Part 2 of 3: Thirteen year longitudinal analysis of mental health condition trends among Discovery Health Medical Scheme members, focusing on population health

In this second article of our three part series, we continue to unpack the trends in mental health conditions among Discovery Health Medical Scheme (DHMS) members. In part one, we looked at the rise in prevalence and incidence of mental health conditions and the relationship with chronic conditions. This article considers the unique opportunities for managing mental health based on the demographics of members living with these conditions.
Authors
Discovery Health Intelligence Team members Katherine Tregoning (Actuary), Claudia Pastellides (Actuary), Cassi Rubin (Head: Mental Health Risk), Lara Wayburne (Chief Health Intelligence Actuary)
Overview
We explore how mental health conditions vary across gender, age and family structure among members of the Discovery Health Medical Scheme. In 2024, women made up 62% of those living with mental health conditions. This pattern was consistent over the 13‑year period of our analysis and reflects global findings. Depression, bipolar mood disorder, anxiety disorder and parasomnias are more prevalent among women, while ADHD and developmental disorders are more common in men. Women are also more likely to seek professional help and claim for psychiatric medicine.
Young adults aged 18 to 24 have seen the sharpest rise in mental health conditions, with prevalence more than doubling since 2012. Treatment patterns differ by age: younger people are more likely to consult professionals, while older members rely more on medicine.
Family structure also plays a role. Members on single policies show higher rates of mental health conditions, possibly linked to isolation. Children in families where an adult has depression are five times more likely to be diagnosed themselves.
Recognising the influence of demographic and familial factors on mental wellbeing is helping Discovery Health Medical Scheme to tailor its mental health benefits with both precision and personalisation in mind.
Mental health patterns and gender
There is a clear disparity in the burden of mental health conditions between female and male members in the Discovery Health Medical Scheme (DHMS), with 62% of the population with mental health conditions in 2024 being female. Our registration and claims data show that mental health conditions were 45% more prevalent in