Celebrating HIV mortality improvements for HIV registered members on Discovery Health Medical Scheme

Long term mortality rates among HIV registered members on Discovery Health Medical Scheme have significantly improved, largely due to consistent adherence to antiretroviral therapy, effective viral load suppression and care support. These developments also highlight emerging challenges from non communicable diseases requiring continued focus on holistic care.
Authors
Discovery Health Intelligence team members Claudia Pastellides (Actuary), Chanie Suttner (Actuary), Xolani Masombuka (Analyst) and Lara Wayburne (Chief Health Intelligence Actuary)
Quick overview
Mortality rates for HIV‑registered members on Discovery Health Medical Scheme (DHMS) have declined over the long term, with the most significant reduction observed in deaths directly attributable to HIV. This improvement can be linked to consistent adherence to antiretroviral therapy (ART) and consistent viral load suppression, showcasing the effects of continued advances in HIV treatment and disease management support. We celebrate the positive impact on our HIV‑registered members, their families and the transformative role played by the healthcare system at large to help people with HIV live longer and healthier lives. While HIV‑registered members are living longer, the effects of non‑communicable diseases (NCDs) are emerging, both as a cause of death and as a multimorbidity.
Two global awards: Recognition for Discovery Health's HIV Managed Care Ecosystem


At the end of 2025, Discovery Health Medical Scheme's HIV Care Programme was recognised on the global stage, twice over.
- First, in early October Discovery Health won Best Health & Wellness Offeringat the Global Insurance Innovation Awards 2025 for its HIV Managed Care Ecosystem. The Global Insurance Innovation Awards are among the world's most prestigious accolades, celebrating organisations that are reshaping insurance through innovation, technology and meaningful customer impact.
- Then, in early November, the Programme won Gold (first place) in the category of 'Best Customer Experience for Vulnerable Customers' in the International Customer Experience Awards.
The HIV Managed Care Ecosystem refers to Discovery's integrated HIV Care programme which combines advanced data science, technology, and clinical expertise to deliver world-class support for HIV-positive members. The Ecosystem demonstrates how innovation, applied with empathy and compassion, can save lives, extend futures, and transform the way in which Discovery Health Medical Scheme members who are registered for HIV, experience and access the healthcare they need - the results of which are outlined in this report.
HIV mortality shifts from 4th to 13th place as a leading cause of death among DHMS members over a 13‑year period
In our article on mortality rates titled "COVID‑19 led to the highest death rates ever recorded among Discovery Health Medical Scheme (DHMS) members, finds 13‑year review of mortality rates", HIV was the fourth leading cause of death in 2012 after cardiovascular disease, cancer, non‑specific deaths and unintentional injuries. By 2022, the same three conditions ranked as the top three drivers of death, although cancer overtook cardiovascular‑related deaths. HIV had dropped to the 13th leading cause of death among DHMS members by 2022. This trend continued into 2024.
We therefore set out to investigate the following trends for DHMS members who are HIV‑registered:
- The trends in HIV mortality rates over a 13-year period from 2012 to 2024
- The trends in leading causes of death for HIV‑registered members over this period
- Clinical factors influencing mortality rates for HIV‑registered members
Our analysis focuses on HIV registered members, defined as those who are registered on Discovery Health Medical Scheme's HIV Care programme and does not include members who may be living with HIV but have not registered for the condition. The number and prevalence of HIV registered members increased from 2012 to 2018 and has remained relatively stable thereafter. A stable prevalence rate (percentage of members registered for HIV relative to the total membership) together with a reducing incidence rate for HIV registered members, indicates that HIV registered members are living longer. The incidence rate refers to the number of HIV registered members in a year relative to the unregistered membership.
As shown in Figure 1, the age profile of the HIV registered members has shifted significantly over the analysis period. In 2012, 24.3% of members were aged 35-39, compared to 16.0% in 2024. Conversely, the proportion of HIV registered members aged 50-55 increased from 6.1% to 14.3% over the same period. The HIV registered population remains largely concentrated among working-age adults, with relatively few younger or older members, both in absolute terms and compared to the overall DHMS population. This shift in age distribution reflects the increasing longevity of HIV registered members, with the cohort that was once concentrated in the 30-39 age band now shifting to nearly a decade older.
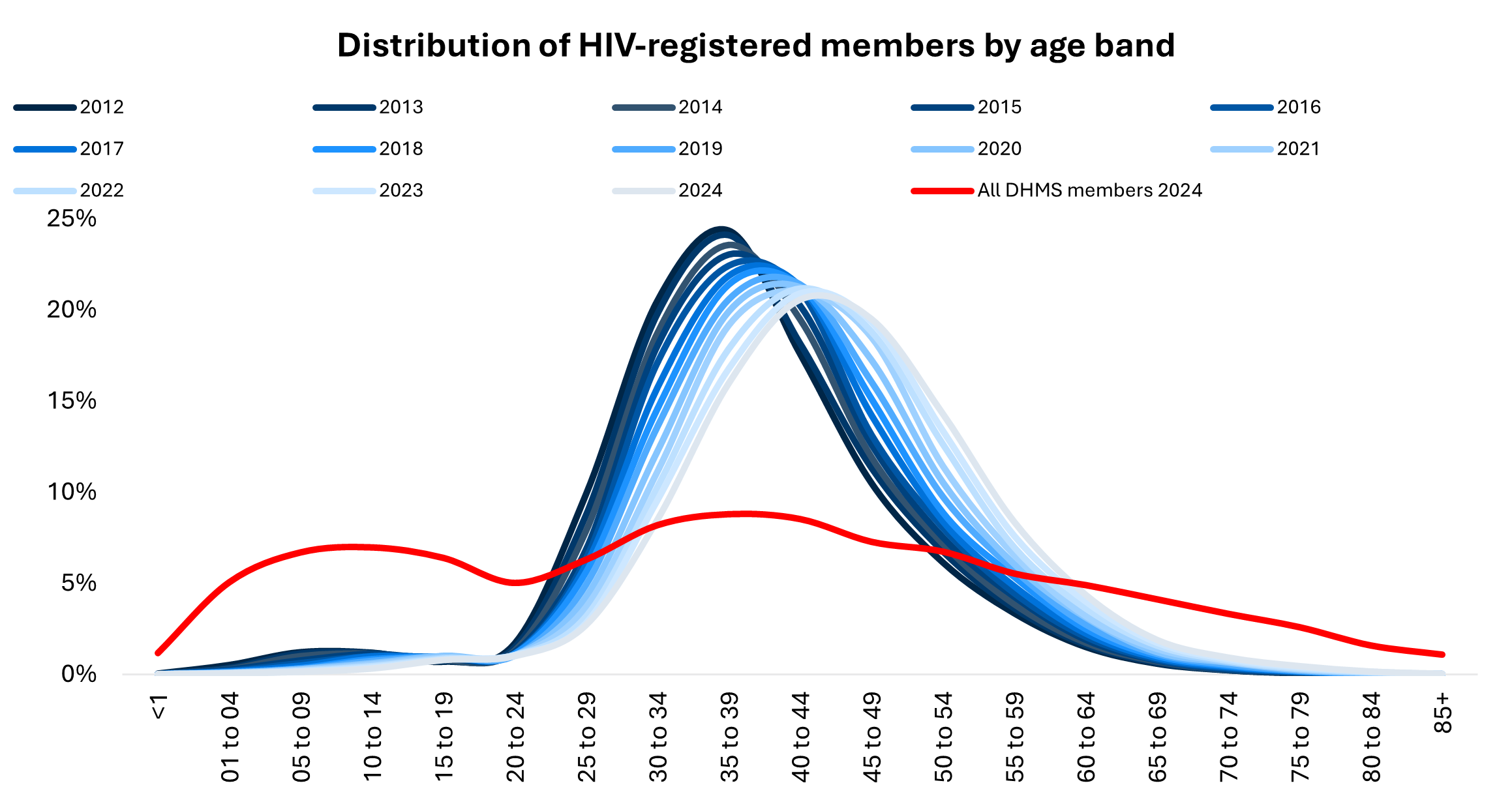
Figure 1: Distribution of HIV‑registered members by age band from 2012 to 2024 amongst DHMS members compared to all scheme members
Investigating mortality rate trends for HIV‑registered DHMS members
This article sets out an analysis of mortality experience of HIV‑registered adult members (aged >18 years old) of DHMS from 2012 to 2024.
