How DHMS Operates
The Scheme exists for the benefit of our members, and we place them at the centre of care.
Sustaining the Scheme's financial, operational and reputational wellbeing ensures our ability to continue funding quality healthcare for individual members, which requires equitable consideration of the interests of our whole membership base. As a funder that connects our members into the private healthcare value chain, the quality of our relationships with all our stakeholders is essential to how we create sustainable value for our members in line with our purpose, and to realising our vision of market leadership in a better healthcare system.
The Scheme's business model centres on delivering excellence in our core activities, which are primarily effective medical schemes governance and oversight.
We outsource administration and managed care services to Discovery Health (Pty) Ltd
In accordance with the Act and the Scheme Rules, the Trustees have appointed an accredited administrator and managed care provider to deliver these services to the Scheme and our members.
We elect to use a single provider as the Trustees believe that an integrated model (as opposed to a fragmented model using multiple service providers) delivers best value for money and optimal efficiency. Based on the measures applied to evaluating the services Discovery Health provides to the Scheme, the Trustees are satisfied that we contract with the best administrator and managed care provider in the sector.
Administration and managed care agreements specify the defined and measured outcomes the Scheme expects from Discovery Health. Service level agreements set out performance expectations across a wide range of measures. Discovery Health reports formally to the Scheme on these contractually agreed key performance indicators on a monthly, quarterly and annual basis. In addition, Discovery Health raises any operational or strategic concerns with the Scheme Office.
Discovery Health provides industry-leading capabilities to our members, including initiatives to combat fraud, waste and abuse.
Robust relational governance practices underpin the Scheme's relationship with Discovery Health. From time to time, the Board will commission independent assessments of these practices, benchmarked against local and international governance practice, contracting principles, independence requirements, and the ability to meet members' needs. These assessments provide the Trustees with assurance that the Scheme is applying best practice in governing this outsourced relationship, and any areas identified for improvement are actively implemented and monitored.
Value for money
The Trustees take their responsibility to ensure impeccable governance of the Scheme very seriously, and every year commission an actuarial peer review on a calculation of value received by the Scheme for work done by Discovery Health. In 2023, the Scheme received R2.08 in value for every R1.00 paid to Discovery Health.
Our members benefit when our Administrator and Managed Care Provider adds more value than the fees paid to it by the Scheme. The value for money that Discovery Health provides includes access to highly effective managed care programmes, innovative provider networks, a wide range of benefit plans, and a significantly lower average contribution paid by our members when compared with the next eight open schemes.
As the assessment uses industry information, results are only available for the preceding year. A pragmatic and replicable methodology for measuring the value added by Discovery Health has been applied since 2014. The Scheme engaged NMG Consultants and Actuaries (Pty) Ltd (NMG) to perform an actuarial review on the reasonability of the data, methodology and results. NMG concluded that the methodology is appropriate, that the change in value added from 2022 to 2023 is reasonable, and that they did not encounter any significant anomalies in the data and calculations reviewed.
Lower than the next seven largest open medical schemes in 2025.

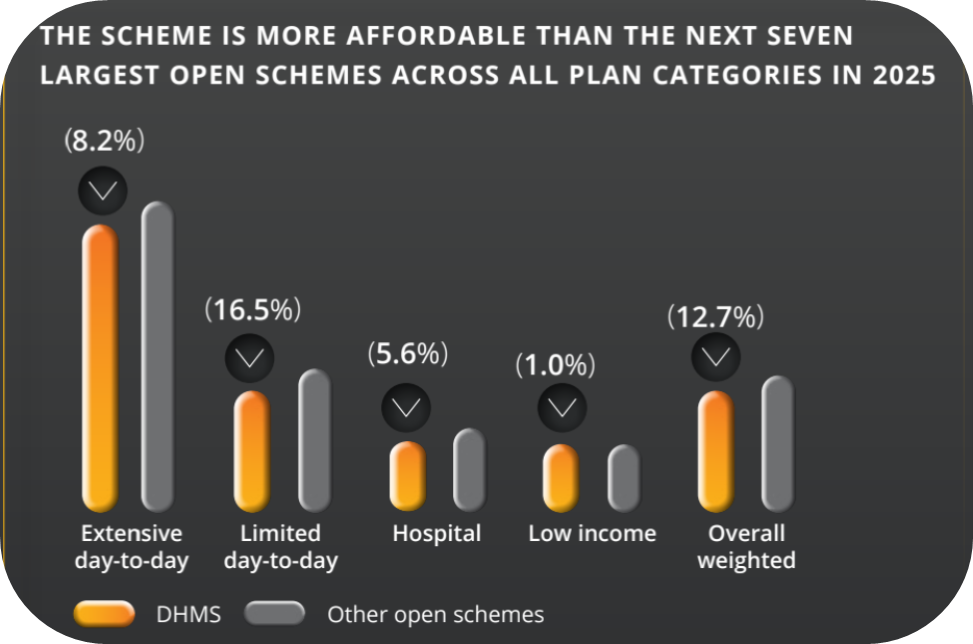
Source: publicly available contribution information for DHMS and the next seven largest open medical schemes. To ascertain the contribution differential between DHMS and competitors, we calculate an average contribution within each plan category for a principal member. These average contributions are then weighted (for DHMS and the next seven largest open schemes) according to the distribution of members across DHMS plans. This ensures that plans with similar benefits are being compared on a like-for-like basis, providing a reasonable estimate of the lower contribution that a typical member of DHMS pays relative to members of similar options in competitor schemes. Contribution rates on individual plans of other schemes vary and may be cheaper or more expensive than DHMS's equivalent plans. 2 Based on claimed amounts. Source: CMS Annual Report 2022-2023. Comparative data not yet available for 2023.
We use the Vested outsourcing model to govern our working relationship
The Vested outsourcing model aligns the transactional and relational governance elements of this relationship with global outsourcing best practice.
The principles of the model strengthen the strategic alignment between organisations and encourage a value-driven relationship. In effect, Vested frees both organisations to do what they do best by contracting for results and not activities - which allows for innovation, improved service and continuous value creation.
With respect to the Scheme's relationship with Discovery Health, the Vested model operationalises the Scheme's governance and oversight role and embeds its independence. It also allows us to leverage Discovery Health's expertise, systems, innovation and value-added services in the best interests of the Scheme and our members. The relationship is overseen by our Relationship Management and Innovation Committees, which are mandated to monitor, review and improve the relationship and the innovation that the Vested model promotes.
The commercial arrangements and scope of the agreement that give effect to the integrated (single provider) model and these Vested principles provide the certainty that Discovery Health needs to be able to invest significantly in innovation and new technologies. It also means that both organisations can take a longer-term view in driving positive changes to the healthcare system, which in turn supports the outstanding value we strive to deliver to our members.
As the assessment uses industry information, results are only available for the preceding year. A pragmatic and replicable methodology for measuring the value added by Discovery Health has been applied since 2014. The Scheme engaged NMG Consultants and Actuaries (Pty) Ltd (NMG) to perform an actuarial review on the reasonability of the data, methodology and results. NMG concluded that the methodology is appropriate, that the change in value added from 2022 to 2023 is reasonable, and that they did not encounter any significant anomalies in the data and calculations reviewed.