females than in males (18.1% for females vs 12.4% for males in 2024, Figure 1). The prevalence of mental health conditions has increased slightly faster among females at 49% from 2012 to 2024, compared to a 47% prevalence increase in males. This gap has stayed consistent over time and aligns with international literature, which shows females are more likely to be diagnosed with a mental health condition or seek mental health care.1
1 https://pmc.ncbi.nlm.nih.gov/articles/PMC2810067/
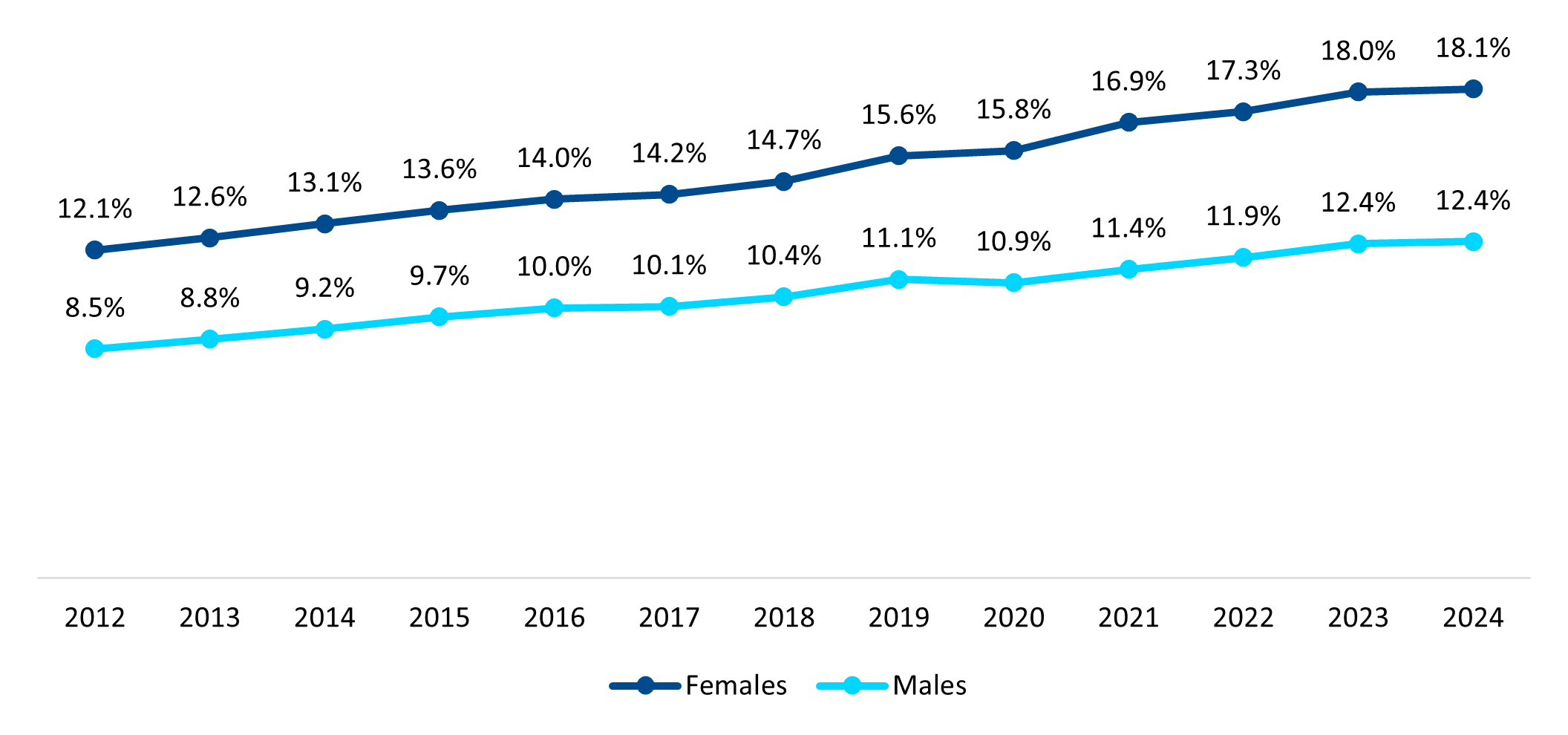
Figure 1: Prevalence of mental health conditions in DHMS by gender
The top six most prevalent mental health conditions that were registered or claimed for by DHMS members in 2024 were depression, bipolar mood disorder, attention deficit hyperactivity disorder (ADHD), parasomnias, anxiety, and developmental and learning disorders. The profiles of the members living with these conditions vary depending on the condition. As shown in Figure 2, most members with depression, anxiety, bipolar mood disorder or parasomnias were female, and this has stayed consistent over time. In contrast, a smaller proportion of members who register or claim for ADHD (39%) or developmental and learning disorders (41%) were female.