How do we calculate mortality rates?
To examine mortality trends over time and compare them across different cohorts, we accounted for variations in age and sex distributions that can influence the underlying mortality rates. This methodology uses the same calculation of mortality as referenced in our previous article on a 13‑year review of mortality rates. We calculated confidence intervals for these standardised mortality rates using the gamma distribution‑based method proposed by Anderson and Rosenberg (1998) that provides more accurate estimates, particularly for low mortality counts.
We classified causes of death through detailed mortality audits and applied the World Health Organization (WHO) classification system to ensure consistency and accuracy in death reporting over time (World Health Organization, 2020).
Mortality trends and average age at death over 13 years for HIV‑registered members
From 2012 to 2024, after removing COVID‑19‑related deaths, the age‑ and sex‑standardised mortality rate for HIV‑registered members decreased by 47% (from 2,328 deaths per 100,000 lives to 1,234), compared to an 11% decline (from 673 deaths per 100,000 lives to 609) in age‑ and sex‑standardised mortality rate for members not registered for HIV benefits (Figure 2).

Figure 2: HIV‑registered vs non‑HIV‑registered mortality rates from 2012 to 2024 (age and sex standardised, excluding COVID‑19 deaths)
There has also been a trend of an increasing age at death for members registered for HIV benefits, indicating that members registered for HIV are living longer than in previous years. From 2012 to 2024, the average age at death for HIV‑registered members rose by eight years, a 23% improvement, increasing from under 43 to over 51 years (Figure 3). This trend reflects progress in managing HIV and improving life expectancy for affected members.
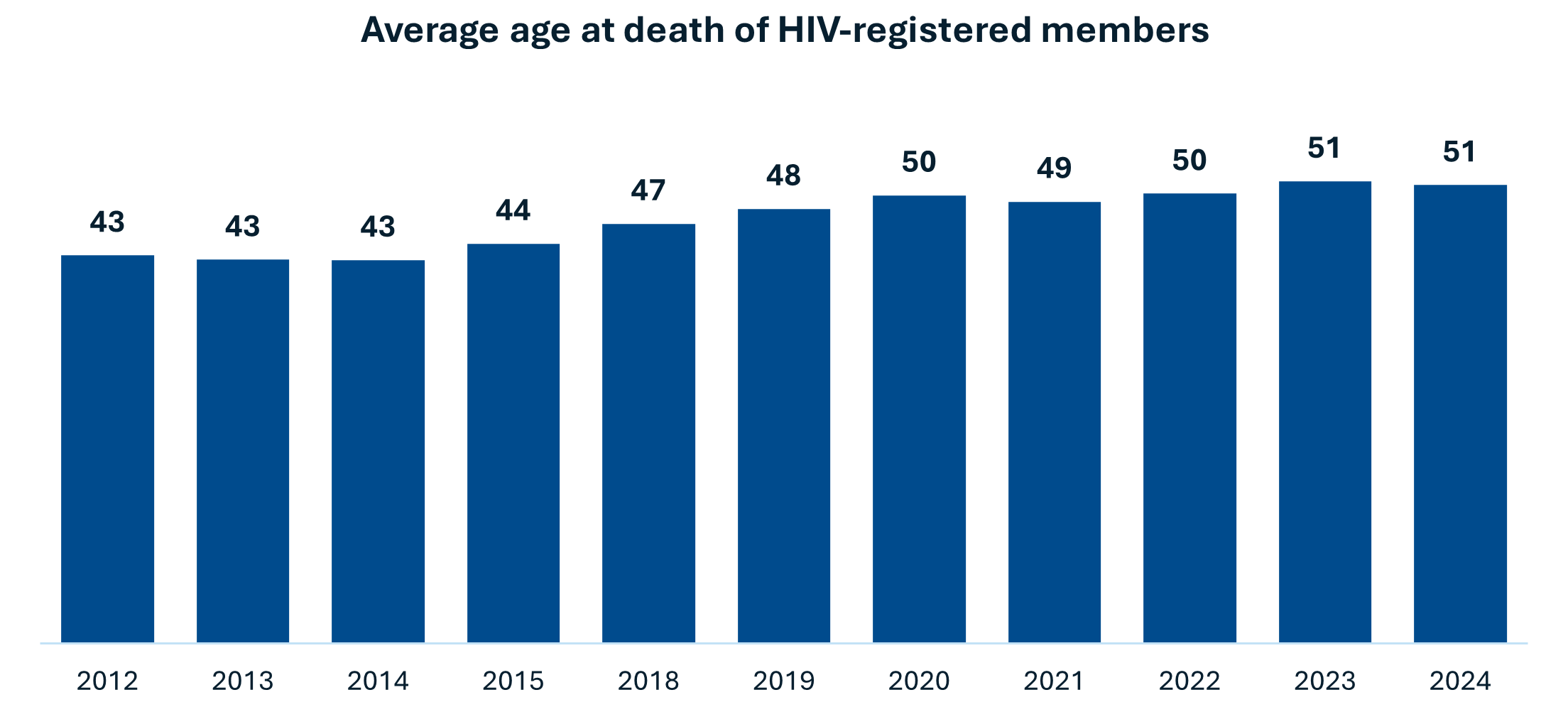
Figure 3: Average age at death for HIV‑registered members on DHMS from 2012 to 2024
What were the leading causes of death for HIV‑registered members?
Figure 4 shows that in 2012, 73% of deaths among HIV‑registered members were attributable to HIV‑related causes. This declined to 50% by 2024. Over the same period, non‑communicable diseases (NCDs) emerged as a growing cause of death for this group, increasing from 23% to 32% by 2024. The changing mortality profile underscores shifting health dynamics among HIV‑registered members, emphasising the need for a broader focus on chronic disease management alongside HIV care.
