15-year analysis shows chronic kidney disease has significant effects on the Discovery Health Medical Scheme and its members

Chronic kidney disease (CKD) affects around 10% of the global population, and just over 8000 Discovery Health Medical Scheme (DHMS) members. This analysis spans 15 years' worth of DHMS data related to CKD, looking at disease stages, admission rates, healthcare costs, morbidity, and mortality rates and more. What's driven mortality rates down by almost a third over time?
Authors
Discovery Health's: Sian-Ailin Da Silva (Statistician), Lizelle Steenkamp (Senior Healthcare Statistician), Xolani Masombuka (Junior Analyst), Michael Cohen (Actuary), Claire van Rensburg (Manager of Kidney Care Programme), Dr Dave Jacobs (Senior Clinician and Clinical Classification System Architect), Shirley Collie (Chief Research Actuary)
CKD: A global priority with serious impact on people and economies
Chronic kidney disease (CKD) refers to a gradual loss of kidney function over time. Risk factors for developing CKD include having HIV, diabetes, high blood pressure, high cholesterol and more.
CKD affects 1 in 10 people worldwide or approximately 844 million people1. According to the 2010 Global Burden of Disease study (looking at total number of deaths globally from various conditions) CKD ranked 27th in 1990 but rose to 18th in 20101. By 2022, CKD was ranked the 16th leading cause of years of life lost2 and was predicted to rank fifth by the year 20403.
CKD causes significant - sometimes described as 'catastrophic'4 - burden to healthcare systems and economies, with the burden borne by developing countries. It is estimated that in developed countries, 6%6 of annual healthcare budgets is required to treat kidney disease alone.
According to the SA Medical Research Council, 'the illness disproportionately affects people of African ancestry, who develop the illness at a younger age and have a more rapid progression towards kidney failure. Furthermore, kidney disease prevalence in Africa may be as high as 1 in 8 people7.
Annual health checks are key to early detection of risk factors for CKD
CKD is progressive and has largely indistinct symptoms, which means that many people are unaware they're headed for renal failure.
- According to the US Centres for Disease Control and Prevention8, as many as 9 in 10 adults who have CKD and 1 in 3 adults who have severe CKD, do not know they have this condition.
The onset of CKD is often preventable. Annual health checks are key to early detection of the risk factors for this disease. As type 2 diabetes and hypertension are two major causes of CKD, managing these diseases with lifestyle changes and treatment is key.
Advanced CKD is associated with increased risk of cardiovascular morbidity, premature mortality, and seriously decreased quality of life6. The progress to end-stage renal disease (ESRD) can be delayed with the right diagnostics and early treatments, along with appropriate lifestyle modifications.
Haemodialysis and peritoneal dialysis are commonly used treatments for the management of patients with ESRD10:
- Those on chronic haemodialysis typically require at least three sessions a week (at about four hours per session).
- Those on peritoneal dialysis (where a catheter is permanently attached to the abdomen) require dialysis for 30 to 40 minutes, four times a day, or dialysis for eight to ten hours while they sleep.
Once individuals commence dialysis, they continue until the point of kidney transplantation, or until they pass away. The costs5 of dialysis and transplantation take up to 3% of the annual healthcare budget in high-income countries.
Tracking the Discovery Health Medical Schemes' CKD landscape from 2008 to 2022
Our sample consists of the population Discovery Health Medical Scheme (DHMS) members who have been registered for CKD from 2008 to 2022.
We segmented these members into three groups:
- The pre-dialysis population
- The chronic dialysis population
- The kidney transplant population.
For each of these groups, we:
- Quantified cost and utilization impact on the Scheme
- Analysed morbidity and mortality profiles.
4.6-fold increase in incidence and 3.25-fold increase in prevalence of CKD over time
The number of DHMS members who are registered as having CKD has more than quadrupled from 2008 to 2022, from 1,747 members in 2008 to 8,113 members in 2022 (Fig. 1).
This reflects a 4.6-fold increase in incidence (absolute number of members with CKD) over the 15-year period under consideration, and a 3.25-fold increase in prevalence (the proportion of all members who have CKD at a specific point in time), from 77 per 100,000 person years to 251 per 100,000 person years - (Fig. 1).
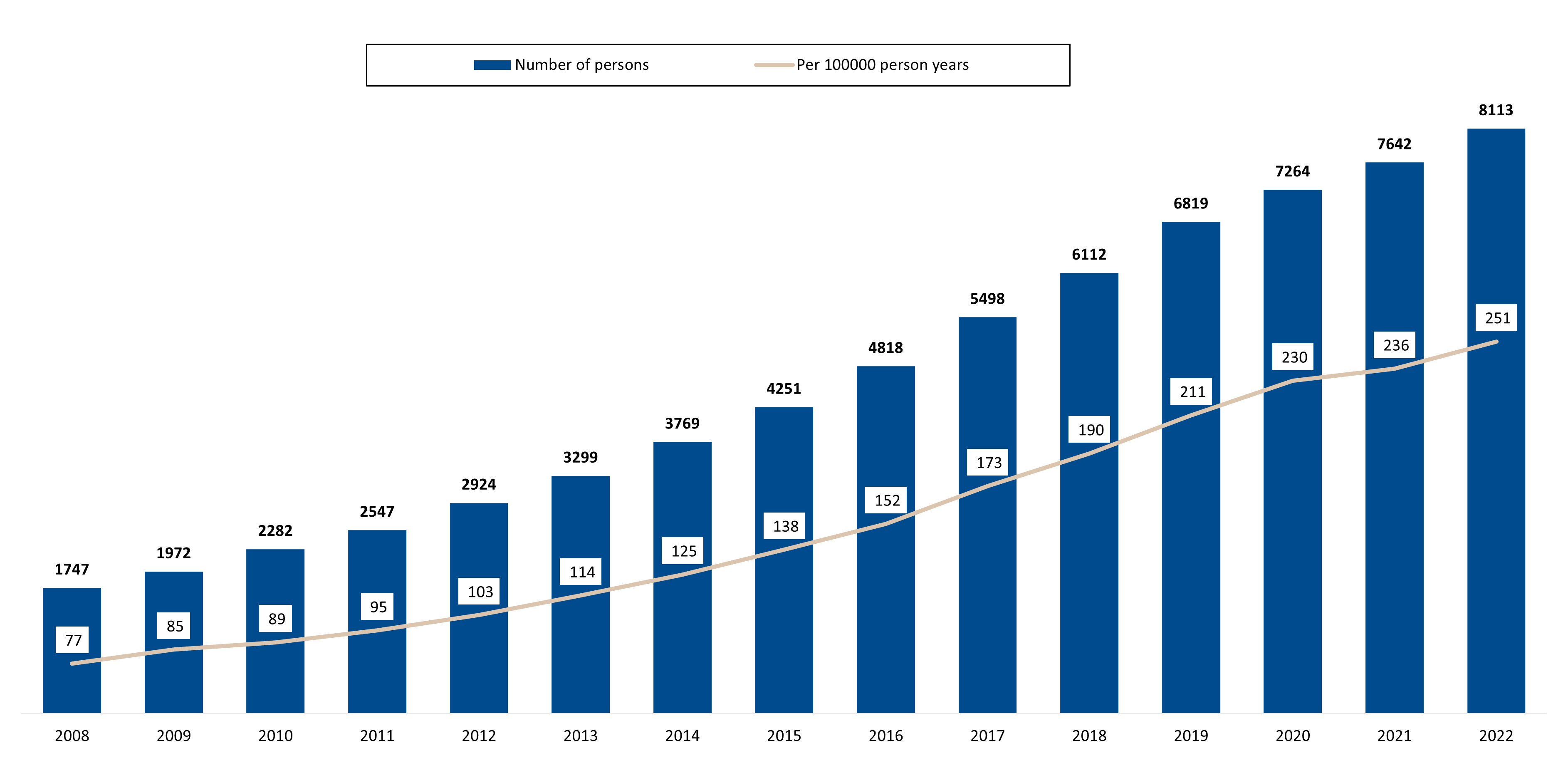
Figure 1: Number of DHMS members registered for CKD, and prevalence of this condition per 100,000 person years, from 2008 to 2022.
7.6-fold increase in pre-dialysis and 4-fold increase in chronic dialysis populations over time
By 2022, DHMS members registered for CKD were split as follows:
- 3,881 (48%) were in the pre-dialysis population
- 3,270 (40%) were in the chronic dialysis population
- 962 (12%) were in the transplant population.
In line with the increase in incidence of all members over time, the number of members in each of our three population groupings has also increased (Figure 2).
From 2008 to 2022 (Figure 2)
- The pre-dialysis population has increased 7.67-fold (a compound annual growth rate - or CAGR - of 15.66%)
- The chronic dialysis population has increased 4.08-fold (10.57% CAGR).
- We note only a 5.75% CAGR increase in the transplant population.