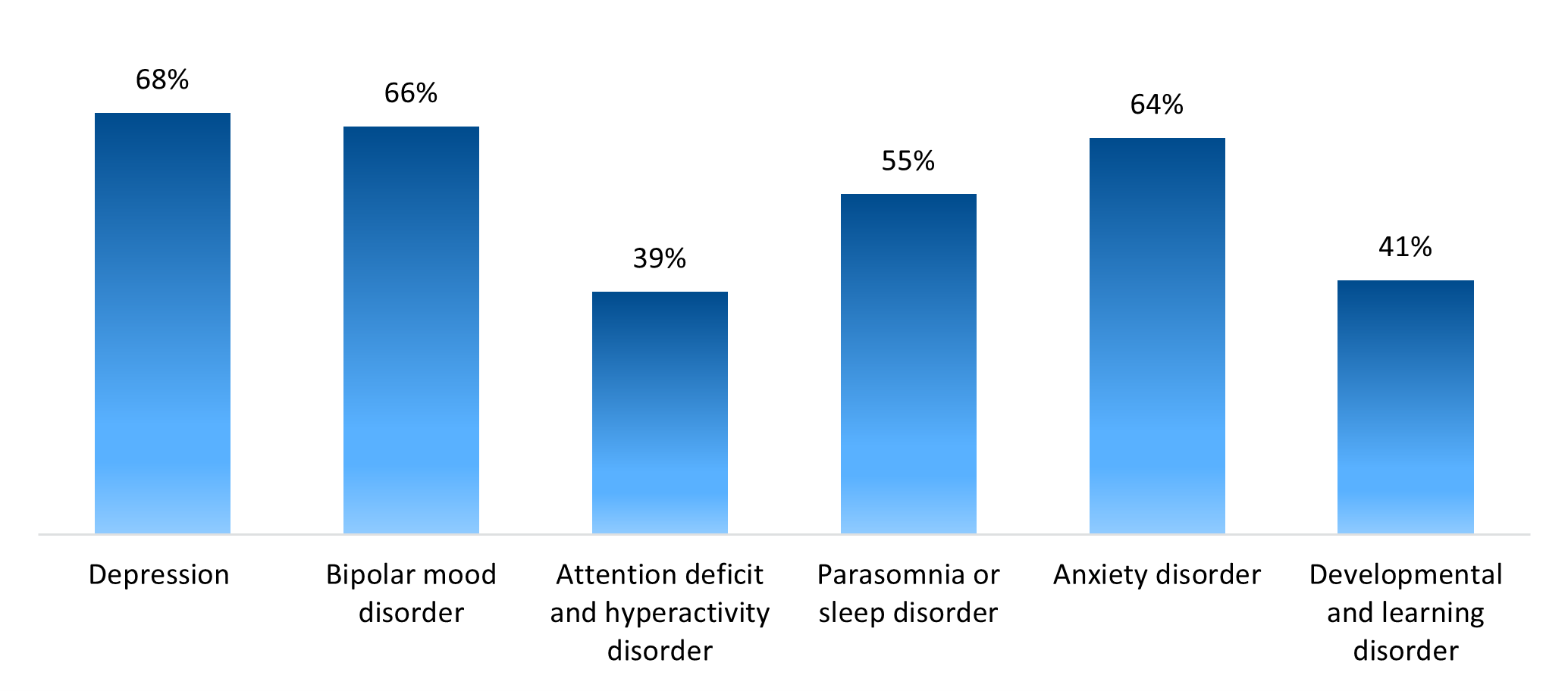
Figure 2: Proportion of females in the top six most prevalent mental health conditions in 2024 in DHMS
Regarding health‑seeking behaviour by gender, Figure 3 shows that 52% of females claimed for antidepressant or antipsychotic medicine, compared to only 41% of males.
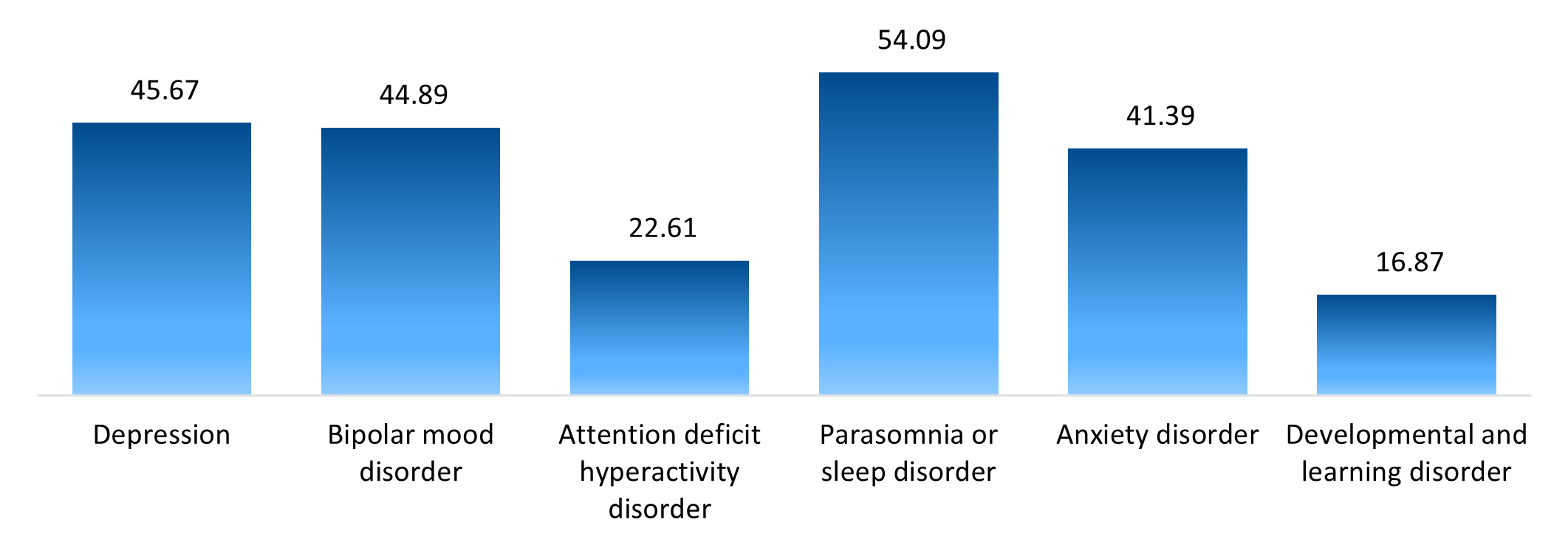
Figure 3: Mental health interventions and the proportion of 2024 mental health condition claimants by gender
Trends by age group
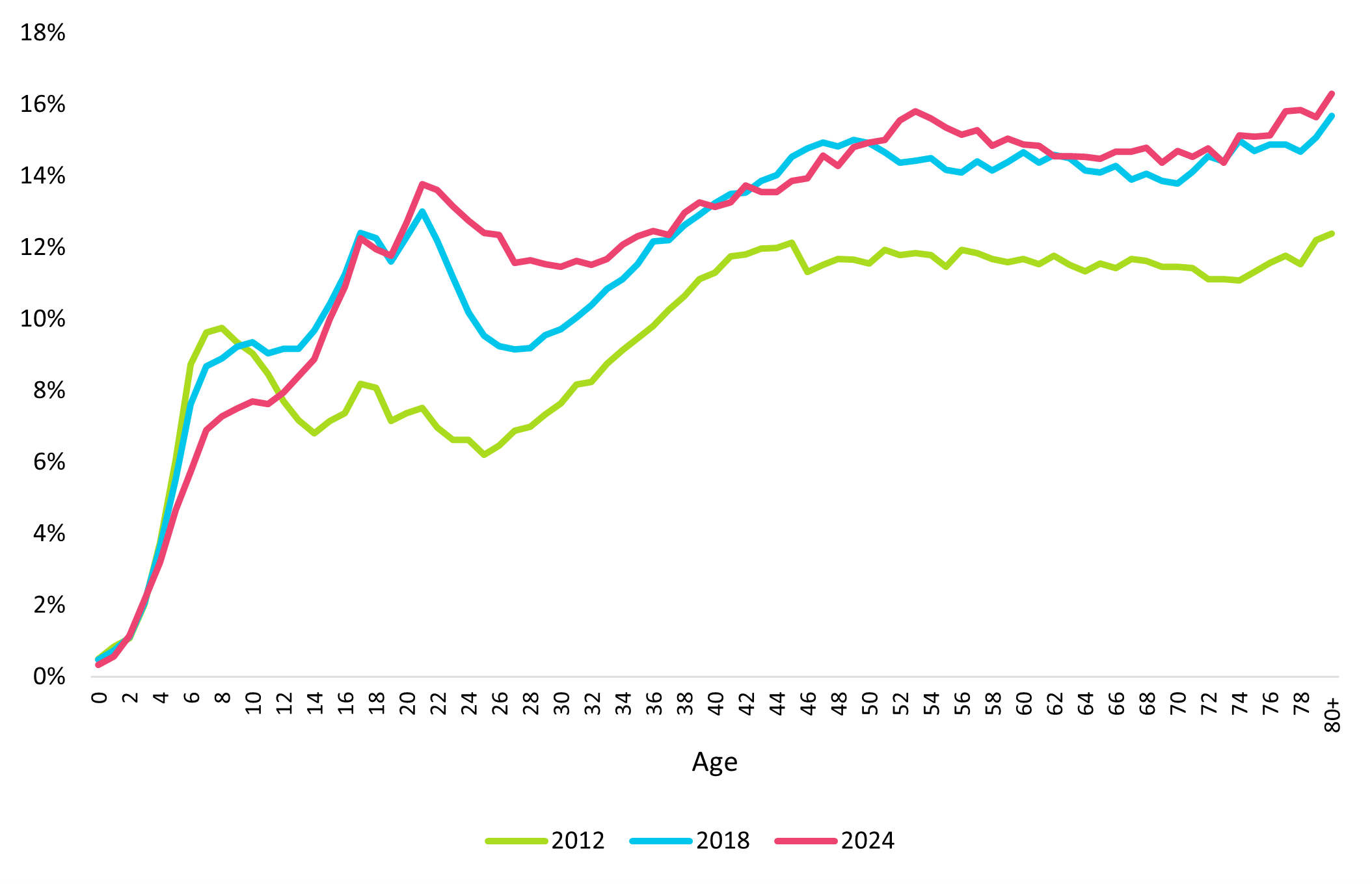
Figure 4 shows the prevalence of mental health conditions in DHMS members split by age from 2012 to 2024. There is a noticeable spike in the number of young adults (ages 18 to 24) registering or claiming for a mental health condition, with the prevalence of mental health conditions in this age group more than doubling since 2012
Trends in prevalence by age differ across the registered or claimed‑for mental health conditions, as shown in Figure 5. In 2024, members who claimed or registered for depression were on average 45.6 years old; however, members who claimed or registered for ADHD and developmental and learning disorders were younger (22.6 years old and 16.8 years old respectively).
