SAMJ Publication: Analysis confirms COVID-19 disrupted private healthcare in South Africa

A large-scale study of COVID-19's impact on private healthcare finds South Africa's outbreak significantly reduced emergency room visits, hospitalisations and doctor visits, and some forms of cancer screenings. Our findings add to a growing body of work suggesting that COVID-19 healthcare disruptions may have important but unknown impacts on other disease outcomes.
COVID-19 reorganised healthcare fear kept patients away from facilities
On 11 March 2020, the World Health Organization (WHO) declared COVID-19 a pandemic, just six days after South Africa recorded its first case of the new disease.1 South Africa, like many countries, implemented strategies to slow the spread of the COVID-19 epidemic, including lockdowns of varying severity (stay-at-home orders, movement restrictions and curfews). The country's initial 21-day lockdown from late March to April 2020 was the most severe and included a period in which people were confined to their homes.
Although essential medical services continued throughout South Africa's outbreak, COVID-19 led to the re-organisation of the healthcare system. Elective (planned) surgeries, considered less urgent, were paused to create capacity to manage COVID-19 cases, particularly during peaks in transmission. Certain high-volume hospitals, meanwhile, closed due to facility outbreaks.2
Several studies found that utilisation of routine healthcare services fell in South Africa during COVID-19. The National Income Dynamics Study (NIDS) - Coronavirus Rapid Mobile Survey (CRAM), for instance, found that nearly a quarter of adults surveyed could not access medication or contraception in the four weeks prior to being interviewed.3 Nearly an equal proportion of those who said they needed acute care during this time did not seek treatment. Subsequent research similarly found that access to public health services nationwide was limited during the first year of the COVID-19 outbreak, in particular antenatal care, contraception, and HIV and tuberculosis testing.4
Early in the epidemic, a large share of unmet healthcare need was attributed to fears of being exposed to COVID-19 at health facilities. This fear was reported in as many as 37% of the pregnant women or new mothers who said they had not visited a health facility in the previous two months.5
Still, studies evaluating COVID-19's impact on healthcare in South Africa have focused largely on the first year of the pandemic and have excluded hospital-level care.
How we covered COVID-19's impact on private healthcare in South Africa
To investigate COVID-19's impact on private healthcare services, we compared anonymised claims data from all Discovery Health Medical Scheme (DHMS) members between April and December in each of the following years: 2019, 2020 and 2021. DHMS is the country's largest open medical scheme with about 2.8 million members.
Our analysis, published in the South African Medical Journal, tracked four areas: emergency room visits, hospital admissions, out-of-hospital doctor visits for patients with chronic conditions, as well as cancer screenings and registrations for Discovery Health Medical Scheme's Oncology Care Programme.
Visits to the Emergency Room (ER) are generally an indication of immediate care sought to relieve an acute condition or to manage a clinical emergency.
Hospital admissions included admissions to private hospitals, day clinics, rehabilitation centres and psychiatric hospitals. These admissions were categorised based on whether they were medical or surgical in nature as well as how severe cases were based on a case mix index. A case mix is a measure of the average severity of hospital admissions, considering both the mix of admissions (e.g., a heart transplant versus a pneumonia admission) and the complexity of the admission (e.g., a pneumonia admission for a patient with HIV versus a pneumonia patient without HIV). Case mix indices are lower for people with fewer concurrent health problems and for people with admissions that require less complicated care.
Doctor visits - visits to General Practitioners (GP's) - were limited to those among patients living with chronic conditions as identified by their status on Discovery's Chronic Illness Benefit. Discovery's Chronic Illness Benefit covers the 27 chronic conditions6 that qualify for Prescribed Minimum Benefits6 in South Africa as well as an additional 22 conditions7 for some members depending on their plan. Doctor visits included both in-person and virtual consultations.
Finally, cancer screenings were limited to mammograms and Pap smears as colon cancer screening was only introduced in 2019.
COVID-19 contributed to significant reductions in most areas measured
Our analysis reveals that COVID-19 led to significant reductions in emergency room visits, hospital admissions, in-person doctor visits and Pap smears particularly during South Africa's initial and strictest COVID-19 lockdown, (Table 1). The number of virtual doctors' consultations, however, rose. We also discovered that although hospital visits decreased during the first two years of COVID-19, patients who were being admitted were on average sicker than those admitted before the pandemic.
This was true whether patients were admitted for COVID-19 related care or other illnesses.
