Two to eleven-fold higher risk of death from COVID-19 for all scheme members

Medical scheme members over six years of age are at varying degrees of heightened risk of mortality when infected with COVID-19. There is also additional risk peaking in members aged 56 to 60. This drives home the importance of the preventive behaviours that limit our exposure to COVID-19 disease, and of being vaccinated against the disease.
Authors
Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health) and Lizelle Steenkamp (Head of Risk Intelligence, Discovery Health)
Methodology
A death is classified as COVID-19 related if it is a:
- Natural death within 14 days of discharge from hospital for a COVID-19 admission
- Death in hospital after a person has been admitted to treat COVID-19 disease
- Natural death within 28 days of a positive PCR test in people with no admission during that interval.
- Please refer to last section of this post for clarity on the above-mentioned definition of COVID 19 mortality
We obtained records of deaths related to COVID-19 disease (based on the above definitions) and expressed the total as 'COVID-19 mortality rates per 1 000 infections'.
'COVID-19 mortality rates per 1 000 infections' were compared to overall annual mortality rates among members of medical schemes administered by Discovery Health before the start of the pandemic. This data is from 2017 to 2019 and expressed as a rate per 1 000 lives, in five-year age bands.
Results
The figures in the table underneath the graph also show that the mortality risk for an individual aged 36 to 40 who contracts COVID-19 (8.5 per 1 000 infections) is similar to the all-cause mortality risk faced by individuals aged 61 to 65 in a year (8.9 per 1 000 lives). This shows the serious impact of COVID-19 infection even on middle-aged people who are not considered at high-risk of serious COVID-19 illness by virtue of their age.
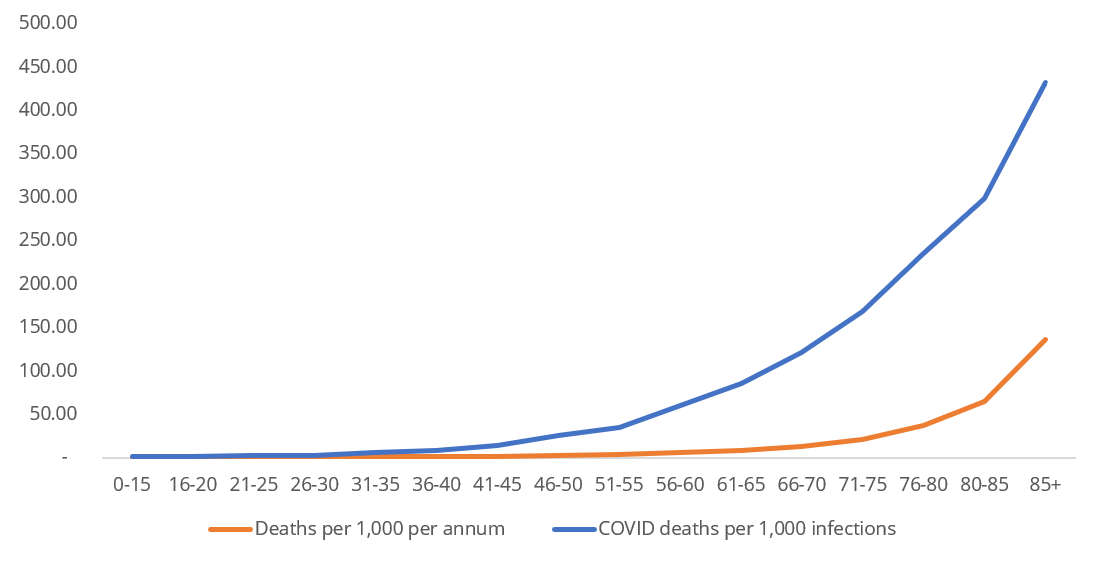
Figure 1: All cause deaths per 1 000 lives (2017 to 2019) compared to COVID-19 related deaths per 1 000 infections
Figure 2 visually depicts the data that is in the table below Figure 1 - the actual size of the increase in relative mortality risk from COVID-19 infection within each age band.
- There is an increased mortality risk across all age bands
- Individuals aged 56 to 60, on aggregate, have the highest relative mortality risk increase from COVID-19 infection (a 10.7-fold increase) relative to the typical mortality risks faced by individuals in this age band (5.65 deaths per 1 000 lives each year) before the COVID 19 pandemic.