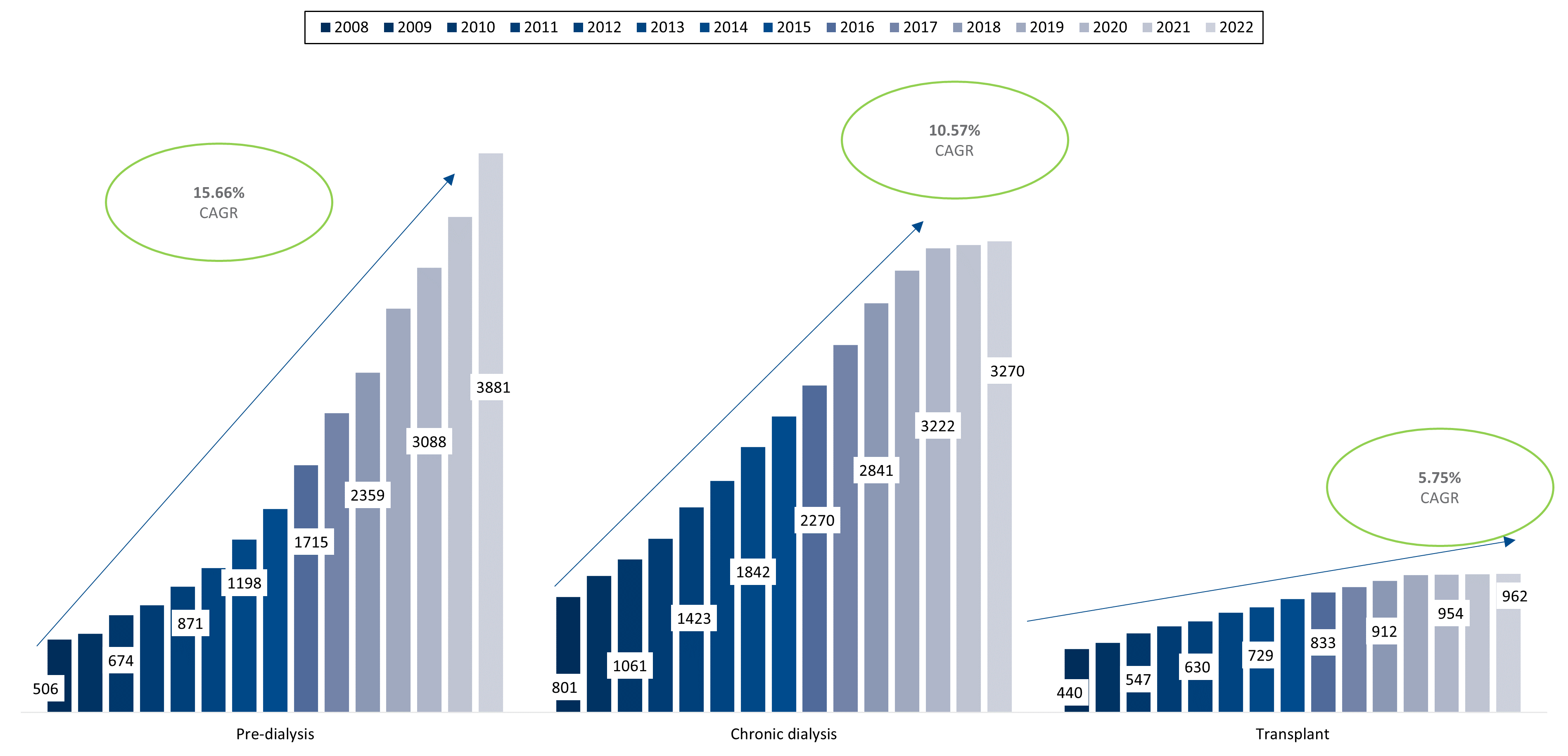
Figure 2: Growth rates of DHMS members in pre-dialysis, chronic dialysis, and transplant populations
- A note on organ transplantation (including kidney transplantation):
Only 0.2% of South Africans are registered as organ donors1
According to the Organ Donor Foundation11, at any given time, up to 5,000 South African adults and children are waiting for a lifesaving solid organ (including heart, lung, liver, pancreas, kidney) or corneal transplant. A study published in 2022 in the SA journal of Surgery12 looking at organ transplantation rates in the Western Cape, shows that the COVID-19 pandemic had a further negative impact on the strained organ supply landscape, with a significant decrease in the number of potential donors referred. In general, the transplant waiting list is growing at a rate faster than the number of transplants being performed annually. Only 6% of transplants needed are being performed annually. The average waiting time for transplant, in private and public sectors of South Africa, is around 5 years 11,13.
CKD disease stage among Scheme members in the pre-dialysis population
CKD is divided into five stages14 based on estimated glomerular filtration rate (eGFR) test results - a measure of how well one's kidneys work through estimating how much blood passes through the glomeruli (tiny blood vessels that filter waste and remove extra fluid from the blood) each minute.
As CKD advances, kidney function decreases. We have used the following classification of eGFR ranges (measured in millilitres of cleansed blood per minute per body surface or mL/min/m2):
- Stage 1: 90 or higher - kidneys working normally / eGFR in normal range yet with early signs of kidney damage.
- Stage 2: 60-89 - mild kidney damage but kidneys still work well.
- Stage 3: 30-59 - Moderate to severe kidney damage and kidneys work sub optimally.
- Stage 4: 15-29 - severe kidney damage and kidneys close to not working at all.
- Stage 5: less than 15 - in end stage failure and requiring renal replacement therapy (chronic dialysis or kidney transplant).
eGFR results in the Scheme's 3,881 pre-dialysis members in 2022 showed the following CKD stage split (Figure 3).:
- 140 (4%) at Stage 1
- 481 (12%) at Stage 2.
- (Majority of members) 2,758 (71%) at Stages 3 and 4
- 303 (8%) at stage 5.
- eGFR results were not available for 199 (5%) members in the pre-dialysis population in 2022 - referred to as "Unstratified" in Figure 3.
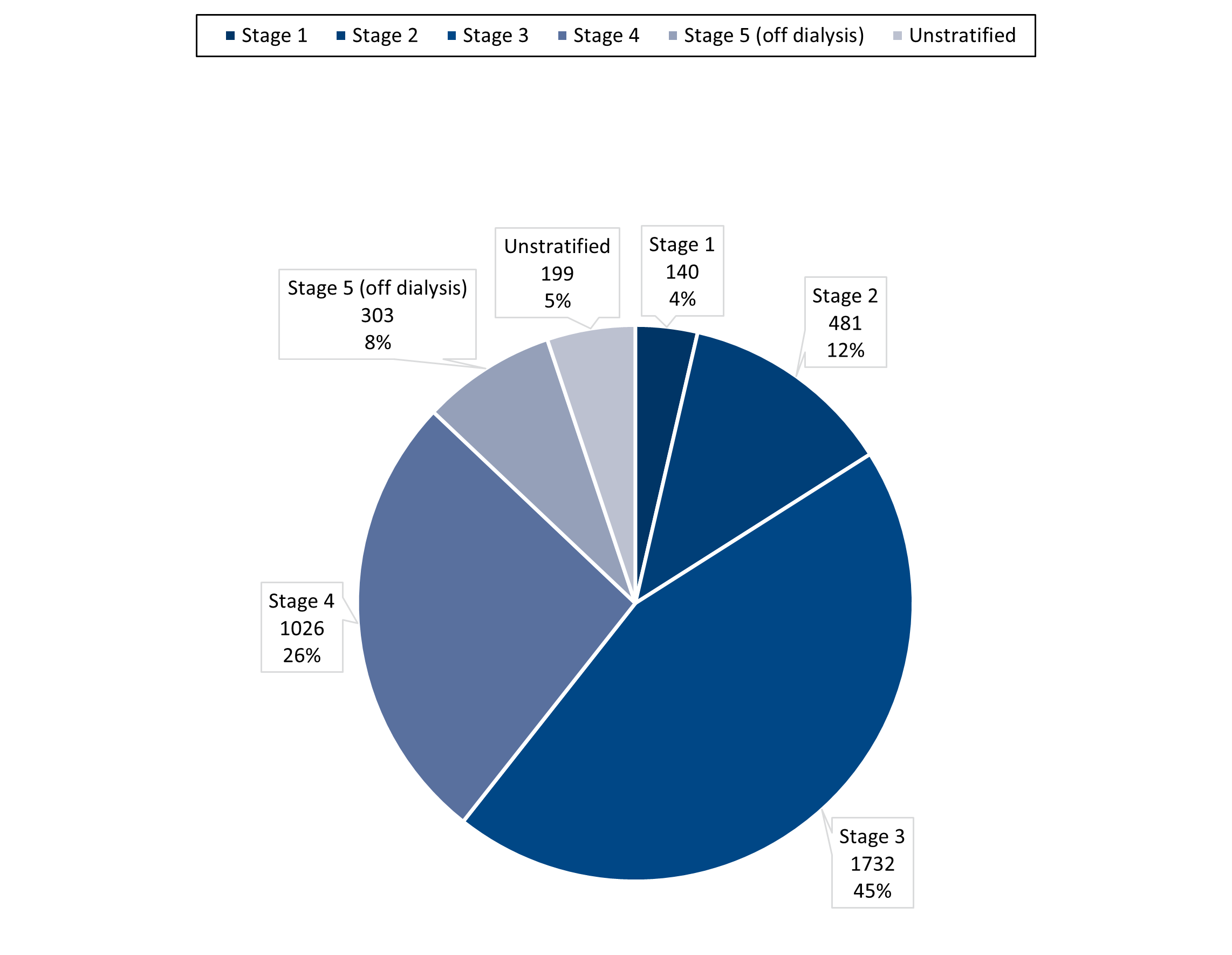
Figure 3: Distribution of Scheme members in the pre-dialysis cohort by renal stage based on 2022 eGFR results (where unstratified refers to members without an available eGFR test result)
Investigating the demographic profile of Scheme members living with CKD across a range of metrics
(a) Age distribution in Scheme members with CKD
Scheme members with CKD are significantly older than the average DHMS member. In 2022:
- The average DHMS member age was 36 years old.
- The majority of members (77%) were between the ages of 5 and 59.
- The average age of members with CKD was 59 years old, with most (78%) between the ages of 45 and 84 (Figure 4).
- The average age of the pre-dialysis population was 64 years
- The average ages of the chronic dialysis and transplant population were younger, at 57 and 47 years respectively.
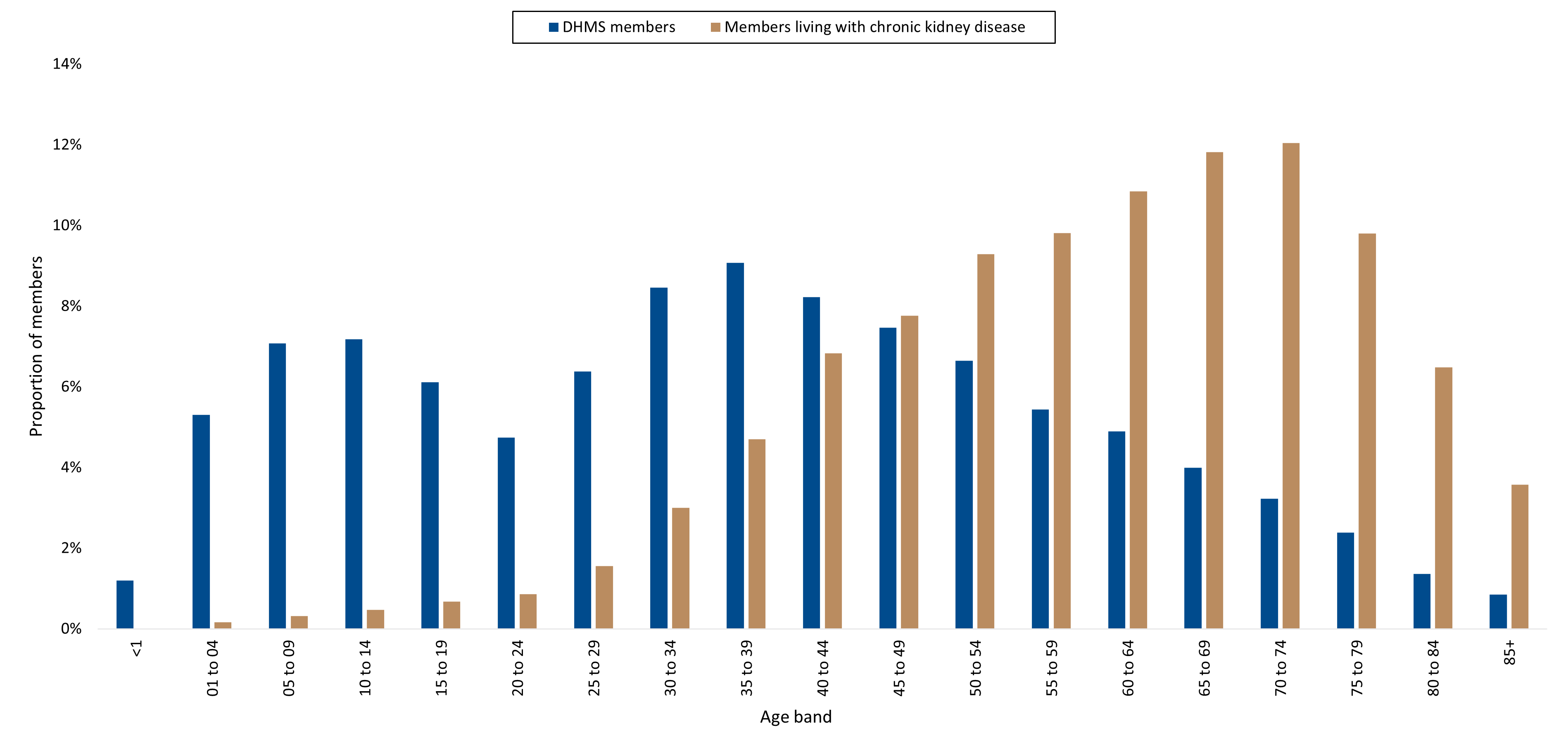
Figure 4: The age distribution of members living with CKD compared to all DHMS members, in 2022.