Table 1: Change in service utilisation rates or case mix index relative to 2019 levels
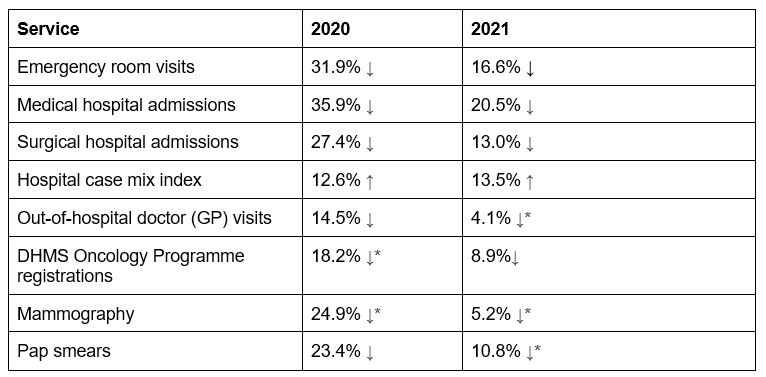
*Denotes change was not statistically significant
Fewer patients were admitted during COVID-19 but those who were, were also sicker
Emergency room visits fell significantly by almost a third (31.9%) between April and December 2020 as compared to the same period in 2019. In 2021, emergency room utilisation rebounded in the last four months of the year but overall, for the period analysed was still 16.6% less than in 2019. The greatest reduction in emergency room visits was observed during the strictest lockdown level in April 2020.
Total hospital admissions similarly decreased the most (62%) during the strictest lockdown in April 2020. In this month, the medical admission rate fell by 58.2% compared to April 2019 while surgical admissions fell even further (73.2%), (Figure 1).
Figure 1: Medical and surgical admission rate change, relative to 2019
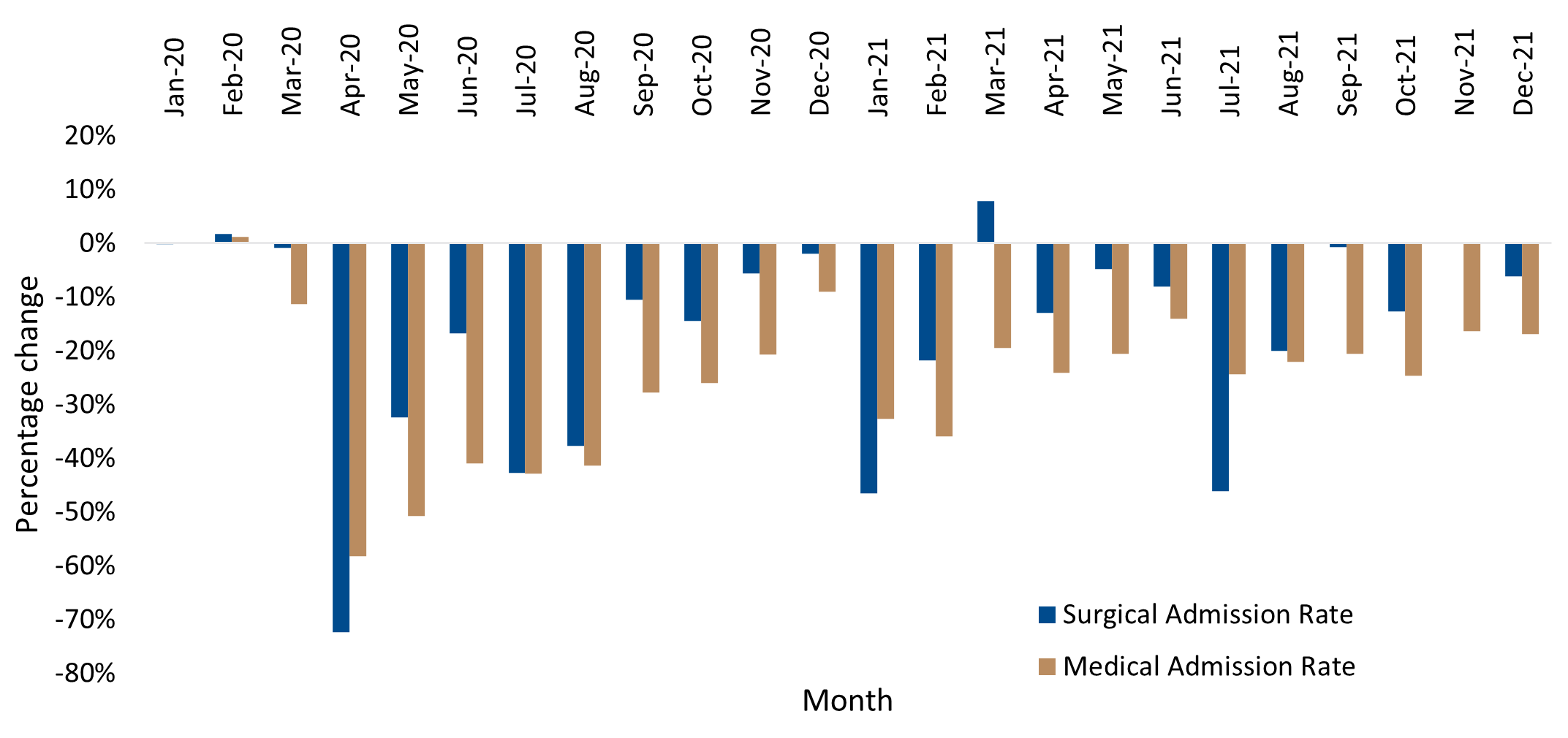
At the same time, patients who were admitted into hospitals both with COVID-19 as well as other illnesses were much sicker in 2020 and even more so in 2021 as compared to 2019, the case mix index showed. The average case mix index of 1.32 for April to December 2020 was 12.6% higher than the corresponding period in 2019, and this elevated case mix level persisted into 2021 with an even bigger differential of 13.5%.