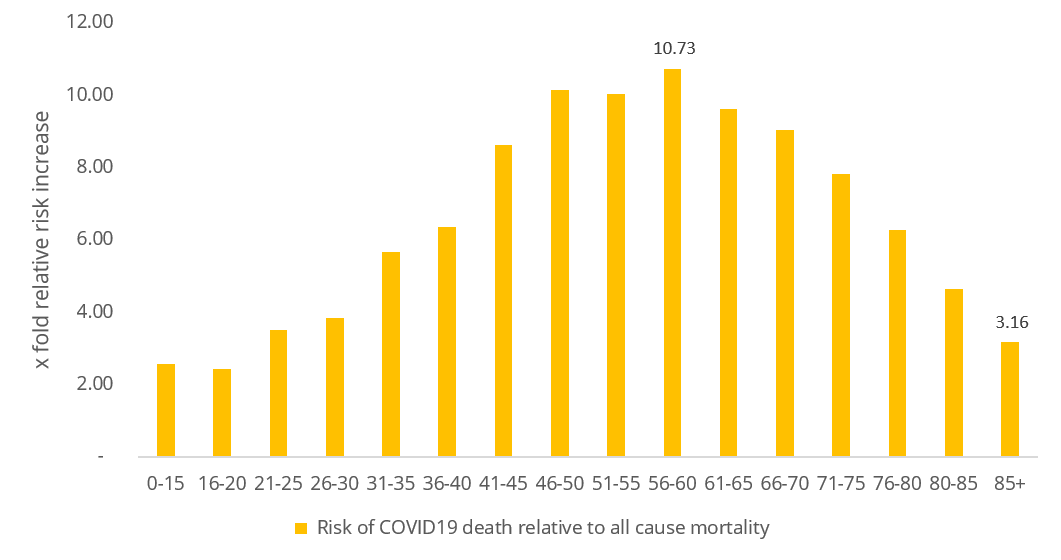
Figure 2: Risk of COVID-19 death per 1 000 infections compared to all-cause mortality risk (from 2017 to 2019) per 1 000 lives
Impact of vaccines on severe COVID-19 infection
In a recent post, we shared data about how vaccination rates among Discovery Health administered medical scheme members have declined across all eligible age bands from 17 May to 20 September 2021.
The recorded reduction in vaccination rates may be caused by the phenomenon of COVID-19 vaccine hesitancy. This is partly driven by people's fears of experiencing serious COVID-19 vaccine-related side effects, even though they are extremely rare. We also show that reluctance to get vaccinated may be driven by scheme members' perception of being at low risk of experiencing serious COVID-19 illness or death (measured through Discovery Health's COVID-19 Personal Resilience Index scores)).
Overall, the data shared in the analysis on this page shows that all scheme members over the age of six years old are at varying degrees of heightened risk of mortality when infected with COVID-19. This risk peaks between ages 56 and 60. This drives home the importance of the preventive behaviours that limit our exposure to COVID-19 disease, and of being vaccinated to reduce our risk of severe COVID-19 illness and death.
In relation to the protective effects of vaccines available to the South African public:
- Based on Discovery Health's data (up to 9 September 2021), two doses of the Pfizer BioNtech COVID-19 vaccine are 90% effective in preventing serious COVID-19 illness requiring admission to hospital. We will soon publish a summary of this data on the Discovery Health Insights website.
- Promising data emerged from the South African Medical Research Council's study of the Sisonke trial. In this trial, just under 480 000 local healthcare workers received the single dose Johnson & Johnson (J&J) vaccine. Analysis showed up to 71% protection against severe illness and hospitalisation and up to 95% protection against death. Also, 96% of breakthrough infections (infections post vaccination) were mild, 3% were moderate and less than 0.05% were severe or critical. Importantly, the study found that the J&J vaccine has an excellent safety profile while also offering good immediate and sustained immune responses against the Delta variant (with immune protection lasting up to eight months).
CLARITY ON THE DEFINITION OF COVID-19 REPORTING DEFINITION USED IN THIS ANALYSIS
The process of determining underlying cause of death is based on the World Health Organization's (WHO's) coding guidelines. This requires the review of all available historical medical documentation and diagnoses. This is a rigorous and time-consuming process.