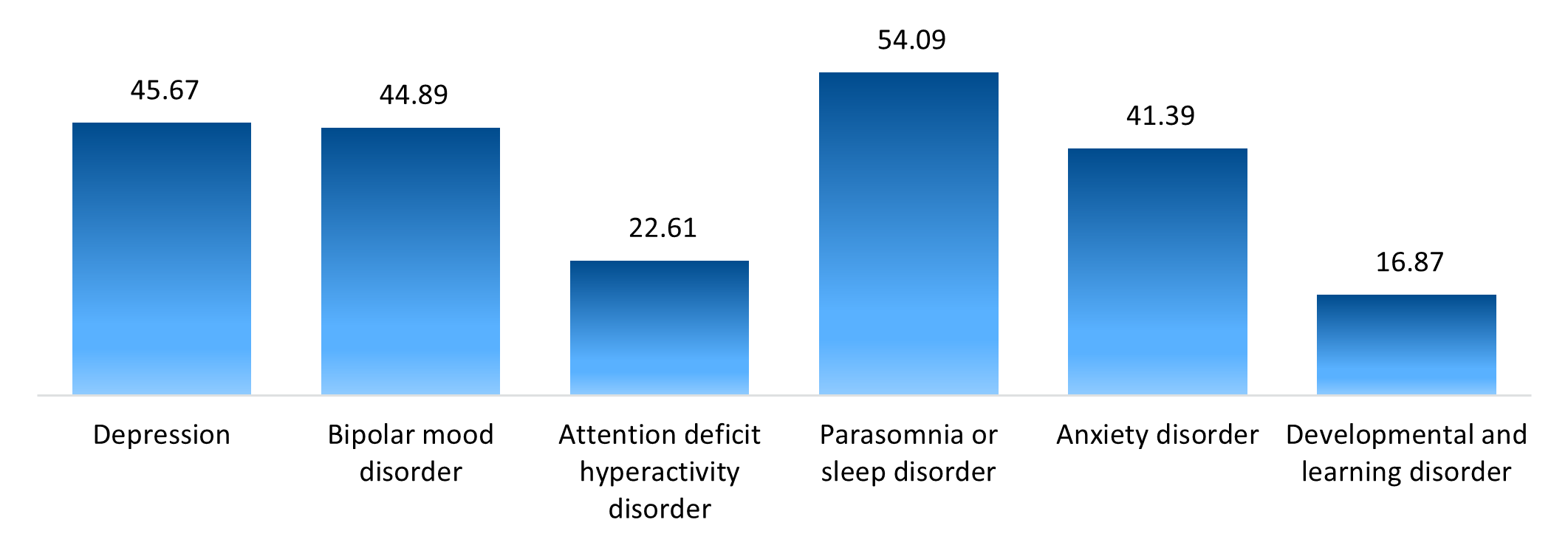
Figure 5: Average age for the top six most prevalent mental health conditions in 2024
Figure 6 shows how the age groups use mental health interventions differently. Of young adults (aged 20 to 29) who had a claim associated with a mental health episode of care in 2024:
- 71% consulted a psychologist, general practitioner or psychiatrist
- 44% claimed for antidepressant or antipsychotic medicine
- 8% had a hospital admission related to mental health.
Of the members older than 75 years who had a claim related to mental health:
- 31% consulted a professional
- 61% claimed for medicine
- Only 2% were admitted to hospital.
This shows that health‑seeking behaviour in the mental health population differs by age, with younger members claiming more for psychotherapy and older members claiming more for mental health‑related medicine.