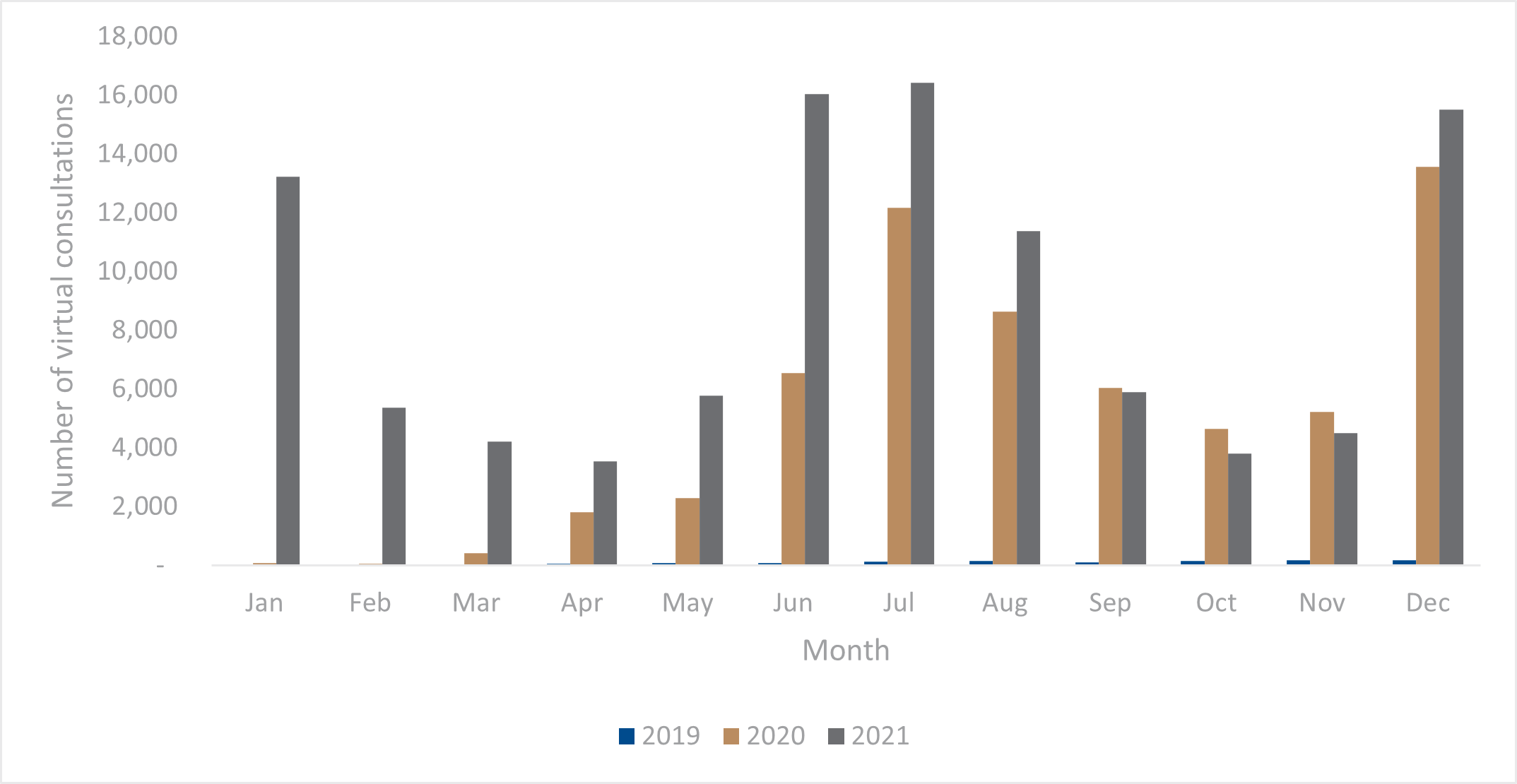
Telemedicine helped plug the gap in chronic illness care, but not enough
Doctor (GP) visits also fell among chronic disease patients in 2020 (14.5% per 1,000 chronic lives) against 2019 rates before rebounding in 2021 to nearly pre-pandemic levels. In 2021, the rate of doctor visits among people living with chronic conditions was still 4.3% less than those seen in 2019 but this was not statistically significant. The reduction in consultations also extended to specialists, including gynaecologists and psychiatrists. Peaks in virtual visits coincided with the surge in infections during the various COVID-19 waves but not enough to offset the reduction in face-to-face visits, (Figure 2 & 3).