We also note a shift towards older ages amongst members living with CKD, from 2008 to 2022. This distribution change over the years is consistent across all three segments of the CKD population (pre-dialysis, chronic dialysis, and the transplant population). This suggests that these members' life expectancy has increased since 2008 (Figures 5a, 5b, 5c, 5d).
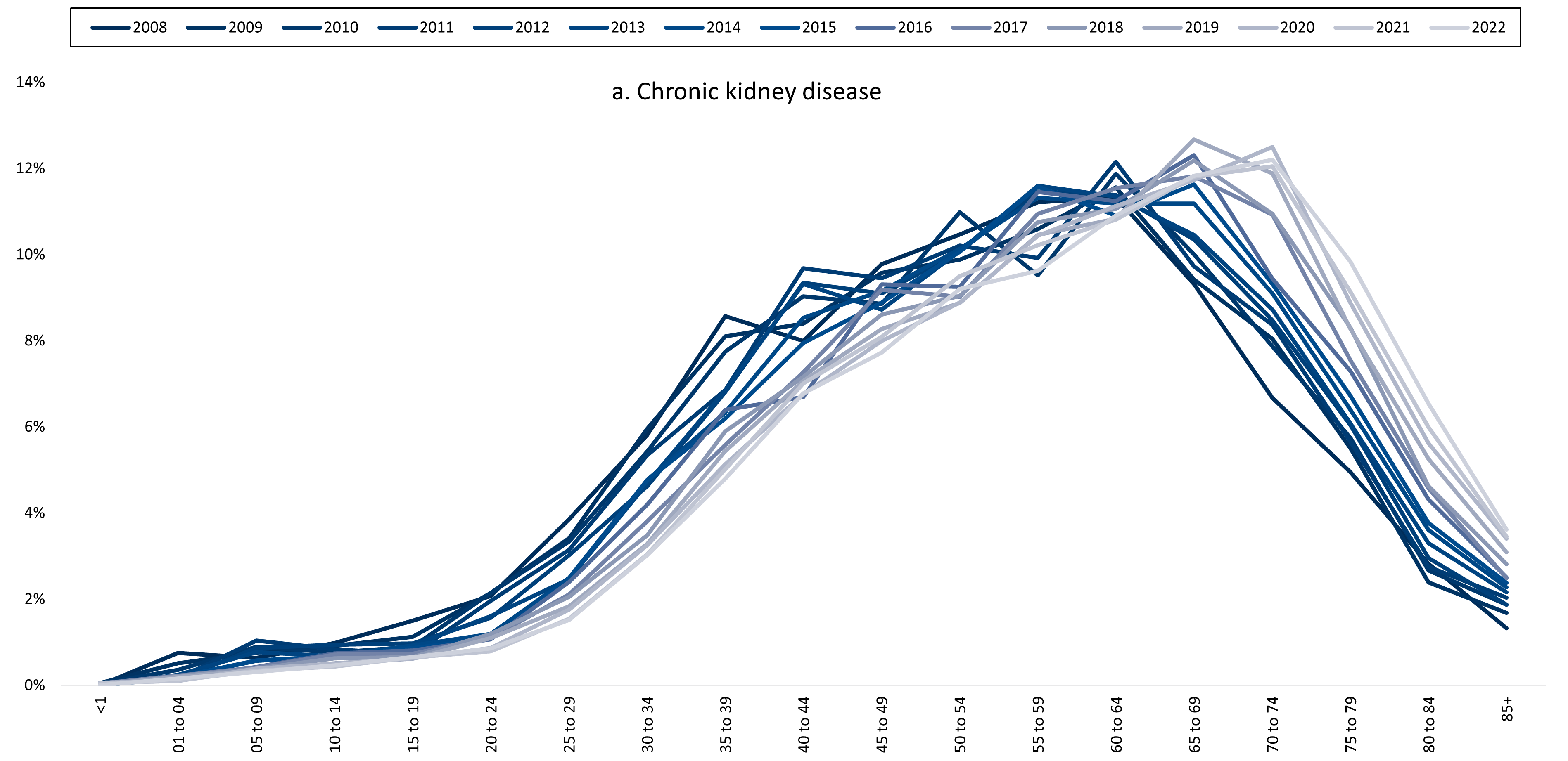
Figure 5a: Shift towards higher age bands evident from 2008 to 2022, among all DHMS members living with CKD.
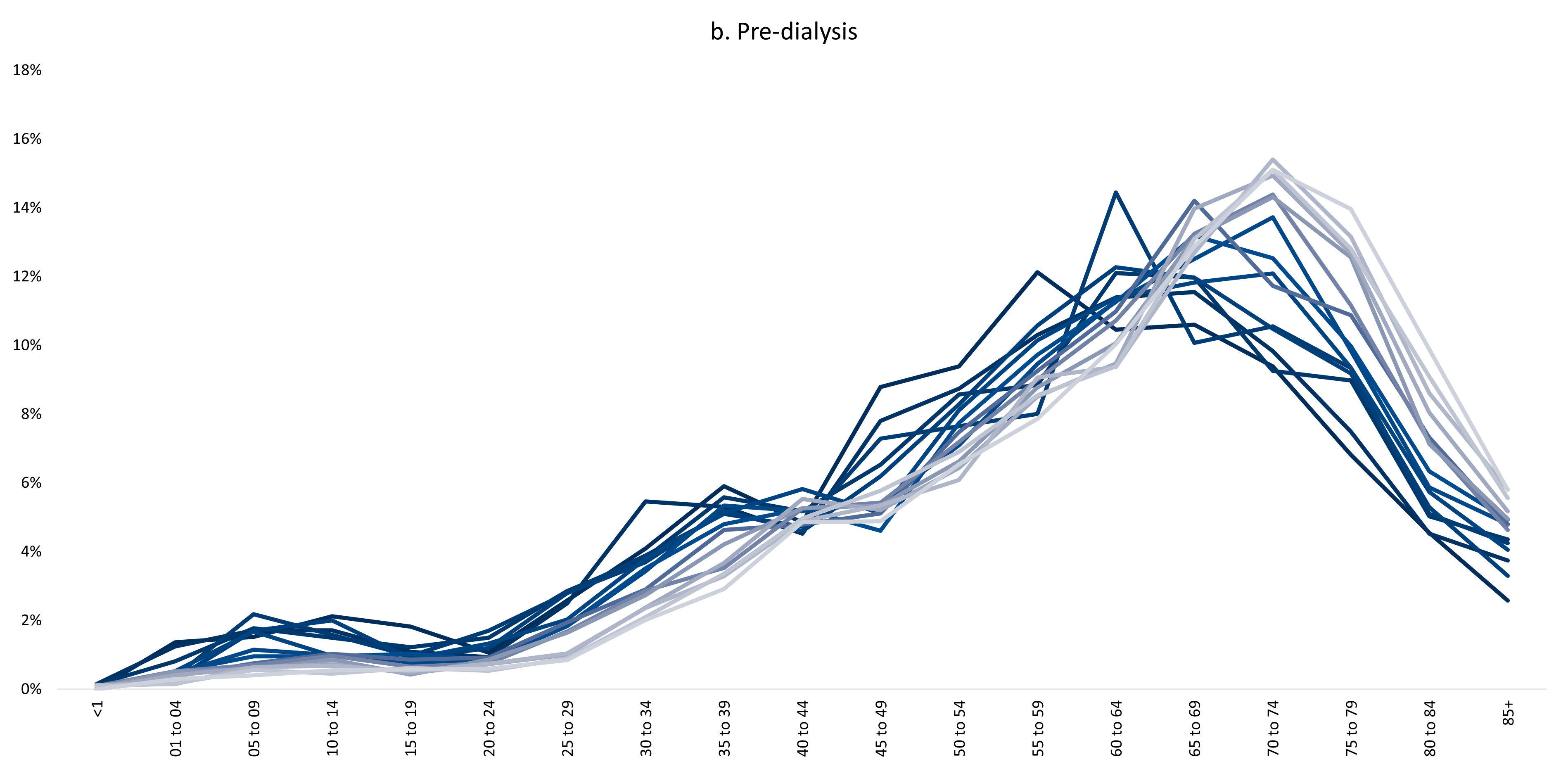
Figure 5b: Shift towards higher age bands evident from 2008 to 2022, among DHMS members living with CKD and who are in the pre-dialysis population.