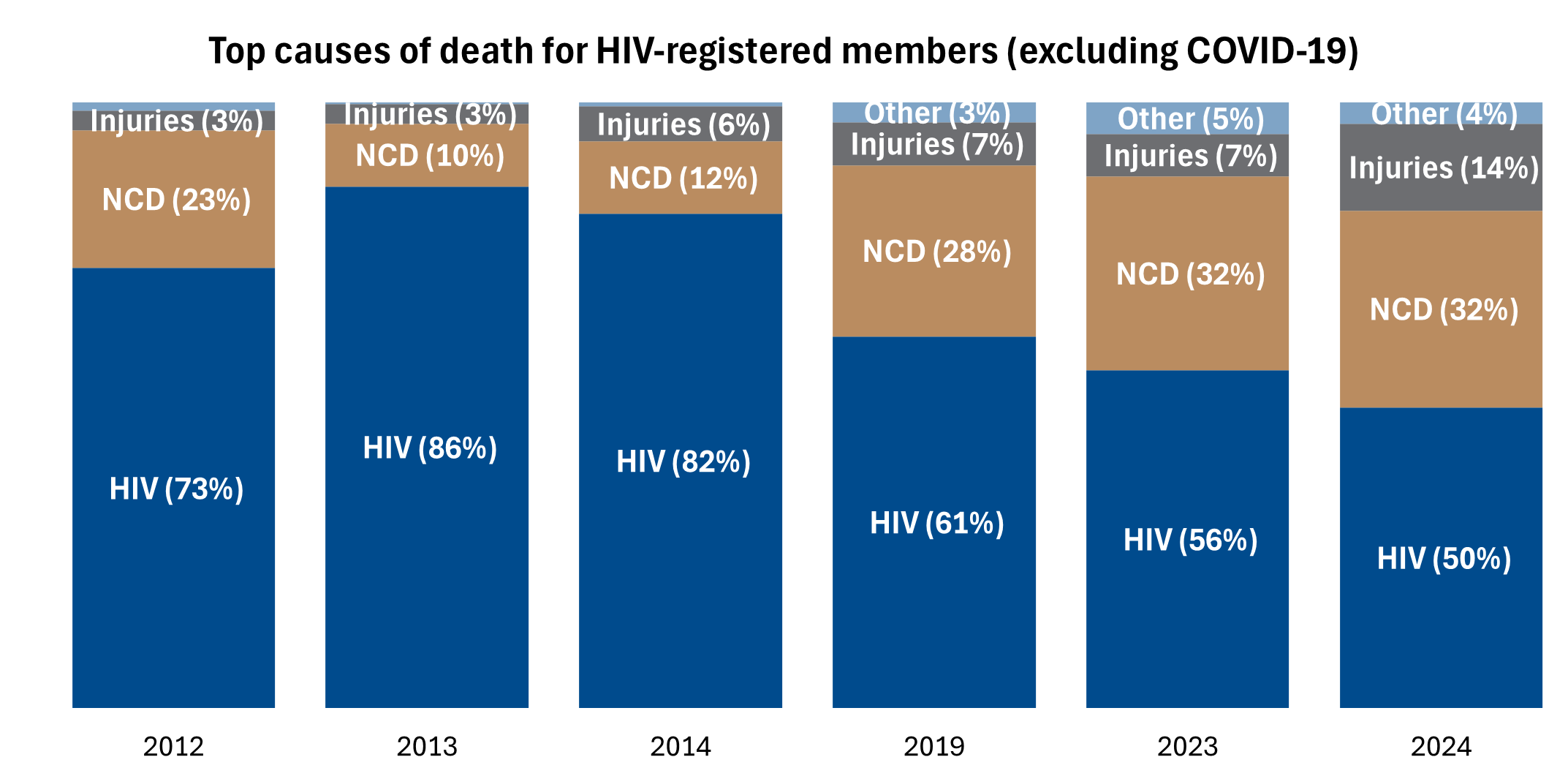
Figure 4: Top causes of death for HIV‑registered members (excluding COVID‑19) from 2012 to 2024
Factors influencing HIV mortality rates
The reduction in HIV‑related mortality rates is closely associated with improvements in several HIV management protocols. To better understand the factors influencing mortality among HIV‑registered members, statistical modelling was applied. The Cox proportional hazards model was used to examine the relationship between time to death and various explanatory variables. In this context, the event of interest is the time to death among HIV‑registered members over the 13‑year period from 2012 to 2024. After adjusting for age and sex, the model evaluates the relative impact of antiretroviral therapy (ART) possession ratio, viral load levels, line of treatment, and the presence of NCDs on mortality risk. We discuss each factor separately below.
(i) Antiretroviral therapy (ART) possession ratio
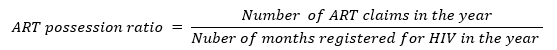
What is the Antiretroviral therapy (ART) possession ratio?
The ART possession ratio is a measure of adherence based on prescription refill claims. We have calculated the ART possession ratio as the number of ART claims a member has in a year divided by the number of months that the member is registered for HIV in a year. We classify a high possession ratio as greater than 75% and a low possession ratio as 75% or less. This threshold is supported by findings from a Namibian study, which showed that an ART possession ratio below 75% was significantly associated with virologic failure (≥5,000 copies/mL).
The following are limitations of using the ART possession ratio as a measure of adherence:
- Uses information from claims data indicating members are on treatment
- Does not consider other sources of treatment, such as employer onsite clinics, NGOs, the state, or out‑of‑pocket payments
- Early prescription refills can artificially inflate the ART possession ratio
- Does not account for whether members take the medicine as prescribed, only that they have claimed for it
Consistent adherence to ART is essential for achieving viral suppression, where the virus becomes undetectable and less likely to cause harm or be transmitted to others.
The Cox proportional hazard model shows that HIV‑registered members with a low ART possession ratio have a 22% higher risk of death compared to those with a high ART possession ratio, and this difference was statistically significant (Figure 5). This strong association emphasises the importance of consistent ART usage in reducing mortality risk.