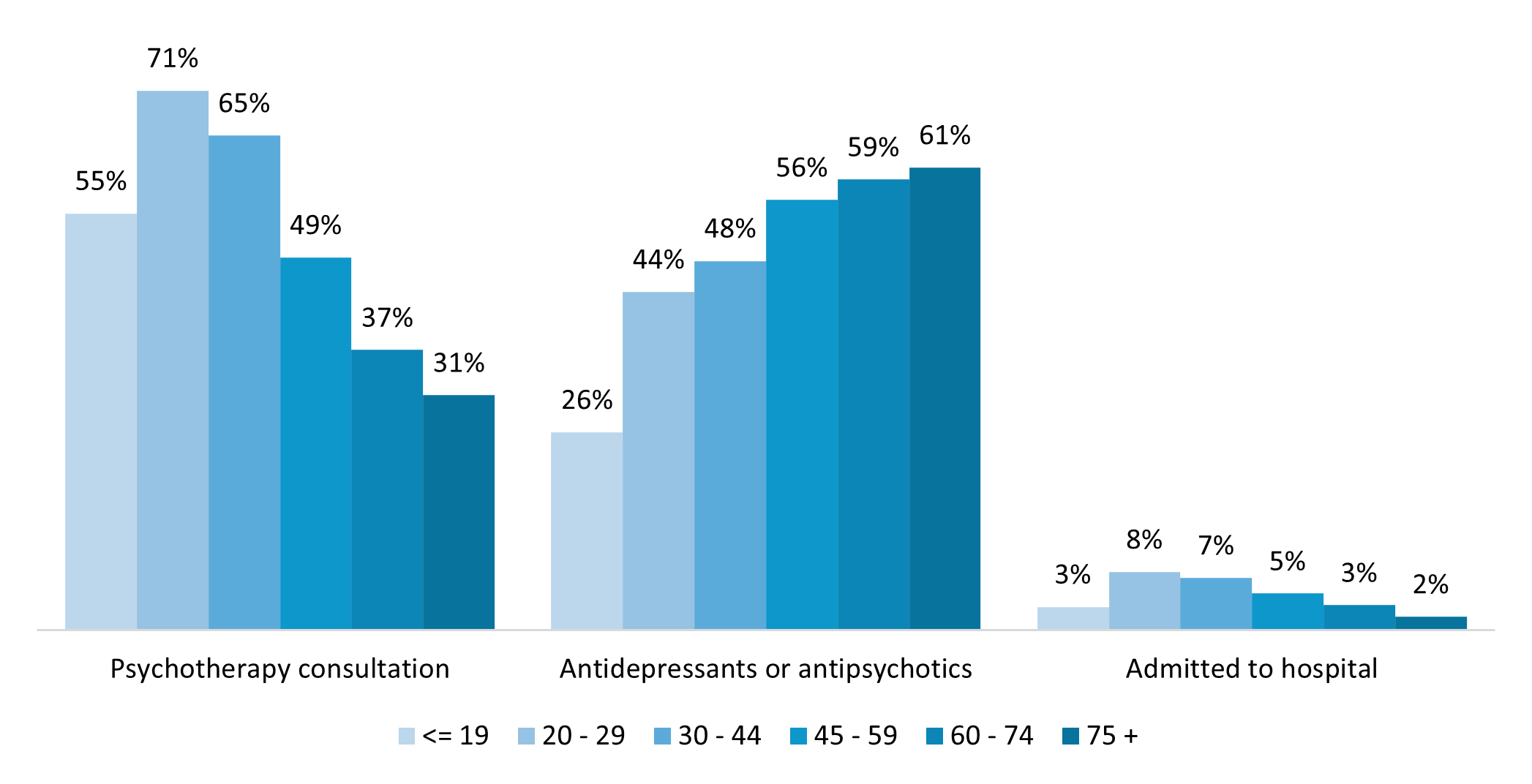
Figure 6: Proportion of 2024 mental health interventions by age group
Family size and mental wellbeing
Family size is decided by the number of beneficiaries listed on a DHMS policy. Figure 7 shows that mental health conditions were more prevalent among members with single policies compared to those with larger policy sizes. In 2024, single policies had 1.38 times higher prevalence of mental health conditions compared to policies with four or more people (16.29% for single family size vs 11.82% for family of four, Figure 7). This observation is influenced by age: young adults are often on a single policy, while older members and children are typically part of larger policy sizes. Loneliness and isolation are known clinical triggers for a mental health episode, and family size is a useful indicator of a mental health condition depending on whether there are supportive relationships within the family.2