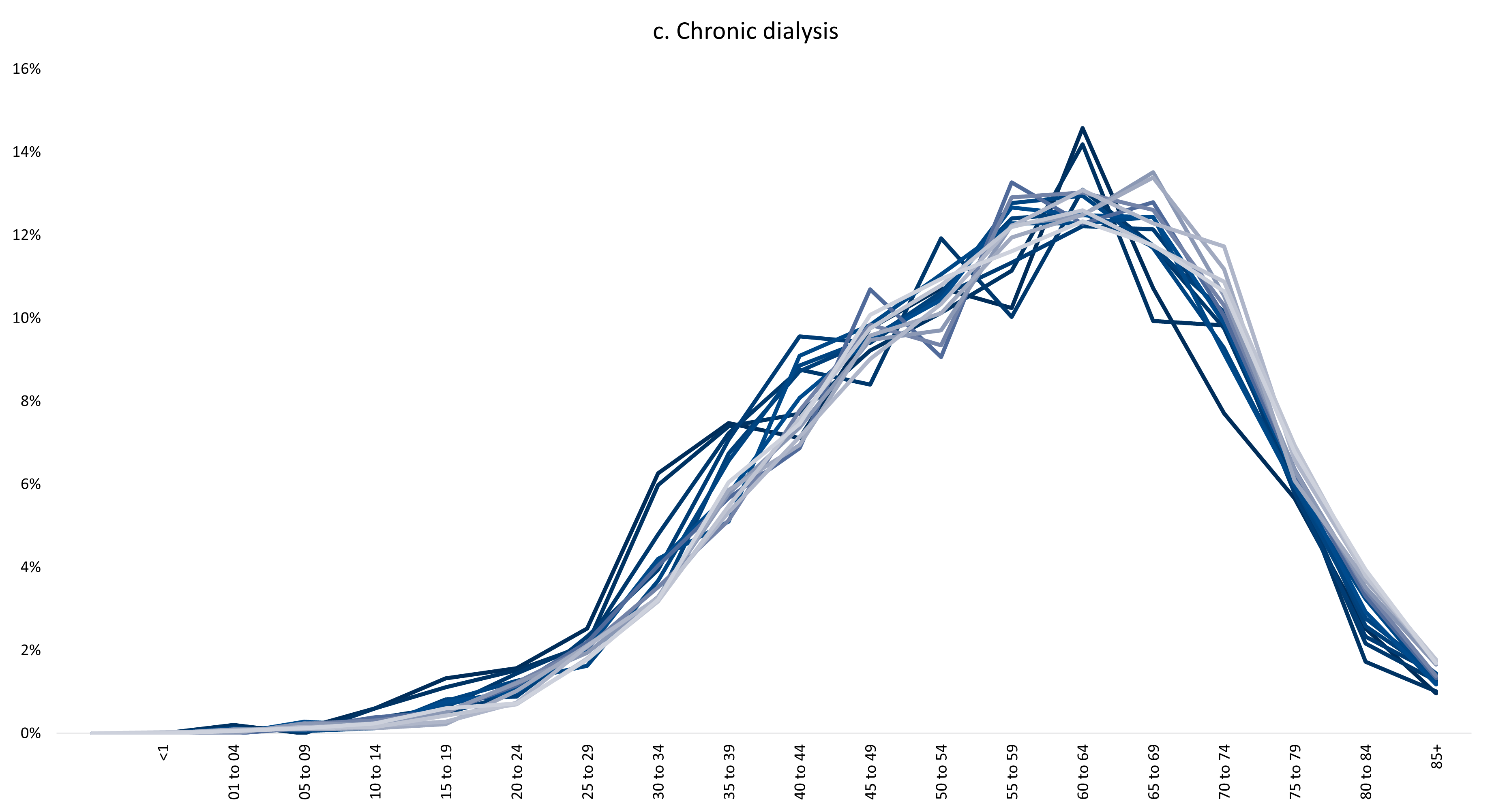
Figure 5c: Shift towards higher age bands evident from 2008 to 2022, among DHMS members living with CKD and who are in the chronic dialysis population.
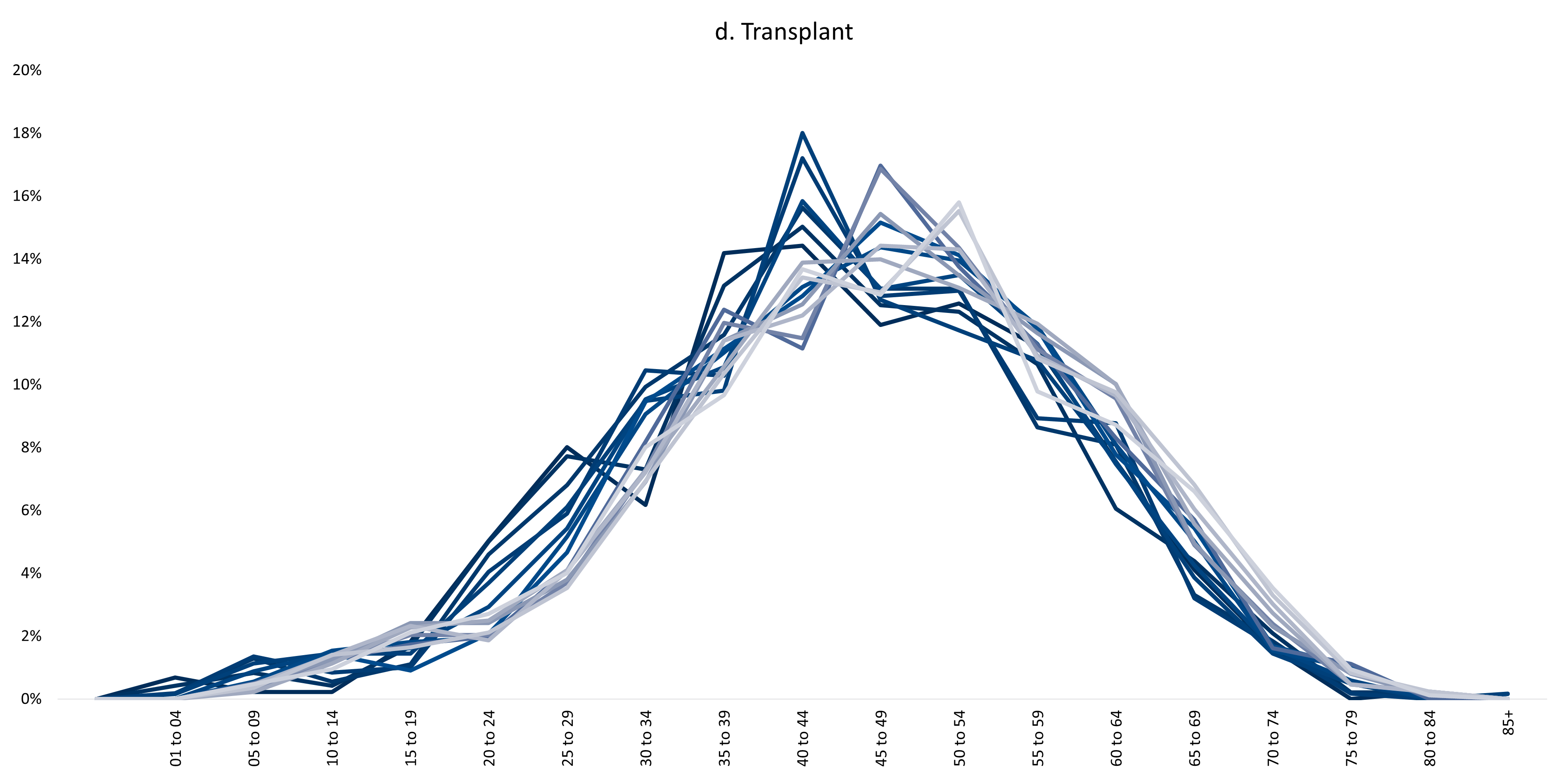
Figure 5d: Shift towards higher age bands evident from 2008 to 2022, among DHMS members living with CKD and who are in the kidney transplant population.
(b) Distribution of males and females living with CKD
The distribution of males and females living with CKD has remained steady over time (Figure 6).
- Females make up 40 to 42% of the population.
- Males make up 58 to 60% of the population.
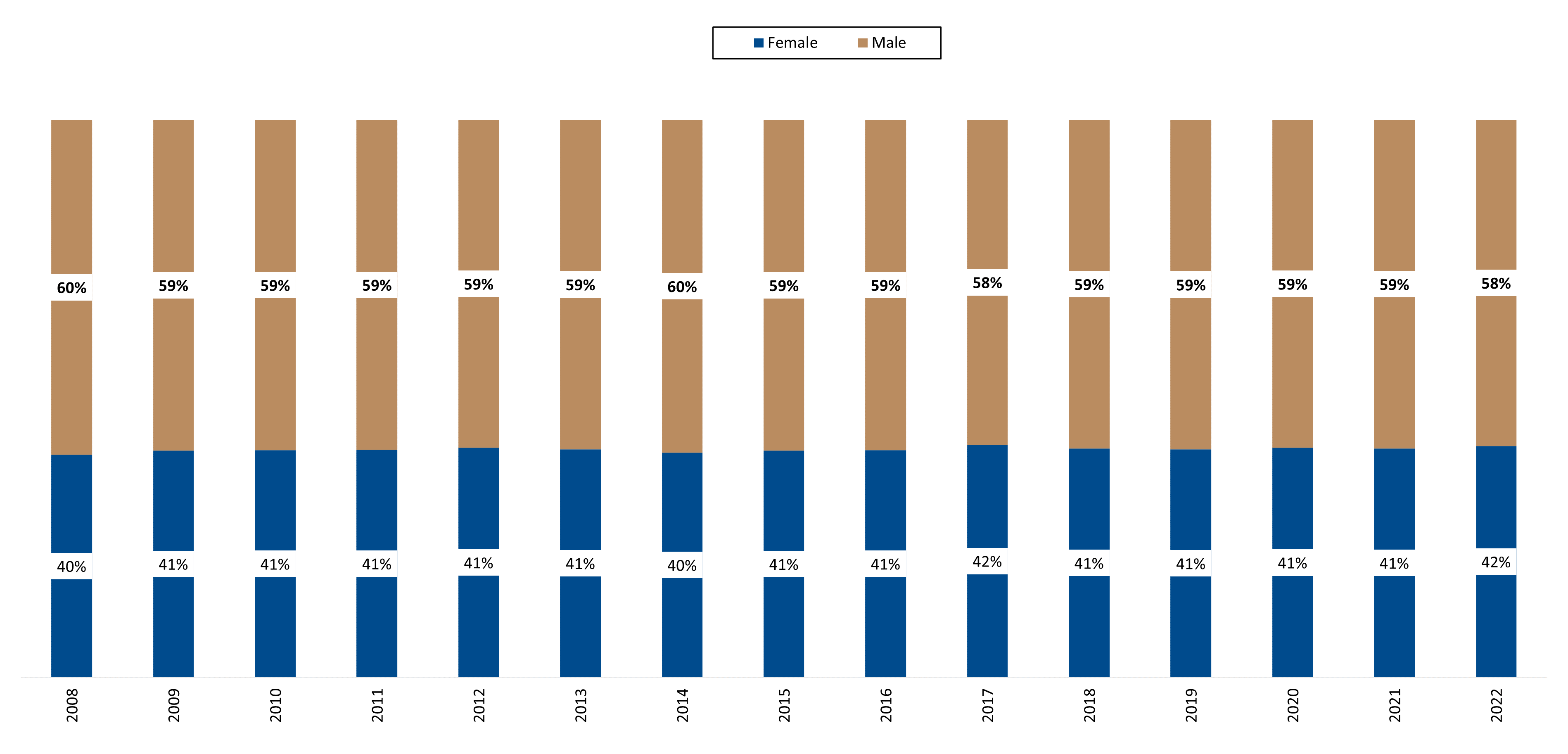
Figure 6: Distribution of male and female Scheme members living with CKD, over time
(c) Distribution of Scheme members living with CKD by province in South Africa
In 2022, most members (48%) received treatment in Gauteng followed by KwaZulu-Natal (20.2%). The smallest population of Scheme members treated for CKD was in the Northern Cape (0.6%).
Despite KwaZulu-Natal being the province where the second highest concentration of Scheme members underwent treatment, this province's transplant population (11.1%) was far lower than that of the Western Cape (25.4% transplant population) which had the third highest member treatment population. Overall, in 2022, 495 members in the transplant population were treated in Gauteng, 244 in the Western Cape, 107 in KwaZulu-Natal, 43 in the Eastern Cape, and the remainder in other provinces.