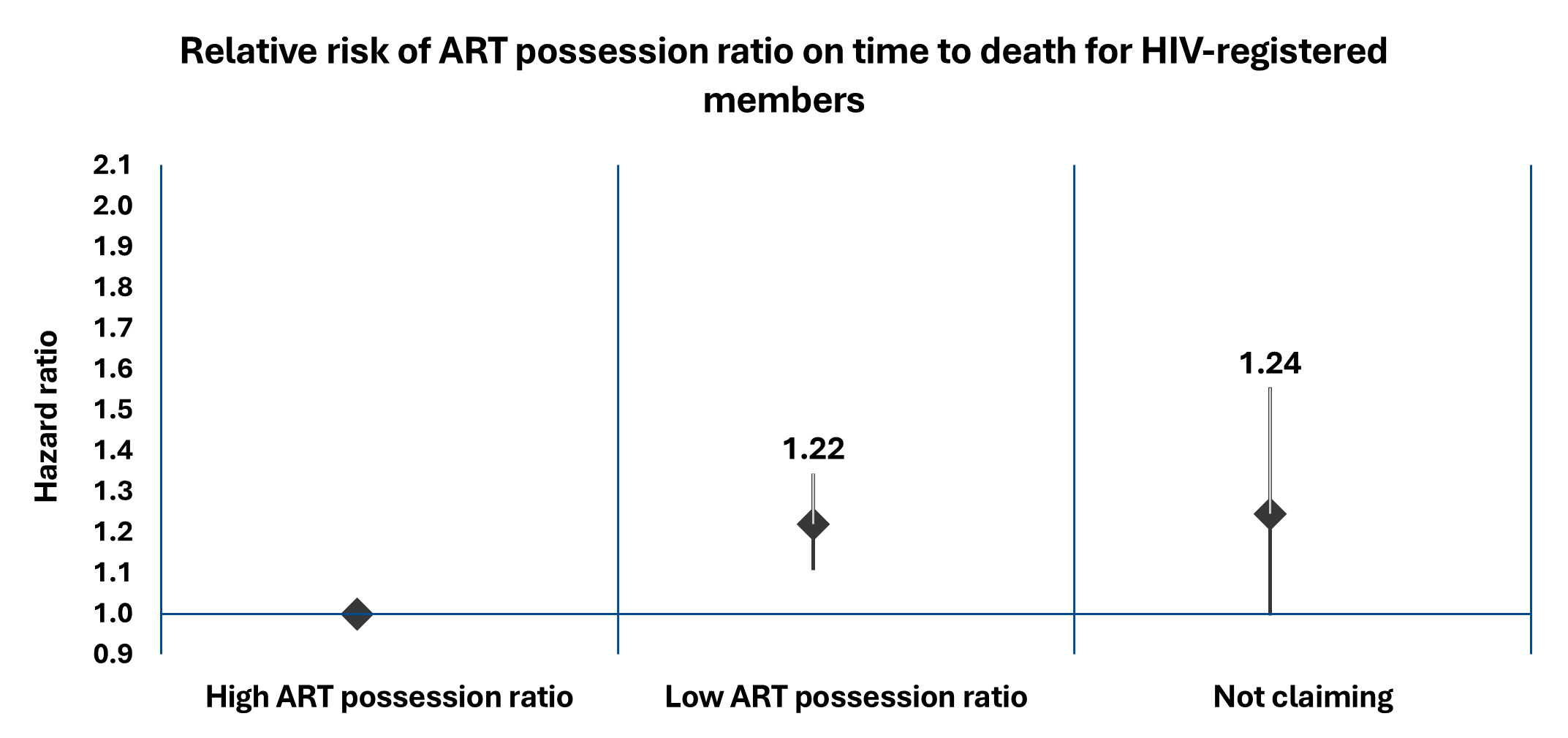
Figure 5: The relative risk of the level of ART possession on time to death for HIV‑registered members from 2012 to 2024
(ii) Viral load testing among HIV‑registered members
Viral load testing measures the level of virus present in the blood and is crucial for monitoring the effectiveness of ART. Lower viral loads are associated with better health outcomes and a reduced risk of transmission.
Figure 6 shows that there has been a 20% increase in the proportion of HIV‑registered members with an undetectable viral load (<50 copies/mL) from 2012 to 2024 (65% vs 85%) and a 16% decrease with an uncontrolled viral load (>1,000 copies/mL) over the same period (23% vs 7%). This increase in the proportion of registered HIV members with an undetectable viral load indicates that there is an improvement in the management of HIV.
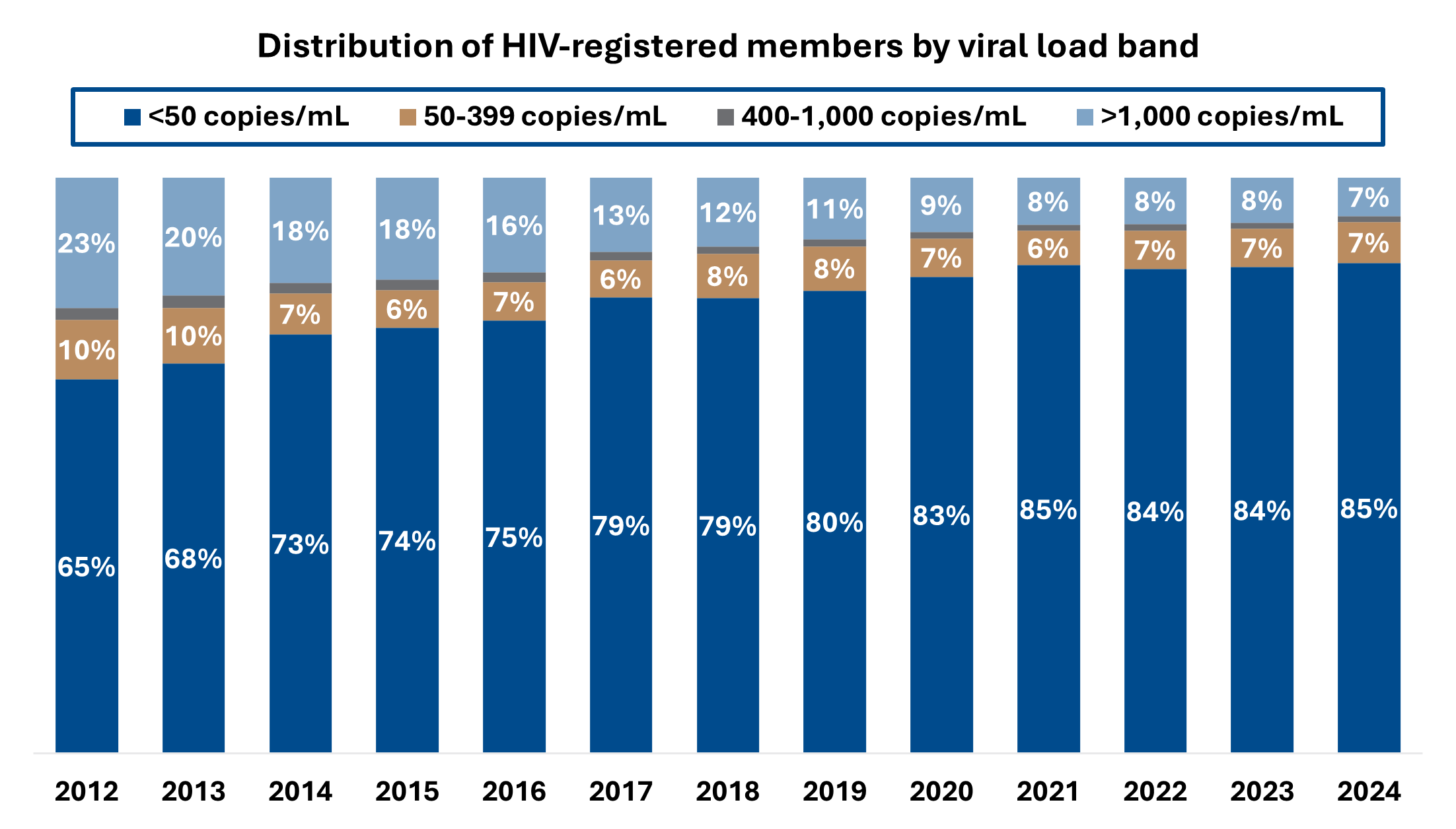
Figure 6: Proportion of HIV‑registered members by viral load band from 2012 to 2024
Half of our registered members for HIV take less than six months to achieve an undetectable viral load (VL <50 copies) after starting ART (Figure 7). As the duration on ART increases, the likelihood of achieving and maintaining an undetectable viral load also rises. This is because consistent and prolonged use of ART helps to suppress HIV more effectively over time, improving the chances of reaching and sustaining undetectable viral load levels. After two years on ART, 85% of HIV‑registered members on ART have an undetectable viral load (Figure 7).