General Practitioners accounted for the highest number of virtual consults followed by radiotherapists and general physicians.
Figure 2: Out of hospital doctor consultations per 1,000 chronic adult DHMS members (2019-2021)
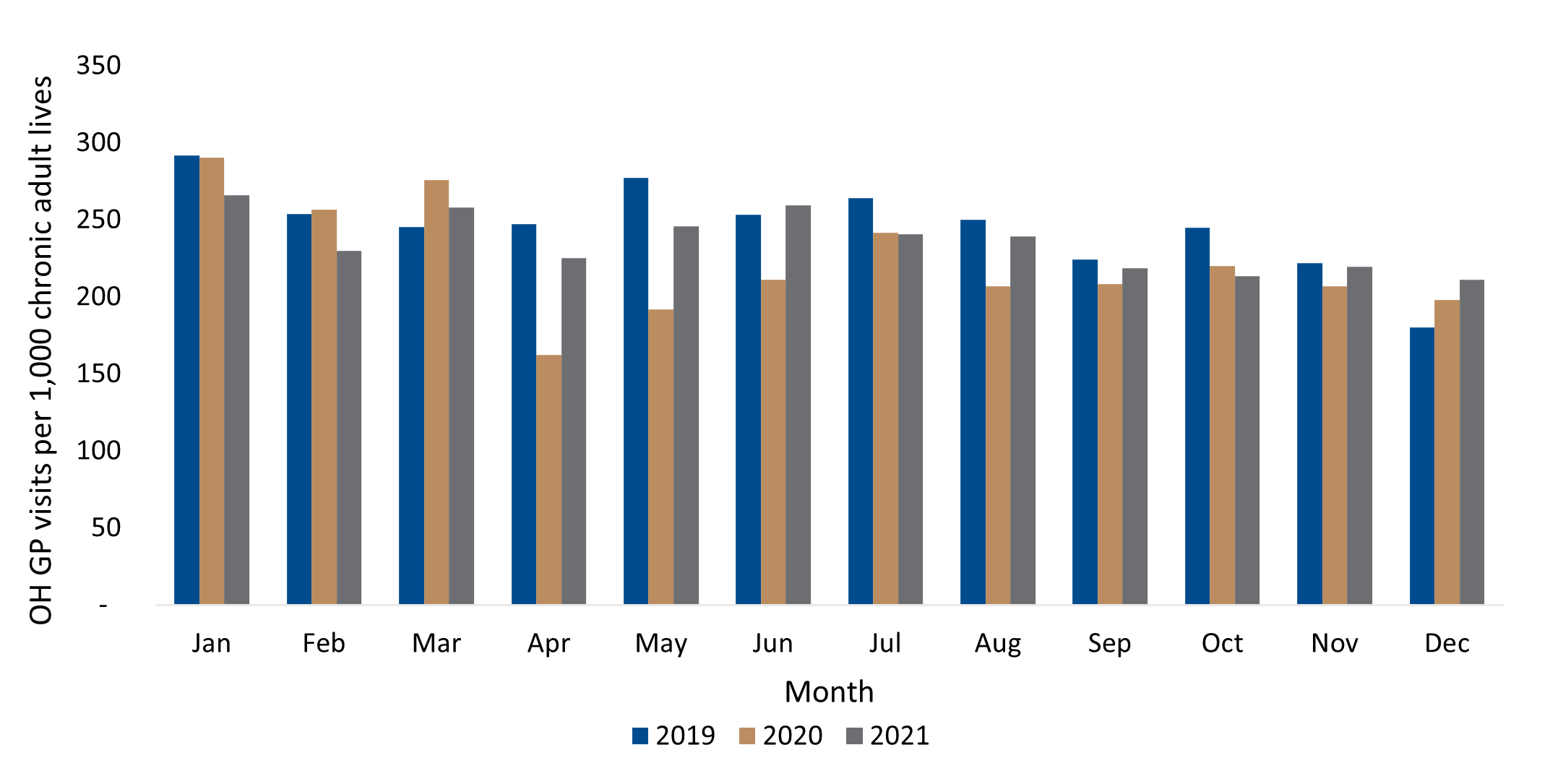
Figure 3: Number of virtual consultations (video and telephonic) for adult members (2019-2021)
Cancer screenings, already low, dropped further during COVID-19
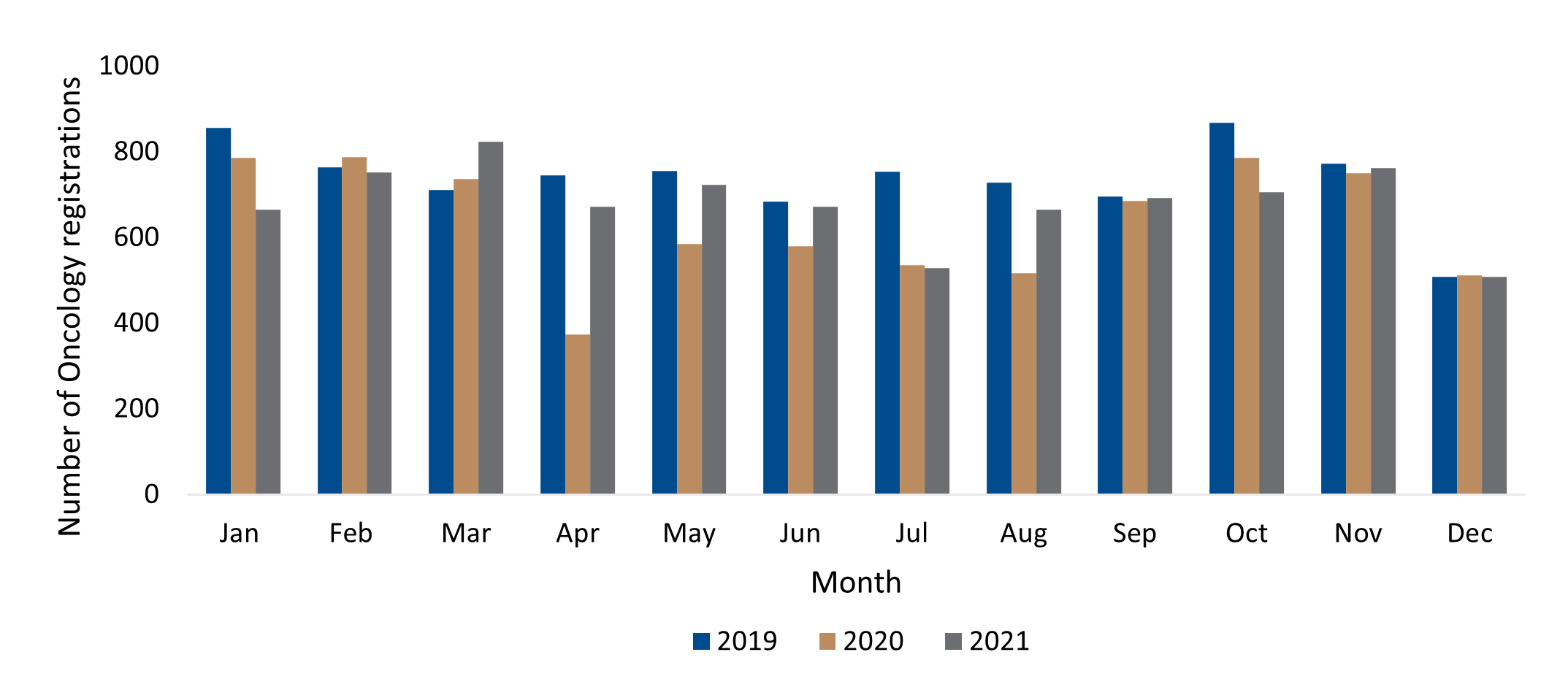
Registrations onto DHMS' cancer treatment programme dipped in 2020 (18.2%) although this was not a statistically significant decrease, as stated above. As in the case of emergency room visits and hospital admissions, cancer registrations fell the sharpest during April 2020's hard lockdown, (Figure 4). The rate of registrations increased in early 2021 after the second wave of infections but declined once again at the onset of the third wave and remains low when compared to previous years.