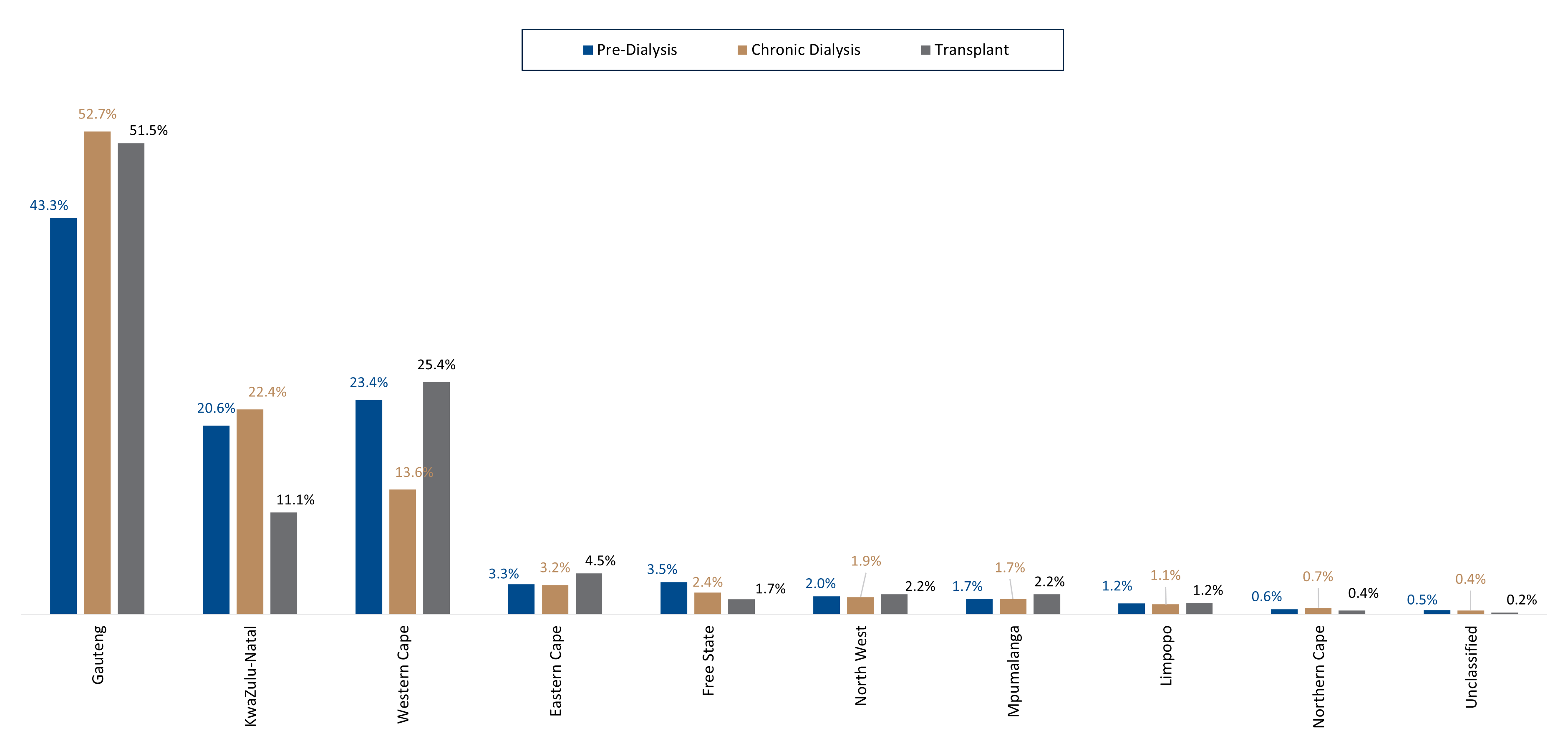
Figure 7: Province in which CKD members received treatment in 2022
(d) Other chronic conditions affecting Scheme members living with CKD
Although kidney disease occurs for many reasons, people most often develop this condition as a result of having diabetes, high blood pressure or heart disease15.
In 2022:
- 23% of DHMS members who were registered for CKD (1,832 people) were also registered for more than five additional chronic conditions.
- 15% were registered for CKD (1,185 people) and five other chronic conditions.
- 19% were registered for CKD (1,528 people) and four other chronic conditions.
- 20% were registered for CKD (1,661 people) and three other chronic conditions.
- Only 205 members (3% of our study population) were registered for kidney disease alone (Figure 8).
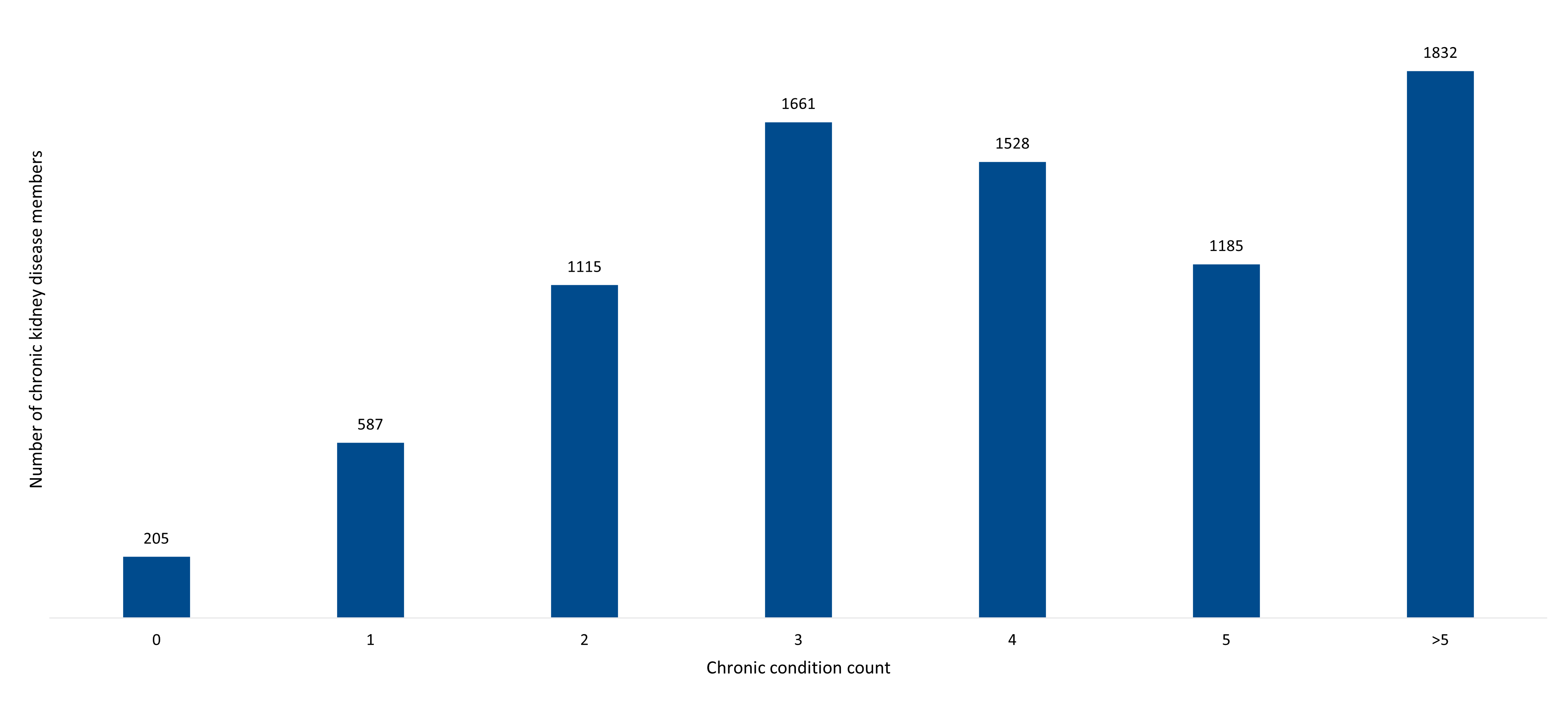
Figure 8: Number of additional chronic conditions that members with CKD were registered for in 2022
In 2022, the most common co-morbidities among members living with CKD were essential hypertension with hypercholesterolaemia (977 or 12%) followed by hypertension alone (896 or 11%) (Figure 9) and then a combination of essential hypertension with hypercholesterolaemia and type 2 diabetes (761 or 9%).
Other co-morbidities featuring in this population included:
- Type 2 diabetes
- Ischaemic heart disease
- Congestive heart failure
- HIV
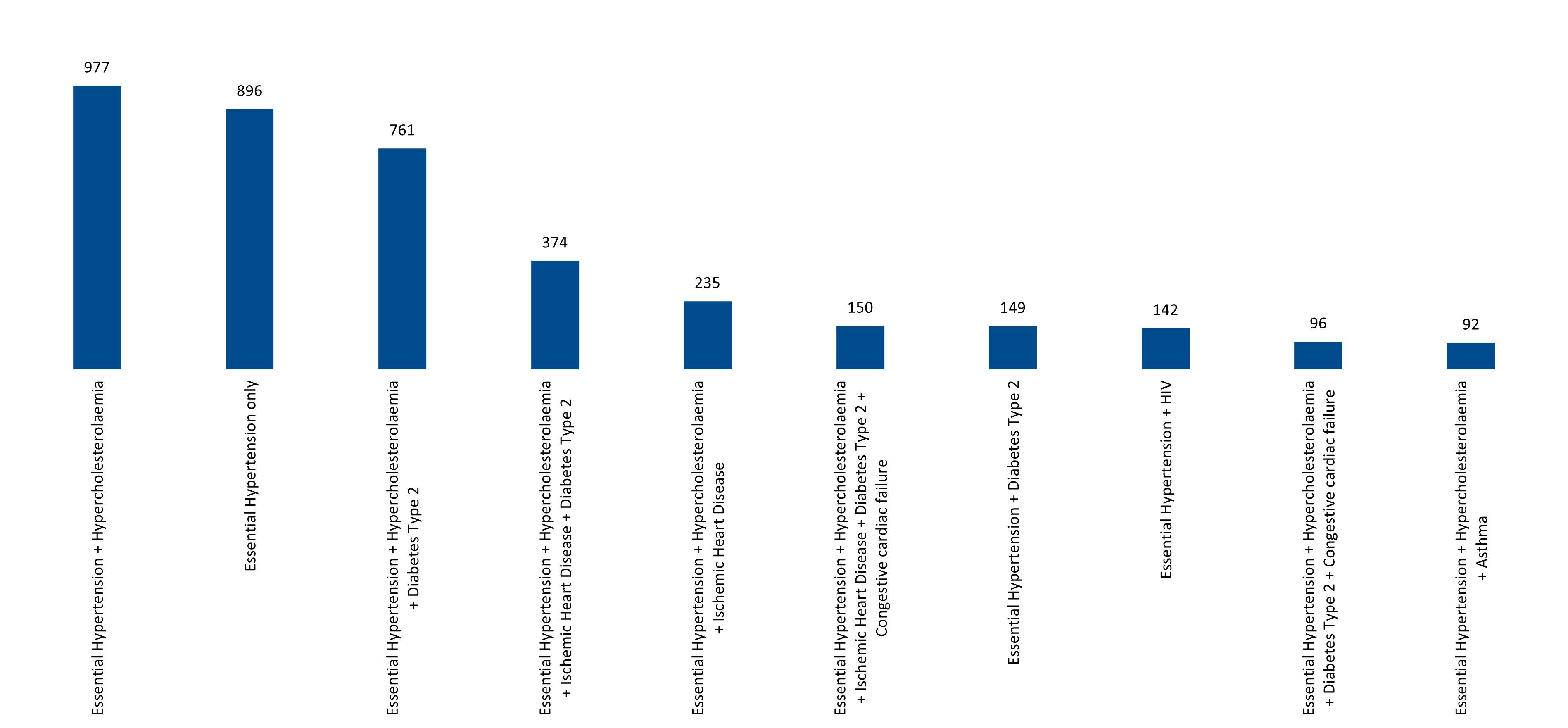
Figure 9: Top 10 comorbid combinations amongst members who also have CKD in 2022
What does Vitality data tell us about Scheme members living with CKD?