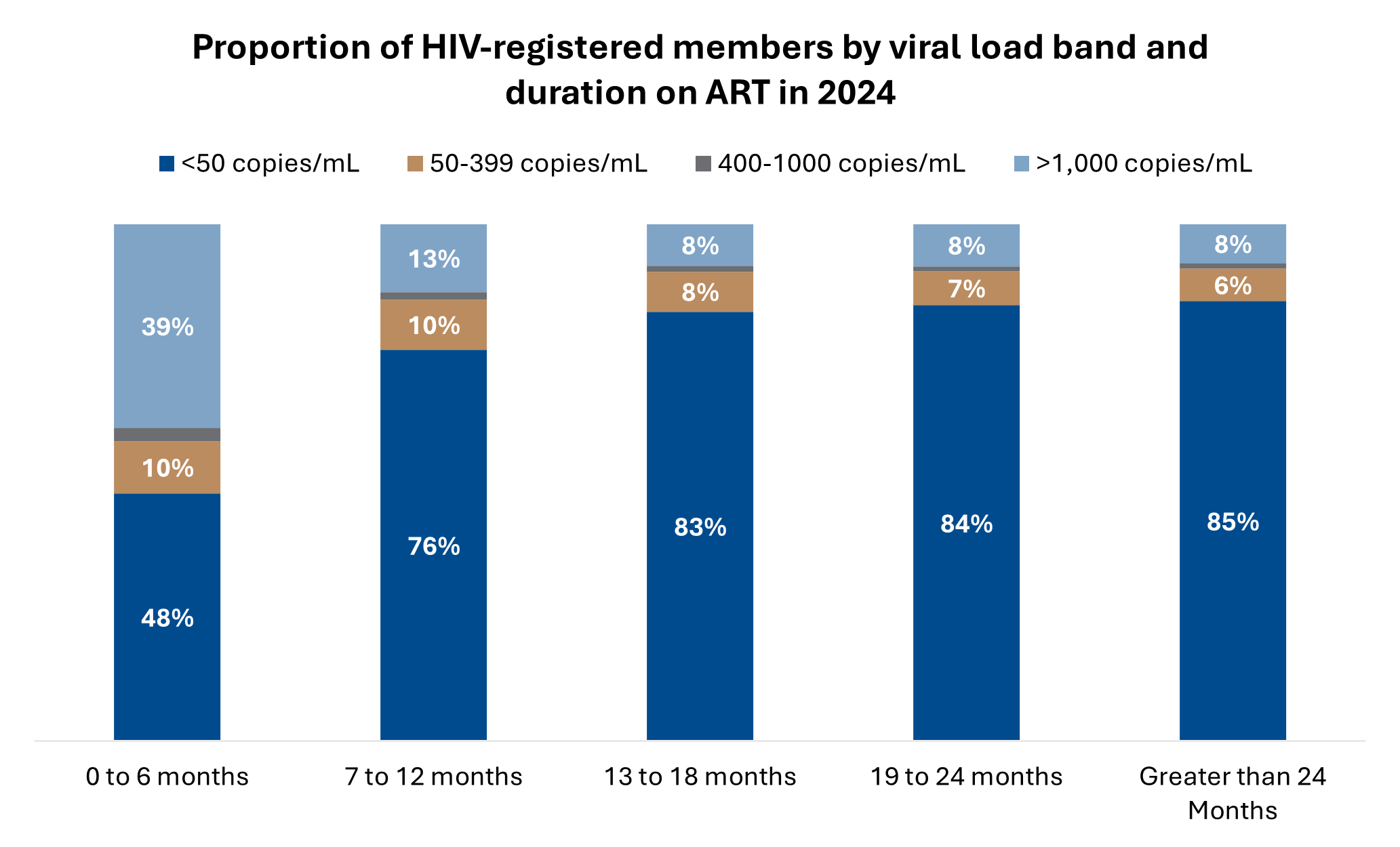
Figure 7: Proportion of HIV‑registered members by duration on ART and by viral load band in 2024
The WHO's consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring provide comprehensive recommendations for a public health approach to managing HIV. These guidelines emphasise the importance of viral load suppression in reducing HIV‑related morbidity and mortality.
The Cox proportional hazard model results in Figure 8 show that higher viral loads (>1,000 copies/mL) are associated with the highest risk of death, being 4.7 times greater than those with undetectable viral loads. Among the explored variables, high viral load levels have the greatest impact on increasing mortality, underscoring the critical importance of effective viral suppression in managing HIV.
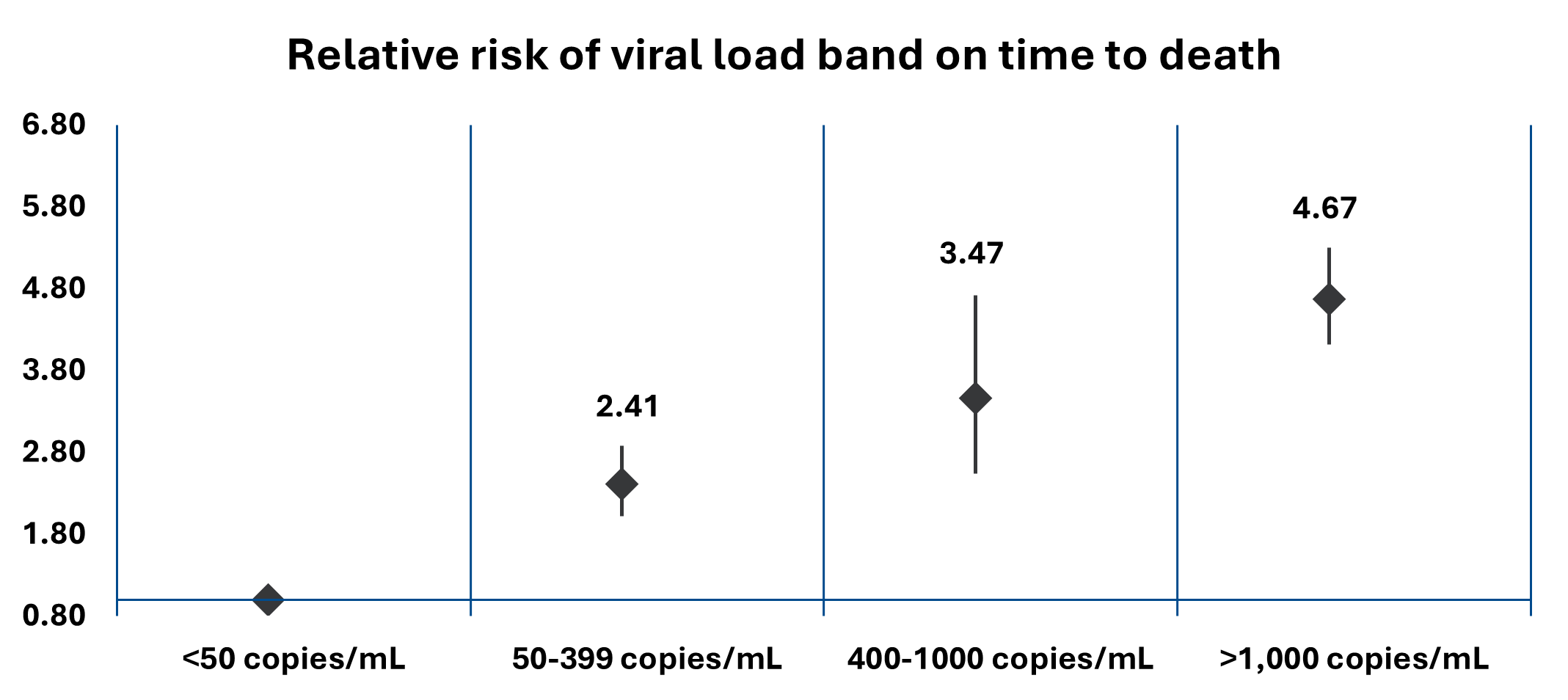
Figure 8: The relative risk of viral load levels on time to death for HIV‑registered members from 2012 to 2024
Comparing the mortality rates of HIV‑registered members with undetectable viral loads to those who are not HIV registered (adjusted for age and sex), we see that the mortality rate of HIV‑registered members with undetectable viral loads has decreased by 32% over the last 13 years (from 634 to 433 deaths per 100,000 lives) (Figure 9). The mortality rates of HIV‑registered members with undetectable viral loads are now similar to those of members not registered for HIV benefits. This highlights the effectiveness of modern HIV treatments in improving the prognosis for HIV‑registered members, enabling them to achieve health outcomes comparable to those of the general population.