Figure 4: New adults DHMS oncology registrations (2019-2021)
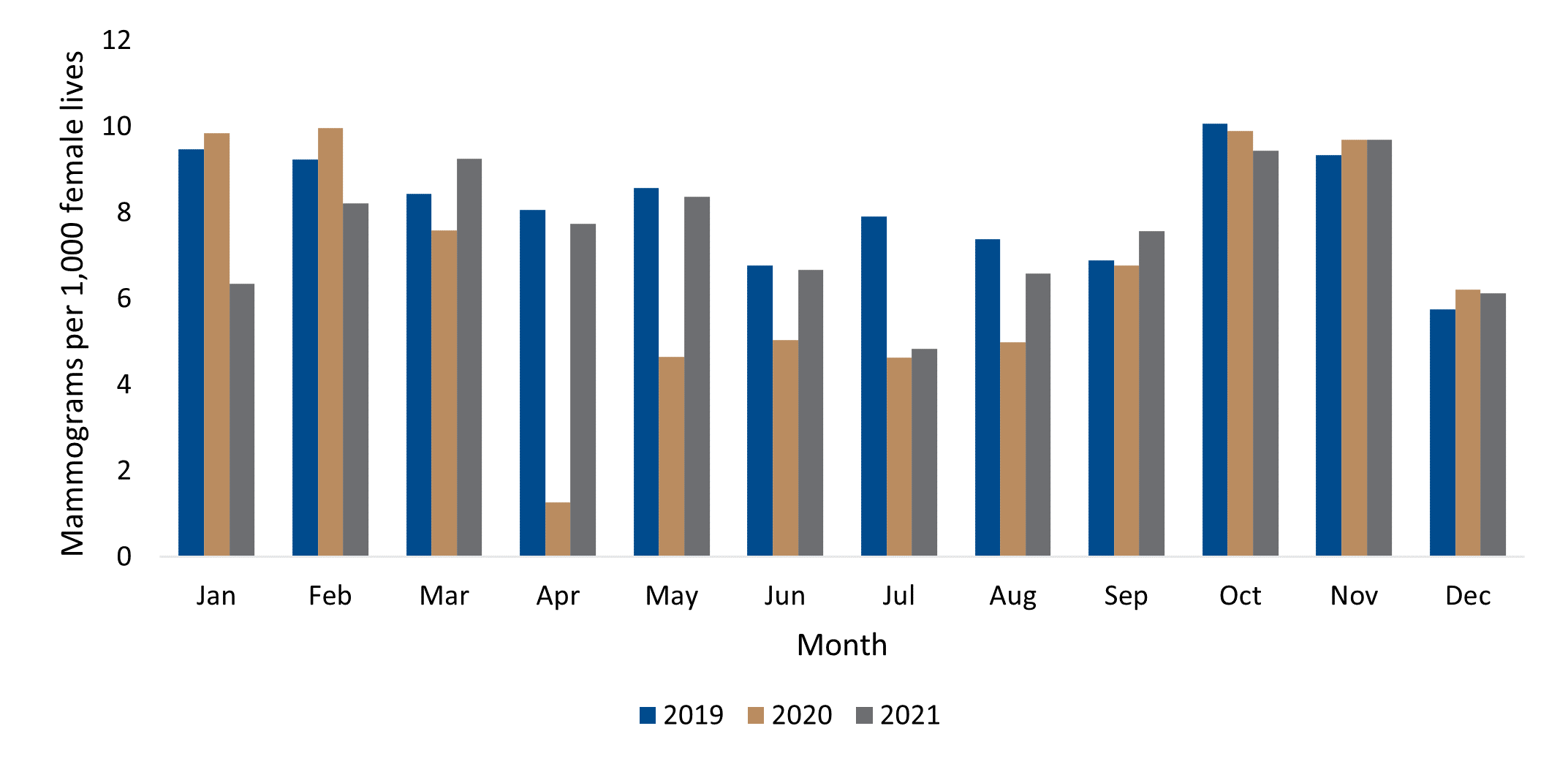
Similarly, the rate of mammograms per 1,000 female lives to detect breast cancer also decreased by nearly a quarter in 2020 (24.9%) before recovering to remain slightly lower (5.2%) than pre-COVID levels in 2021, (Figure 5). Neither dip in breast cancer screenings was statistically significant however.