Discovery has adopted a shared-value health and life insurance model through its science-based Vitality programme16, which provides members with comprehensive health promotion and disease prevention services. Vitality members who engage in health-promoting activities (such as exercising) or preventive activities (recommended preventive screenings) are awarded points that move them up through a tiered status system from Blue Vitality status up to Bronze, Silver, Gold and the highest status, Diamond.
The absolute number of DHMS members living with CKD and who were also Vitality members increased from 919 to 2,558 between 2008 and 2022. However, the percentage of such members dropped from 53% to just under a third (32%) of members. Among Vitality members (Figure 10), those on Blue status decreased from 87% in 2008 to 54% in 2022. Those on Bronze or Silver Vitality status increased respectively from 11% and 1% in 2008, to 33% and 7% in 2022.
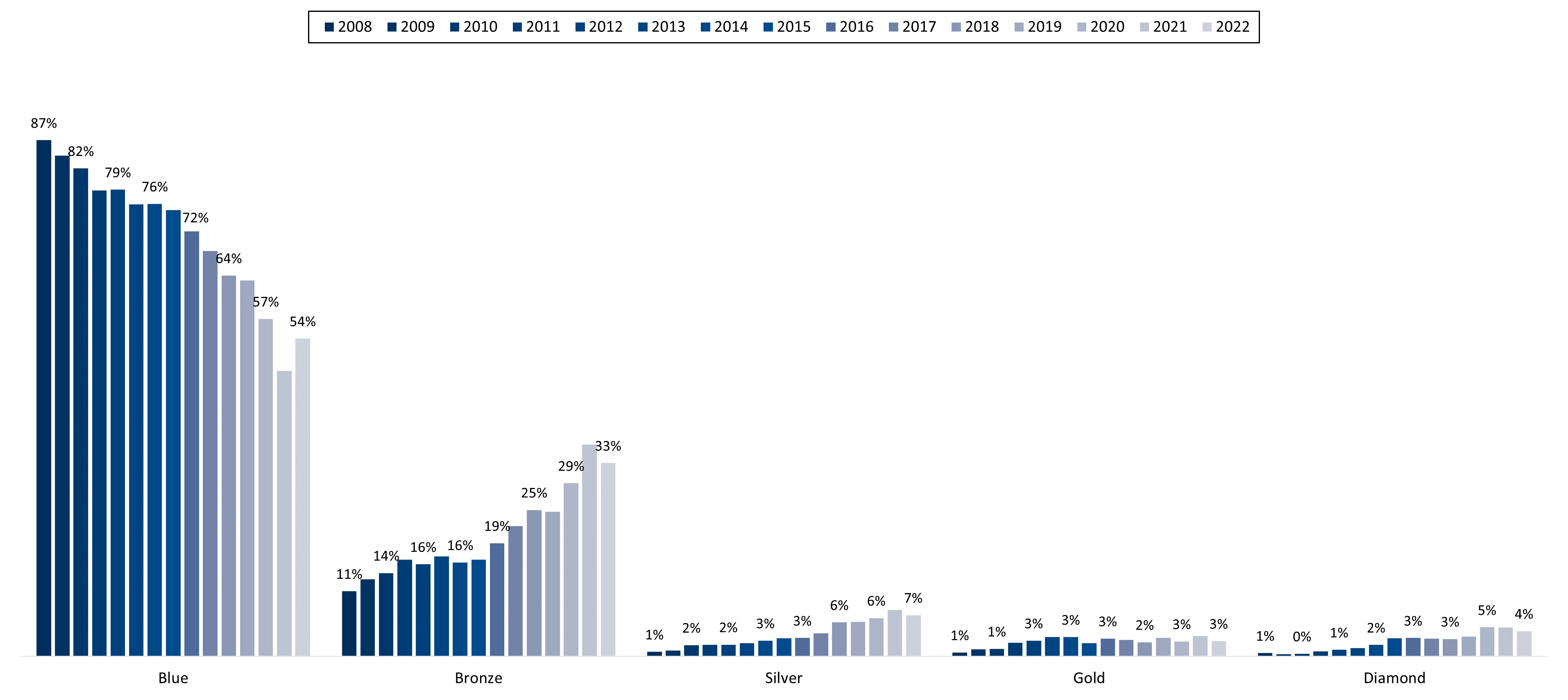
Figure 10:Distribution of members living with CKD by Vitality status, 2008-2022
Members of the CKD population who were also Vitality members in 2022:
- 32% of the pre-dialysis cohort
- 27% of the chronic dialysis cohort
- 47% of the transplant cohort.
Most of the above-mentioned members were on Blue or Bronze Vitality status. More people from the pre-dialysis and transplant groups (18% and 17% respectively) were on Silver, Gold or Diamond status, than were people from the chronic dialysis group (6%) (Figure 11). This suggests that members in pre-dialysis and transplant populations are able to live healthier lifestyles, and likely be more active too (as physical activity, among other metrics, boosts Vitality status, as mentioned above).
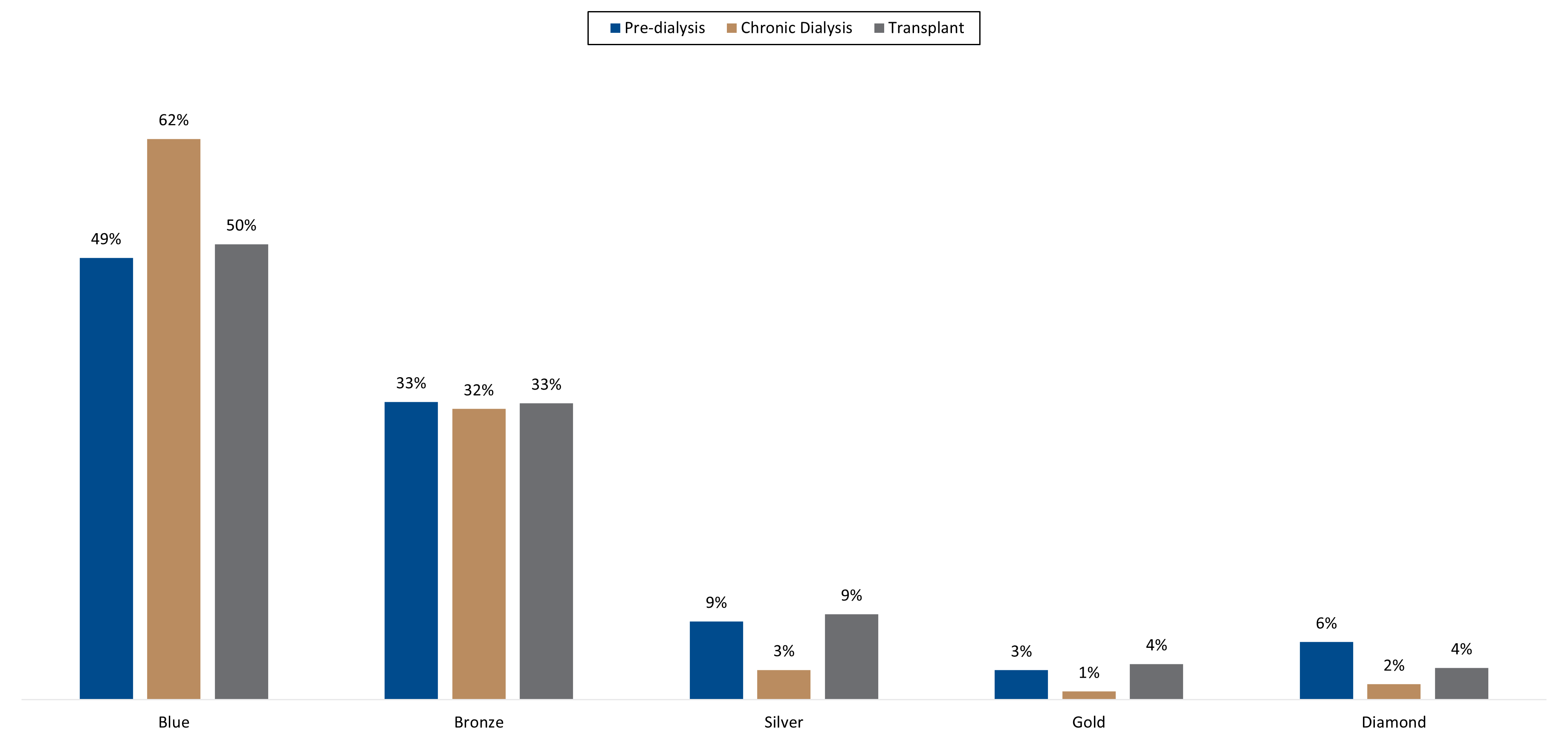
Figure 11: DHMS population living with CKD - segmented by Vitality status in 2022
Cost impact and admission experience for Scheme members living with CKD
(a) Cost impact
In 2008, a medical scheme member living with CKD cost the Scheme (on average, per month) 31.5 times more than the average DHMS member. This relative cost has come down to 17-fold more than the average DHMS member in 2022 (a reduction of 4.3% per annum). A contributing factor to this decline in relative cost is the higher proportion of members in the pre-dialysis member group in 2022 relative to 2008 (Figure 2).
In 2022, members in the pre-dialysis, chronic dialysis and transplant groups cost the Scheme 7.2-, 29- and 15.7-fold more, per month, than the average DHMS member (Figure 12).
These costs have also come down over time as, in 2008, members in the pre-dialysis, chronic dialysis and transplant groups cost the Scheme 10.7-, 49.8- and 24.5-fold more than the average DHMS member.