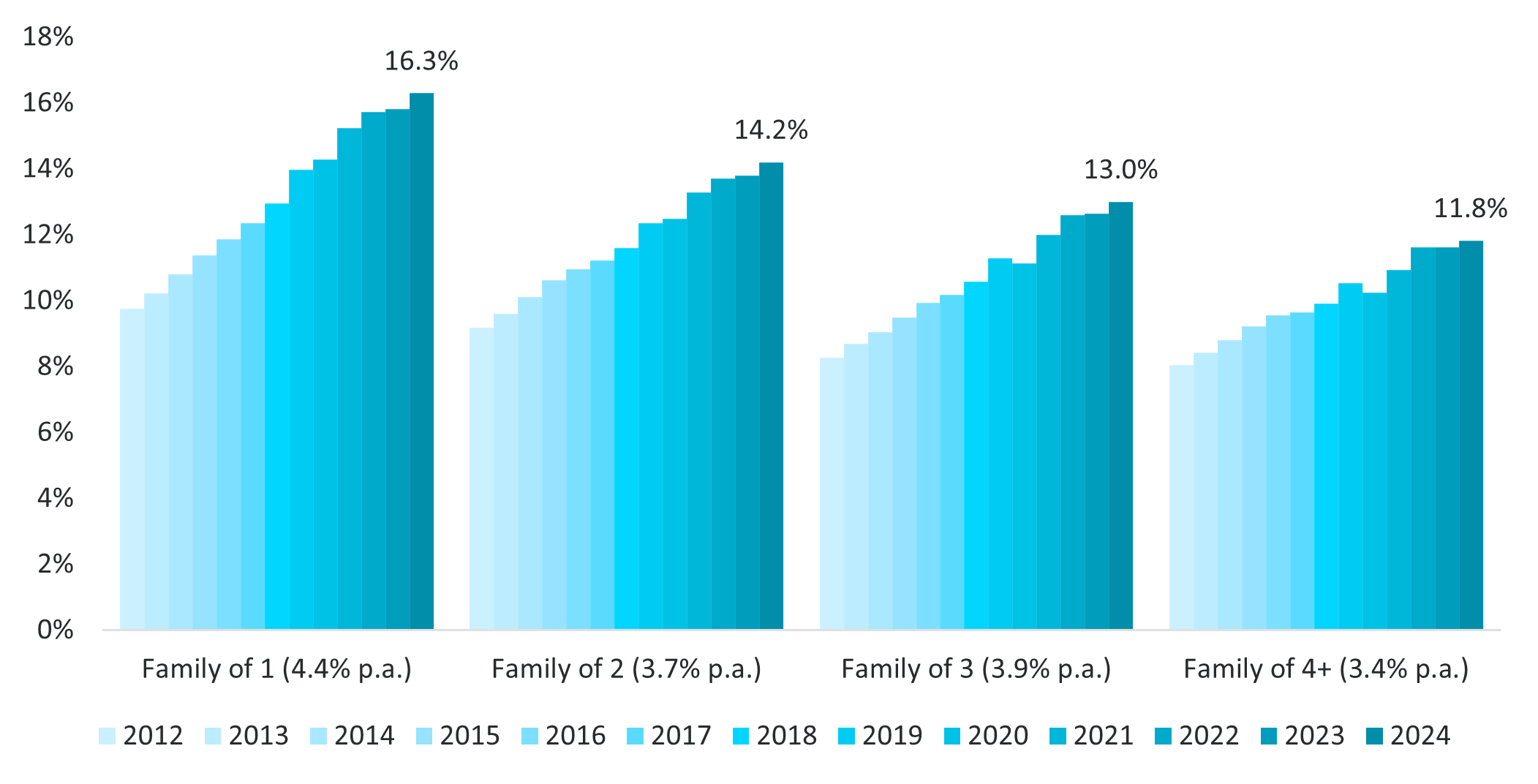
Figure 7: Prevalence of mental health conditions in DHMS members with a mental health condition by policy size (used as a proxy for family size) compared to 2012
Familial mental health data
In 2024, in families with adults who were diagnosed with depression, the prevalence of depression in child dependants was five times higher than for children where there was no existing adult depression diagnosis in their family (15% vs 3% respectively, Figure 8). This shows that a mental health condition in the family may increase a child's likelihood of claiming for one. Figure 8 highlights the growing probability over time of a child dependant being diagnosed with depression if an adult on the same policy has depression. Notably, this is on the rise since the beginning of the COVID‑19 pandemic.