Figure 5: Mammography cancer screenings for adult DHMS females (2019-2021)
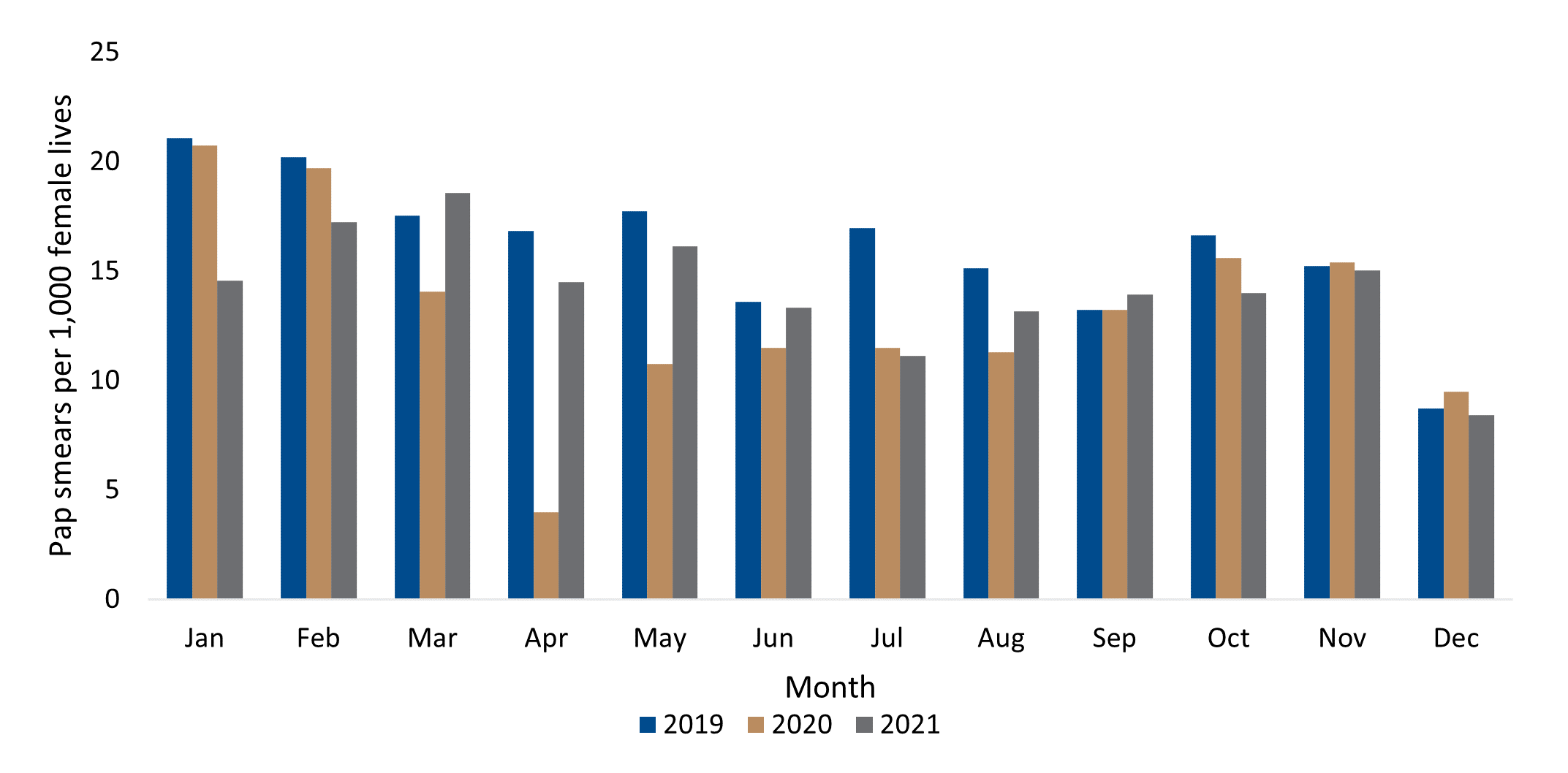
A statistically significant decrease (23.4%) was observed in Pap smear visits per 1,000 female lives in 2020 when compared to 2019, (Figure 6). This trend persisted into 2021 although the reduction (10.8%) in 2021 in relation to 2019 was not statistically significant.
Figure 6: Cervical cancer screenings for adult DHMS females (2019-2021)
DHMS introduced colorectal cancer screenings in 2019 however registrations for DHMS's Oncology Programme for this cancer fell during COVID-19 in 2020 (16.5%) and continued in 2021 (12.1%). As with declines in mammography, reductions in colorectal cancer were not statistically significant.
In summary, our analysis found declines in cancer screenings and registrations in DHMS's Oncology Programme during the first two years of the COVID-19 epidemic in South Africa. In 2021 however, there appears to be an improvement approaching pre-pandemic levels for breast cancer and cervical cancer screening.
Although only reductions in 2020 Pap smears were found to be statistically significant, the decreased utilisation of cancer screenings and care is concerning given South Africa's already low rates of cancer screening. Therefore, any decrease in cancer screening is coming off an already low base.
Lower uptake of services during COVID-19 could lead to more serious illness in the future
Our research adds to a growing body of evidence that shows COVID-19 reduced the uptake of other health services, namely in this study emergency room visits, hospital admissions, doctor visits and cancer screenings. Our study is the first in the South African private sector to evaluate this using a large claims-based dataset.
Although some reductions in cancer screenings and care were not statistically significant, these decreases alongside significant reductions in medical and surgical hospital admissions and doctor visits may result in patients presenting with more severe illnesses in the future. More long-term research will be needed to confirm or disprove this hypothesis.