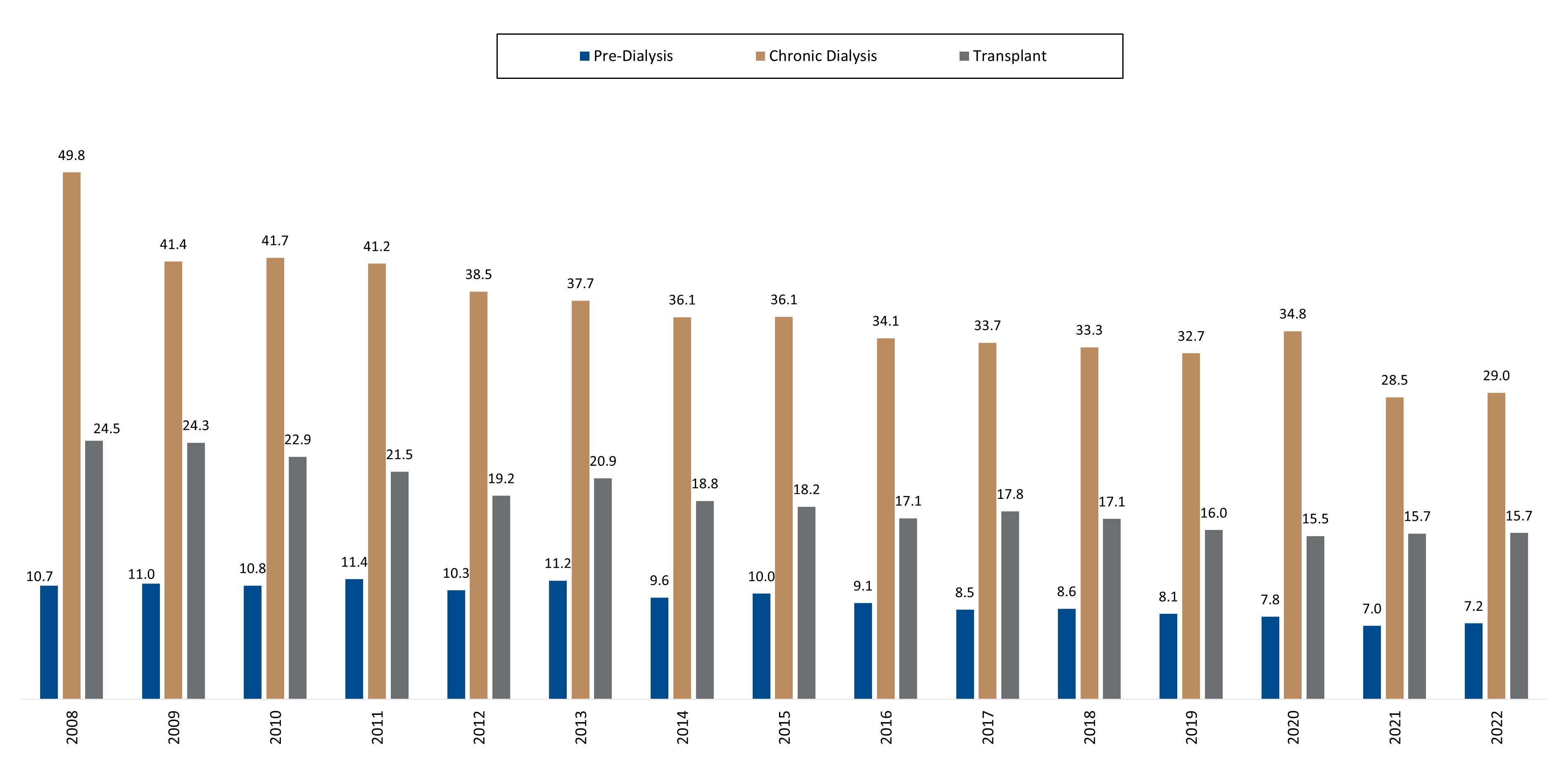
Figure 12: Indication of the magnitude of cost to the Scheme for members living with CKD relative to an average DHMS member, each month.
The total cost of treating Scheme members living with CKD has increased steadily year-on-year, from about R316 million in 2008 to R2.4 billion in 2022. These figures accounted for 2.5% of DHMS total expenditure in 2008 and 4.1% of total expenditure in 2022 (Figure 13). One of the reasons for this increase in spend is the increase in members living with CKD, and proportion of members living with CKD over time (Figure 1).
- The COVID-19 period: The significant disruption to healthcare utilisation patterns during the COVID-19 pandemic resulted in costs related to members living with CKD declining from 4.7% of total DHMS spend in 2020, to 4% in 2021 and slightly up to 4.1% in 2022.
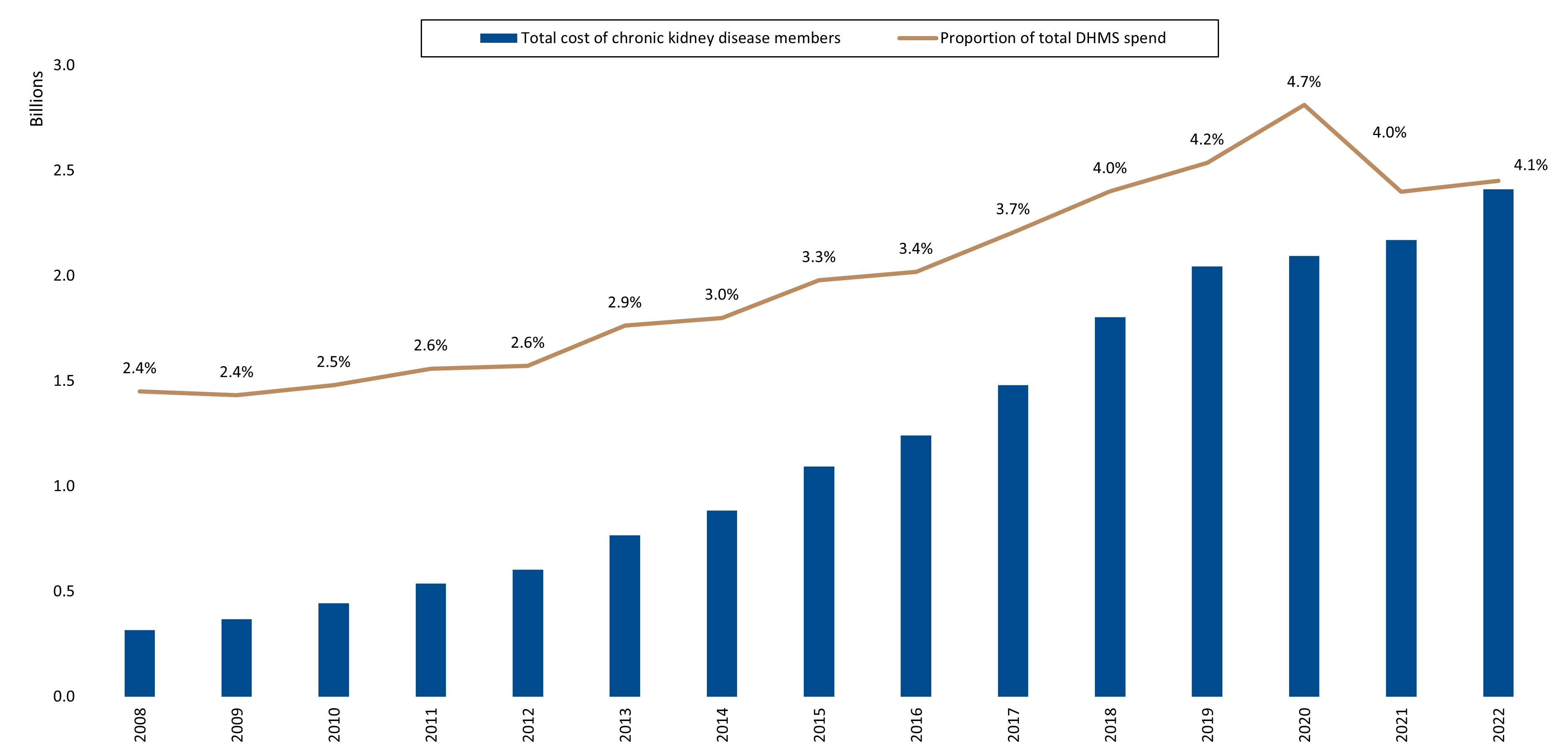
Figure 13: Total costs generated by members who have CKD; and proportion of total DHMS spend allocated to these members, from 2008 to 2022
(b) Admission experience over time
In our prior studies, we observed a significant drop in admission rates across the DHMS member base during the COVID-19 pandemic period (which we take as 2020 to 2022 for the purposes of our analyses). This decline in admission rates was evident among members living with CKD too. And, by 2022, utilisation levels had not yet gone back to pre-pandemic levels.
How often are members living with CKD admitted to hospital?
In 2022, 4,949 (61%) members living with CKD were admitted to hospital at least once (so once or more). And 3,147 (39%) of members living with CKD were admitted multiple times (average number of admissions at 3.67 admissions per person).
That said, admission rates have dropped over time, from 66% admitted at least once and 48% admitted multiple times in 2008, to 65% admitted at least once and 44% admitted multiple times in 2019 (pre-pandemic) (Figure 14)
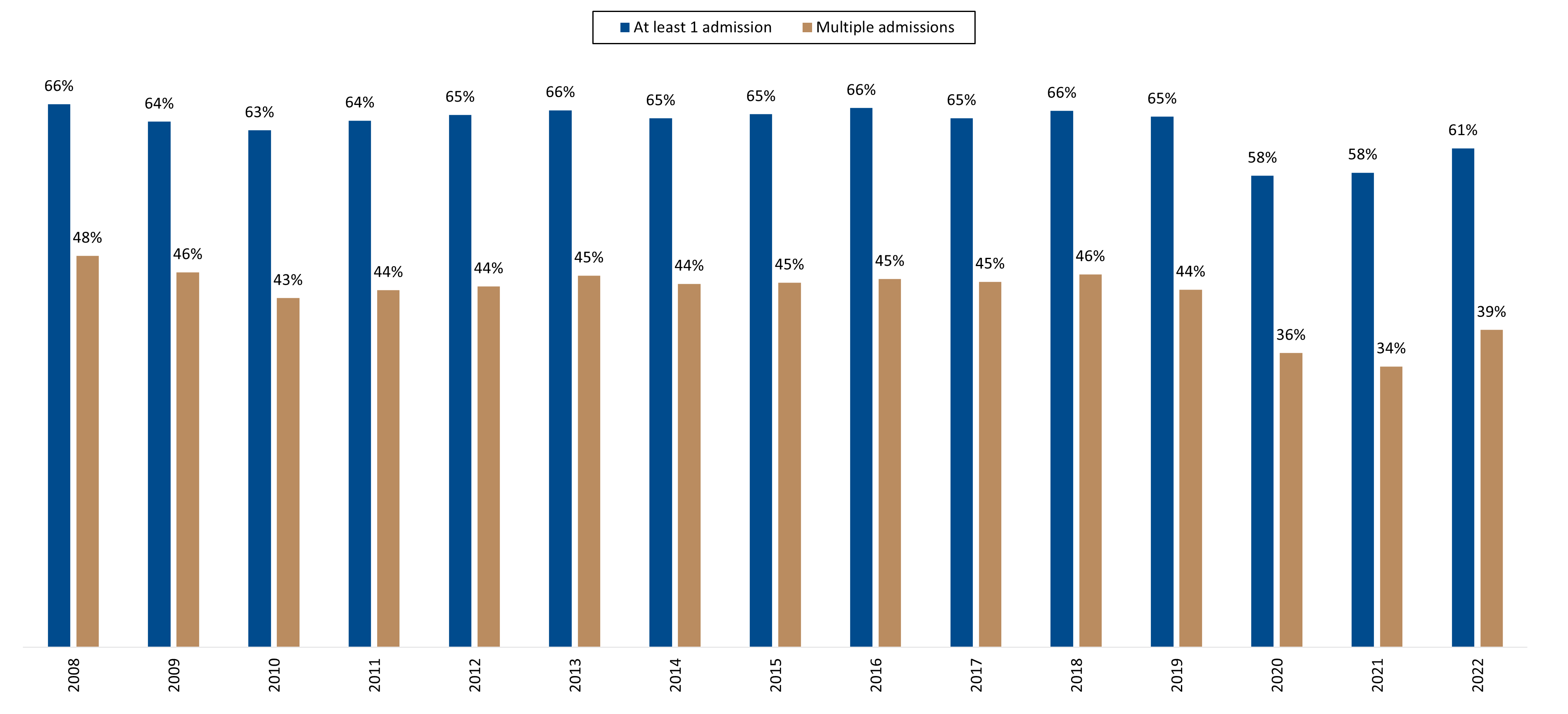
Figure 14: Proportion of Scheme members who have CKD who have had at least one admission or multiple admissions, from 2008 to 2022
Looking at our three cohorts (Figures 15 and 16) the most admissions were in the chronic dialysis population where, in 2022, 2,444 members (75%) were admitted at least once, and 1,732 members (53%) multiple times.