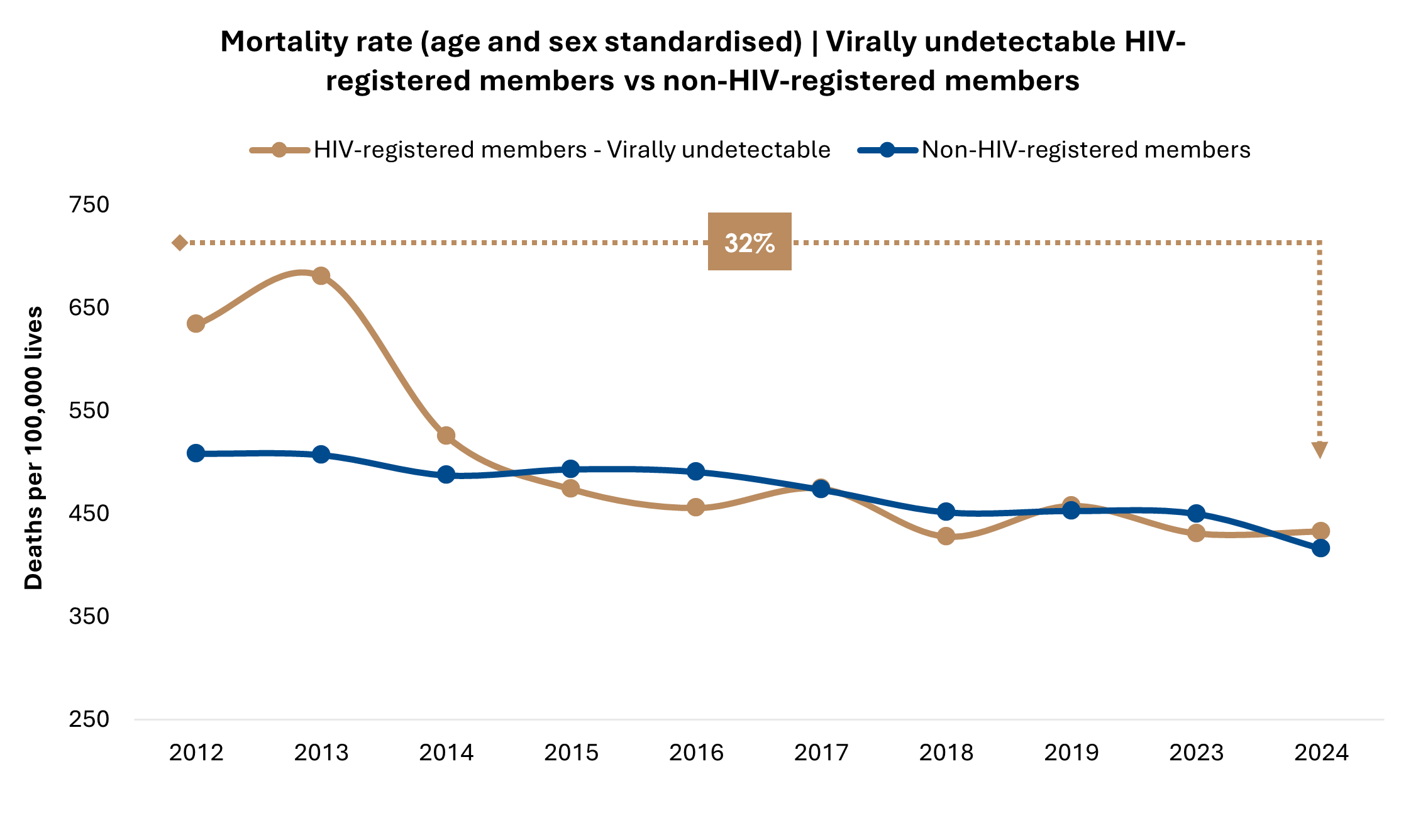
Figure 9: Mortality rate (after adjusting for sex and age) per 100,000 lives for non‑HIV‑registered members and HIV‑registered members with undetectable viral loads from 2012 to 2024
(iii) Treatment line
Overview: Lines of HIV treatment
HIV treatment is typically delivered in sequential lines, as recommended by the WHO. First‑line therapy involves a treatment regimen offering high efficacy and low resistance risk. If this fails, second‑ and third‑line treatments are introduced using alternative drug classes guided by resistance testing and clinical evaluation.
Over time, there has been a significant increase in the proportion of members on ART who are receiving first‑line treatment. This trend is indicative of the advancements in treatment protocols and the improved effectiveness of first‑line therapies. Figure 10 shows that the proportion of HIV‑registered members on first‑line treatment had an absolute proportion increase of 15.5% (71.1% vs 86.6%) and the proportion of HIV‑registered members on third‑line treatment decreased by 0.5% (1.7% vs 1.2%) from 2012 to 2024.
