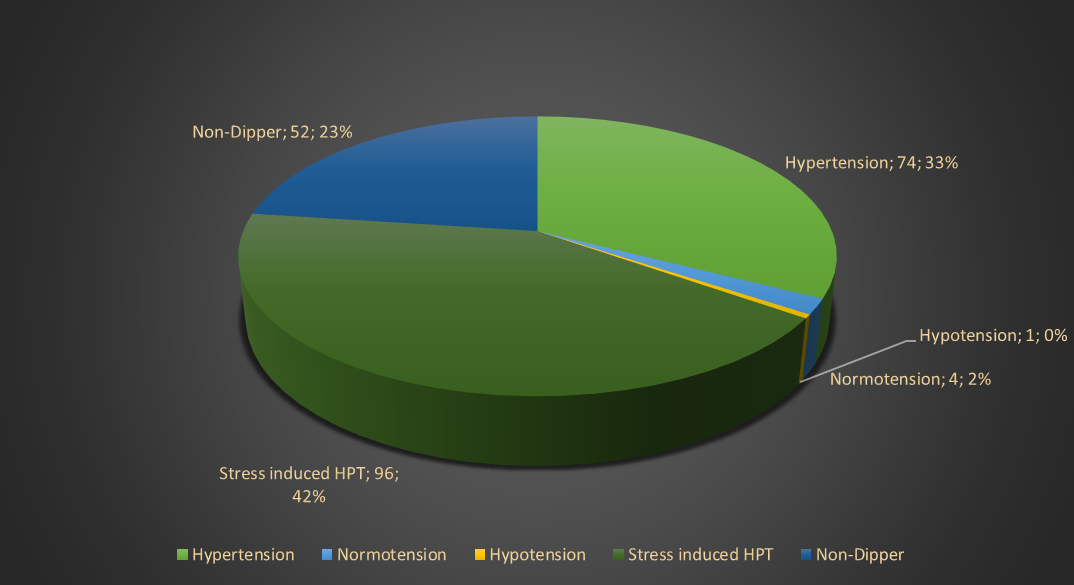
Figure 1 Ambulatory Blood Pressure dispersion
Pre and post lung function (concurrent use of GINA and GOLD guidelines) testing resulted in the diagnoses of asthma at 29%, and COPD at 21%. Patients with mixed obstructive presentations accounted for 7% of the total population. Some 29% of patients had normal spirometric and clinical values. Of the patients tested, nineteen had their medications changed.
Patient outcomes improved, especially with COPD patients correctly diagnosed with the appropriate medication. There was a decrease in hospitalisation and after-hour emergency visits for acute chest pain, pneumonia and bronchitis by the patients evaluated. Cardiovascular patients were appropriately referred, thereby reducing the incidence of unnecessary referrals. No uncontrolled hypertension patients were referred, as they were correctly managed by their general practitioners.
Management of patients in the NCD sphere require a multidisciplinary approach that is transparent and effective without duplicating procedures and unnecessary specialist or hospital referrals. This management approach identifies the urgent cases that do indeed require hospital and/or specialist referrals with supporting evidence, thereby reducing the waiting time for appropriate interventions.
Authors: Dr. A. Coetzee MBChB, R.J. Lourens Clinical Technologist (Critical Care); J.F. Lourens BCom Human Resource Management

Dr Angelique Coetzee
General Practitioner