Since 2008, Discovery has conducted yearly auditing processes in which trained and certified personnel confirm deaths and underlying causes of death based on WHO coding standards.
In the context of COVID-19 deaths
A WHO document from 20 April 2020 titled "International guidelines for certification and classification (coding) of COVID-19 as cause of death" states:
"A death due to COVID-19 is defined for surveillance purposes as a death resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID diseases (e.g., trauma). There should be no period of complete recovery from COVID-19 between illness and death. A death due to COVID-19 may not be attributed to another disease (e.g., cancer) and should be counted independently of pre-existing conditions that are suspected of triggering a severe course of COVID-19."
Discovery Health has assessed all relevant medical, pathology and claims documentation and completed death audits to establish underlying cause of death, up to 31 March 2021. In consultation with the National Institute for Communicable Diseases and principal investigators for Sisonke, Discovery Health has developed a reasonable reporting definition to capture most COVID-19 deaths. This definition includes the WHO guidelines and industry experience.
For the period from 1 March 2020 to the end of March 2021, we have found the following rates of correspondence between Discovery Health's COVID-19 reporting definition and the audited underlying cause of death:
- Underlying cause of death consistent with our reporting definition - 6 176 deaths
- Underlying cause of death COVID-19 related but not included in our reporting definition - 398 deaths
- Underlying cause of death not COVID-19 related but included in our reporting definition - 219 deaths
Our mortality reporting definition is therefore deemed appropriate for the following reasons:
- There is a high level of concordance between the reporting definition and the audited underlying cause of death (93.9% (6176/ (6176+398)) of confirmed COVID-19 deaths. Also, the error rate of misclassification of deaths was 3.5% (219/ 6176), based on data from March 2020 to March 2021.
- The number of all-cause excess deaths on the scheme for the period March 2020 to March 2021 was 6 343, relative to 2018 and 2019 mortality rates. This was consistent with the number of COVID-19 deaths. Furthermore, the monthly pattern in the number of total deaths mirrors the active COVID-19 caseload total.
The number of natural all-cause excess deaths in South Africa (recorded by the SAMRC) has exceeded reported COVID-19 deaths, and has also followed the pattern of COVID-19 caseloads in the country. This is not unexpected given that reporting COVID-19 as an underlying cause of death is dependent on clinical documentation. It is plausible that many uninsured South Africans had not undergone a confirmatory PCR test or been hospitalised for COVID-19 treatment before they died.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and any further context required.
Did you find this post useful?
You may also be interested in reading another post explaining how "Home monitoring using a pulse oximeter linked to 48% lower likelihood of death in high-risk scheme members who have COVID-19". This article details our research which was recently published in the South African Medical Journal.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only the data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.

Why are COVID-19 vaccination rates declining amongst members of schemes administered by Discovery Health? What are possible drivers and deterrents of uptake?
04 October 2021
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health) and Lizelle Steenkamp (Head of Risk Intelligence, Discovery Health)
The South African Medical Journal has published Discovery Health's new research paper: "The impact of routine pulse oximetry use on outcomes in COVID-19-infected patients at increased risk of severe disease: a retrospective cohort analysis".

Using pulse oximeters could reduce likelihood of COVID-19 death
7 September 2021
Authors: Shirley Collie (Chief Analytics Actuary at Discovery Health), Jared Champion (Senior Actuary at Discovery Health), Tommy Chen (Actuary at Discovery Health) and Michael Cohen (Actuarial Analyst at Discovery Health)
The South African Medical Journal has published Discovery Health's new research paper: "The impact of routine pulse oximetry use on outcomes in COVID-19-infected patients at increased risk of severe disease: a retrospective cohort analysis".

Comparing severity of Gauteng's first, second and third waves of COVID-19 infection by investigating hospital admission rates
21 July 2021
Authors: Shirley Collie (Chief Healthcare Analytics Actuary, Discovery Health) and Tommy Chen (Actuary, Discovery Health)
The highly transmissible Delta variant has driven an exponential rise in COVID-19 cases in South Africa's third wave of infection, and in Gauteng in particular - the province that is the focus of this analysis. Encouragingly, our initial data shows that compared to the second wave of infection, COVID-19 infections in the third wave are not associated with increased risk of hospital admission.