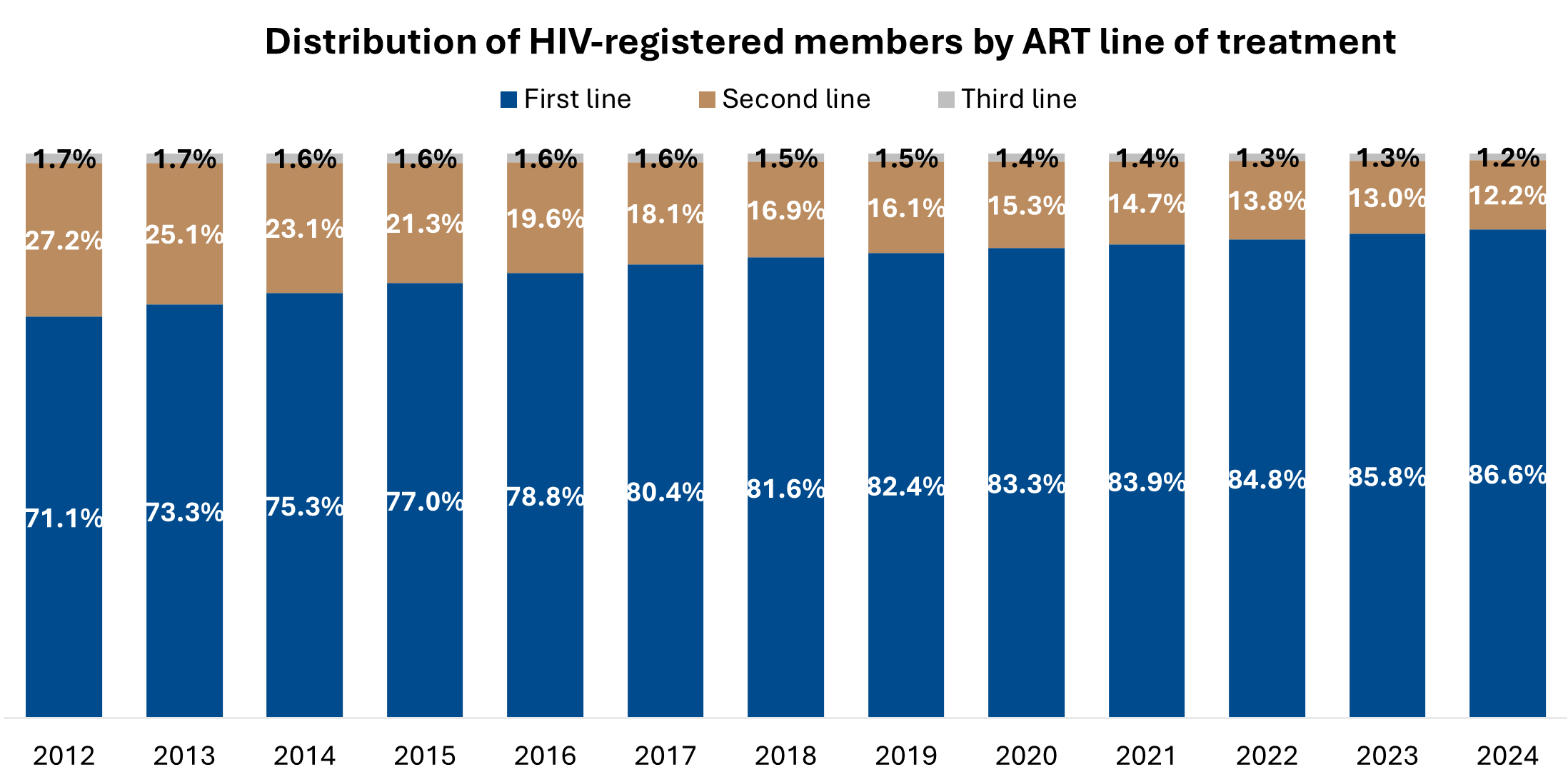
Figure 10: Proportion of HIV‑registered members by ART treatment line from 2012 to 2024
Members on third‑line ART experience a 2.7 times higher risk of death compared to those on first‑line ART (Figure 11). This elevated risk highlights the severe challenges faced by those requiring third‑line therapy, which may stem from significant drug resistance or complications arising from long‑term HIV infection.

Figure 11: The relative risk of ART treatment line on time to death for HIV‑registered members from 2012 to 2024
(iv) Non‑communicable disease (NCD) prevalence
Noncommunicable diseases (NCDs), also referred to as chronic diseases, are typically long lasting and their development is due to a combination of genetic, physiological, environmental and behavioural factors. These conditions are not passed from person to person and often progress slowly over time. The major types of NCDs defined by the World Health Organisation include cardiovascular diseases, such as heart attacks and strokes; various forms of cancer; chronic respiratory diseases, including asthma and chronic obstructive pulmonary disease (COPD); and diabetes. These illnesses represent a significant global health challenge due to their prevalence and long‑term impact on individuals and healthcare systems.
The proportion of HIV‑registered members with NCDs among HIV‑registered members over time increased from 13% in 2012 to 32% in 2024. This is a 2.5 times higher prevalence over this 13‑year period (Figure 12).

Figure 12: Distribution of HIV‑registered members with NCDs from 2012 to 2024
From Figure 13, we see that NCD prevalence increases sharply by age. However, NCD prevalence is similar between HIV‑registered and non‑HIV‑registered members at all ages in 2024.
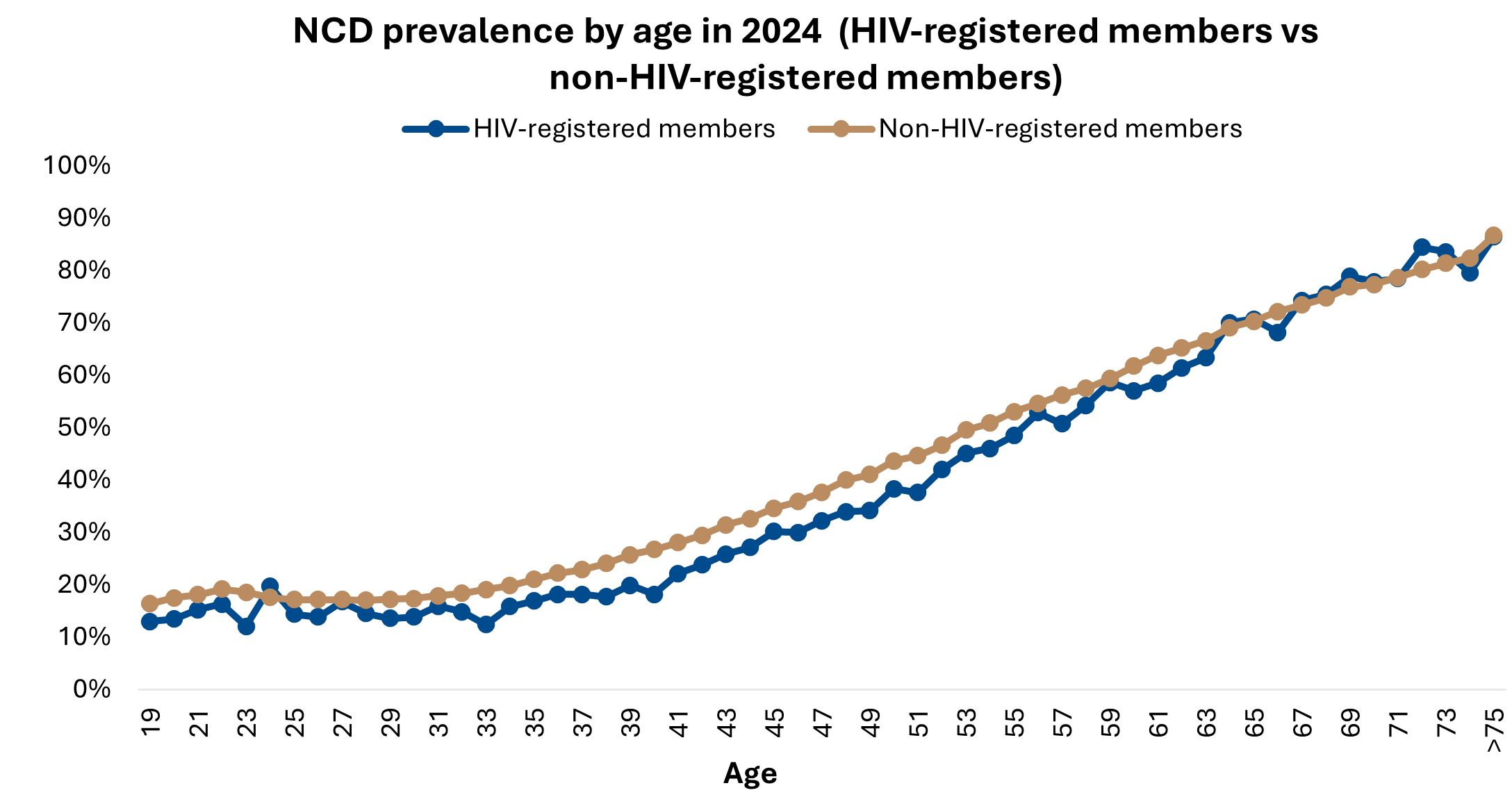
Figure 13: NCD prevalence in HIV‑registered and non‑HIV‑registered members by age in 2024
Cox proportional hazard modelling results show that HIV‑registered members with NCDs have a 60% higher risk of death compared to those without NCDs, highlighting the strong association between NCDs and increased mortality risk among HIV‑registered members (Figure 14).