2https://www.thelancet.com/pdfs/journals/lanpub/PIIS2468-2667(19)30230-0.pdf
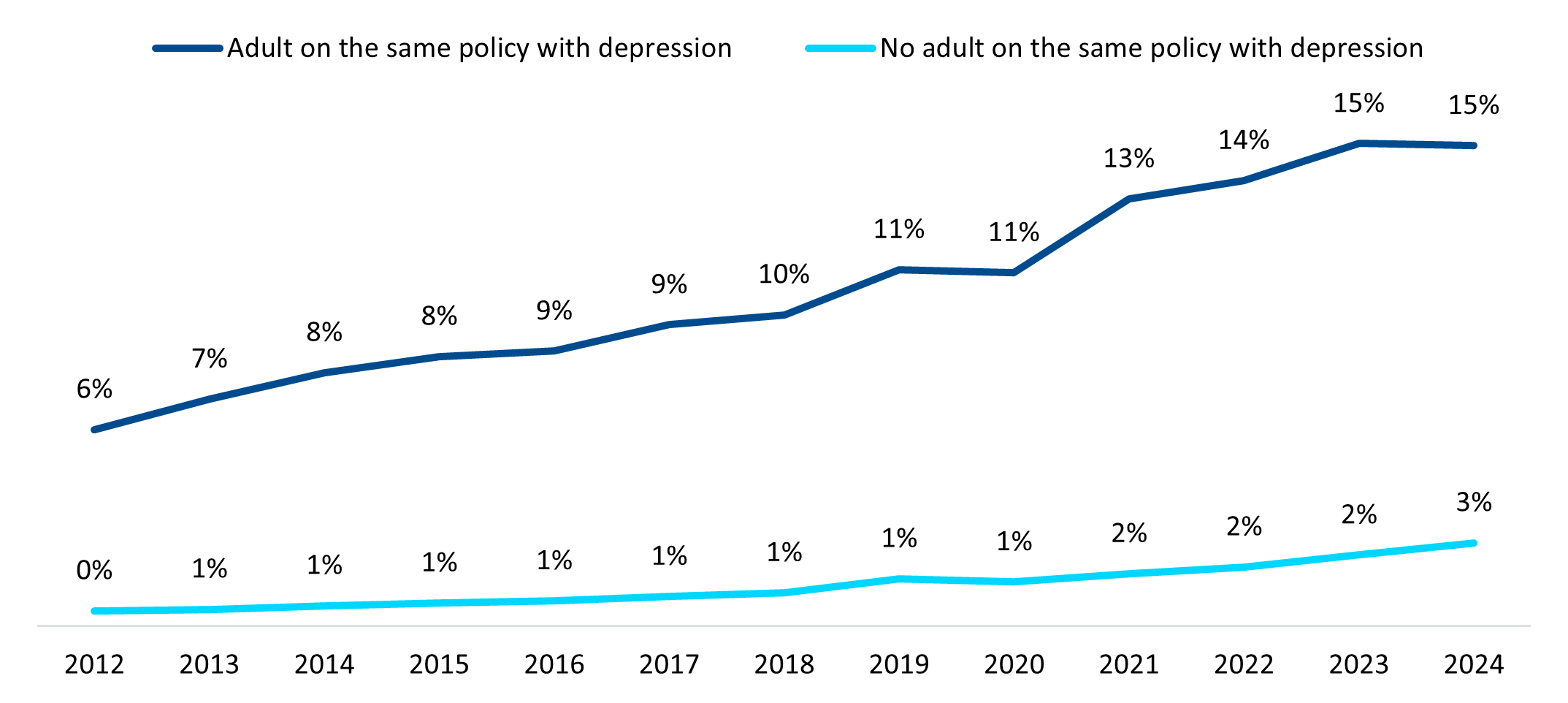
Figure 8: Prevalence of depression in children by depression status of adults on the same policy
Conclusion
The demographic profile of Discovery Health Medical Scheme members varies depending on the type of mental health condition they claim or register for, as well as the type of mental health intervention they use. Mental health conditions are more prevalent among females and those with single member policies. Over the past decade, there has been a notable increase in mental health condition prevalence among young adults. The prevalence of depression is higher among children in families that have an adult living with depression compared to children in families that don't.
An increasing proportion of Discovery Health Medical Scheme members continues to register for mental health conditions each year. The unique trends we've identified help us to design hyper‑personalised benefits for members in the mental health condition population. We'll explore this dynamic response in part three. And, if you missed part one in this three‑part series, read it here.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes. All of our COVID-related analyses are posted under our "COVID-19 Insights" pillar.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only these data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.