Scaling up decentralised health services could solve age-old problems
Previous studies have suggested that fear of being exposed to COVID-19 in healthcare settings played a key role in driving reductions in primary healthcare. Although it was beyond the scope of this study, based on claims data, to evaluate the reason for lower uptake of services, we found considerable decreases in emergency room visits, hospital admissions and cancer screenings correlated with South Africa's strictest movement restrictions. These findings may inform current pandemic preparedness discussions about how to best safeguard essential health services during outbreaks, for instance by scaling up digital or home-based care.
However, our data suggest that some changes in healthcare utilisation patterns seen in South Africa during COVID-19 present several opportunities by helping to decentralise care, initially by providing a catalyst for the adoption and scale of digital health services. Secondly, shifts in the uptake of hospital services may provide the South African private health sector with a chance to remedy long-standing patterns of hospital overutilisation by shifting care to outpatient settings, including the home.8 A continued shift towards decentralised care like this will drive down healthcare costs while possibly improving care.
Study authors
Noluthando Nematswerani (Head of Clinical Policy Unit, Discovery Health), Lizelle Steenkamp (Senior Healthcare Statistician, Discovery Health), Sameera Haneef (Senior Actuary, Discovery Health), Roshini Moodley Naidoo (Head of Risk Management and Quality of Care, Discovery Health) and Sharon Fonn (Head of School of Public Health, Witwatersrand University)
- World Health Organization. Rolling updates on coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed 12 October 2021).
- Parliamentary Portfolio Committee on Health. Health Committee Welcomes Closure of St Augustine's Hospital. 09 April 2020. https://www.parliament.gov.za/press-releases/health-committee-welcomes-closure-st-augustines-hospital (accessed 11 November 2022)
- Burger, R., Nknonki, L., & Rensburg, R. (2020). Examining the unintended health consequences of the COVID-19 pandemic in South Africa. Wave 1 National Income Dynamics Study (NIDS)-Coronavirus Rapid Mobile Survey (CRAM), 2020.
- Pillay, Y., Pienaar, S., Barron, P., & Zondi, T. (2021). Impact of COVID-19 on routine primary healthcare services in South Africa. South African Medical Journal, 111(8), 714-719.
- Spaull, N., Ardington, C., Bassier, I., Bhorat, H., et. al. (2020). Overview and Findings. NIDS-CRAM Synthesis Report Wave 1.
- Discovery Health Medical Scheme. Prescribed Minimum Benefits List of Conditions. 2021. www.discovery.co.za/wcm/discoverycoza/assets/medical-aid/benefit-information/2021/pmb-conditions-list-2021.pdf (Accessed 13 November 2022.)
- Discovery Health Medical Scheme. Cover for Medicine and Treatment of Chronic Conditions. 2022. https://www.discovery.co.za/wcm/discoverycoza/assets/medical-aid/benefit-information/2022/cover-for-medicine-and-treatment-of-chronic-conditions.pdf (Accessed 13 November 2022.)
- Competition Commission of South Africa. Health Market Inquiry Final Findings and Recommendations Report. September 2019. Government Gazette No. 42861, 29 November 2019. https://www.gov.za/sites/default/files/gcis_document/201911/42861gon1533.pdf (Accessed 14 November 2022)
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Read our related post on how Discovery Health is developing new ways of measuring the quality of hospital care
Disclaimer
All information shared on this page is based on perspectives gained from analysis of figures and trends emanating from Discovery Health's data pool. The analysis, which is conducted by Discovery Health's actuarial and data scientist team, aims to encourage industry dialogue. This content is shared for educational and informational purposes only.

Deep dive: Admission rates across South Africa's four COVID-19 waves confirm Omicron-driven fourth wave's lower severity, and more.
07 July 2022
Authors: Chana Suttner (Actuary, Discovery Health),Michael Cohen (Actuarial Analyst, Discovery Health), Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health

Long COVID symptoms, impact on carrying out daily activities: Survey of just over 7,000 medical scheme members reveals key insights
16 June 2022
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health), Lizelle Steenkamp (Senior Healthcare Statistician, Discovery Health), Lebohang Radebe (Data Scientist, Discovery Health), Dr Smybinn Mathews (Clinician, Discovery Health) and Dr Dave Jacobs (Senior Clinician and Clinical Classification System Architect, Discovery Health)

Discovery's COVID-19 personal resilience index predicts an individual's resilience to serious COVID-19 illness
23 May 2022
Authors: Lizelle Steenkamp (Senior Healthcare Statistician at Discovery Health), Tommy Chen (Actuary at Discovery Health), Jared Champion (Senior Actuary at Discovery Health) and Donald Ntjana (Senior Data Scientist at Discovery Health)