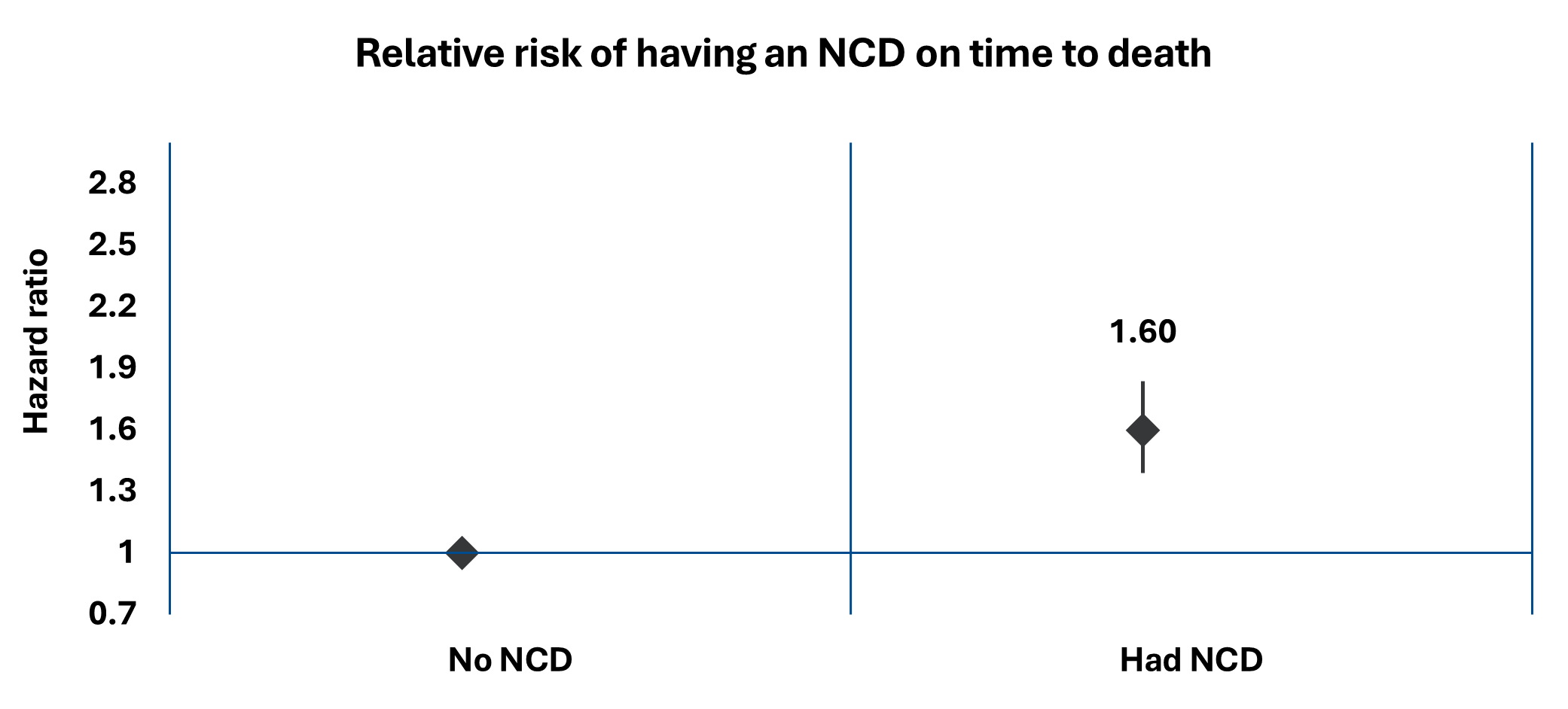
Figure 14: The relative risk of having an NCD on time to death for HIV‑registered members from 2012 to 2024
Conclusion
From 2012 to 2024, mortality rates for DHMS members who are registered for HIV have improved, reflecting significant progress in managing HIV as a condition and improving the life expectancy of those living with HIV.
The proportion of deaths attributable to HIV‑related causes also decreased, while non-communicable diseases (NCDs) emerged as a growing cause of death, highlighting the need for a broader focus on chronic disease management in this population.
The decrease in HIV-related mortality can be attributed to sustained adherence to antiretroviral therapy (ART) which has played a crucial role in achieving and maintaining viral load suppression. As a result, HIV registered members with undetectable viral loads now experience mortality rates similar to those not registered for HIV. This underscores the effectiveness of consistent treatment and sustained or improved adherence to treatment in improving long-term health outcomes for people living with HIV.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes. All of our COVID-related analyses are posted under our "COVID-19 Insights" pillar.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only these data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.
- Anderson, R.N., Rosenberg, H.M., 1998. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep 47, 1-16, 20 https://pubmed.ncbi.nlm.nih.gov/9796247/
- World Health Organization. Methods and data sources for country‑level causes of death 2000‑2019. Geneva: WHO, 2020
- Ferguson, N.M., Donnelly, C.A., Hooper, J., Ghani, A.C., Fraser, C., Bartley, L.M., Rode, R.A., Vernazza, P., Lapins, D., Mayer, S.L., and Anderson, R.M., 2005. Adherence to antiretroviral therapy and its impact on clinical outcome in HIV‑infected patients. Journal of The Royal Society Interface, 2(349‑363). Available at: https://www.psi.ox.ac.uk/research/copy_of_publications/675751 [Accessed 19 Feb. 2025]
- World Health Organization. The role of HIV viral suppression in improving individual health and reducing transmission: policy brief (2023), ISBN 9240055177 (Electronic), 9789240055179 (PDF)
- World Health Organisation Fact Sheet Non Communicable Diseases https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- World Health Organization (2019). Update of recommendations on first‑ and second‑line antiretroviral regimens (WHO/CDS/HIV/19.15). Geneva: World Health Organization. Retrieved from https://iris.who.int/bitstream/handle/10665/325892/WHO‑CDS‑HIV‑19.15‑eng.pdf
- World Health Organization (2016). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach (2nd ed).
Available at: https://iris.who.int/handle/10665/208825 - Hong SY, Jerger L, Jonas A, Badi A, Cohen S, et al. (2013). Medication Possession Ratio Associated with Short‑Term Virologic Response in Individuals Initiating Antiretroviral Therapy in Namibia. Medication Possession Ratio Associated with Short‑Term Virologic Response in Individuals Initiating Antiretroviral Therapy in Namibia. PLOS ONE 8(2): e56307. https://doi.org/10.1371/journal.pone.0056307