In the pre-dialysis population 1,972 (51%) members were admitted at least once and 1,073 (28%) multiple times. In the transplant population 533 (55%) members had at least one admission and 342 (36%) had multiple admissions.
In 2022, where members were admitted multiple times, the average number of admissions across our three populations was similar:
- 3.9 in the chronic dialysis population
- 3.2 and 3.6 in the pre-dialysis and transplant populations
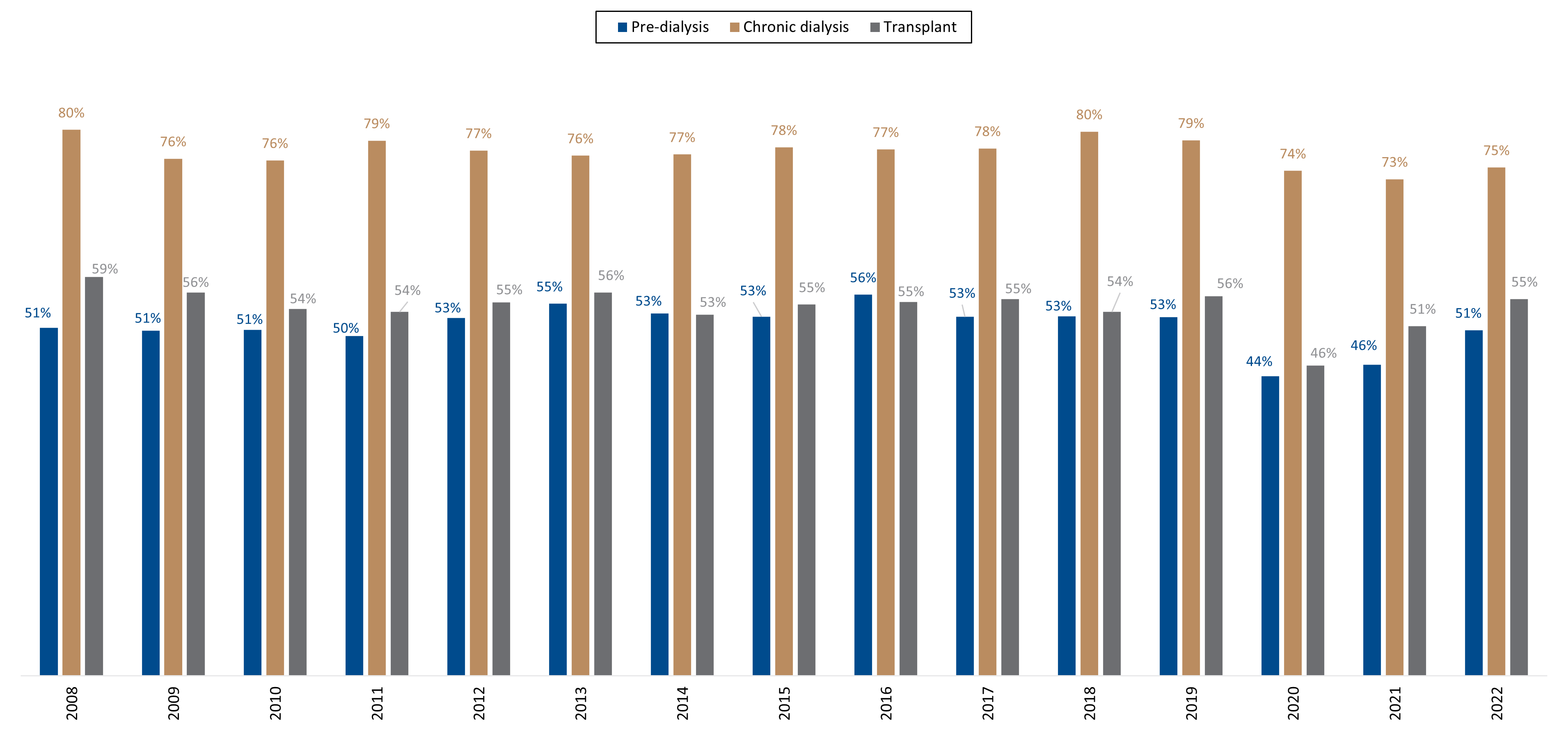
Figure 15: Proportion of members living with CKD with at least one admission
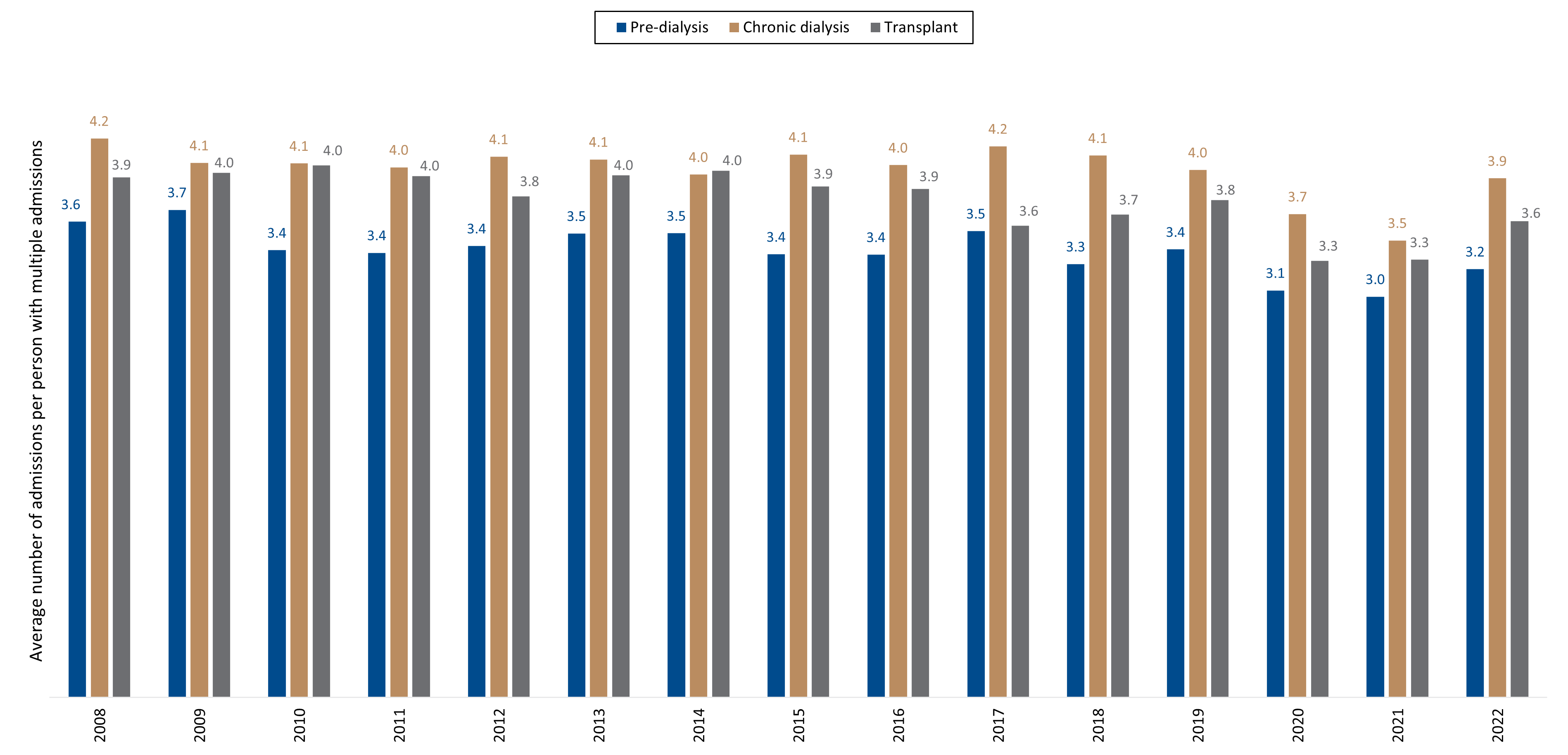
Figure 16: Average number of admissions per person, where Scheme members have had multiple admissions per year
Mortality rates among Scheme members who live with CKD
In 2022, 625 Scheme members living with CKD, died. In this group 535 (85.6%) members died at an age younger than that earmarked as the average life expectancy for the general DHMS population, which is 85.2 years for females and 80.88 years for males. The youngest DHMS member with CKD to die in 2022 was 10 years old.
Data show that 18.4% of DHMS members living without CKD live past 85, but only 6.2% of those living with CKD live that long (Figure 17). Where Scheme members who had CKD died between 2010 and 2022, 73.9% of members were under 75 years old (versus 58.9% of average DHMS members who died before the age of 75).
Deaths among members living with CKD resulted in 9,423 of years of life lost in 2022 alone - 4,148 for females and 5,275 for males. This equates to an average of 15 years of life lost per person.
- 'Years of life lost' is a metric referring to how much younger people with a disease die than an average healthy person. For our analyses we take the average age at death for the total DHMS population and calculate the difference between this average age of death and the actual age at which members with CKD die.
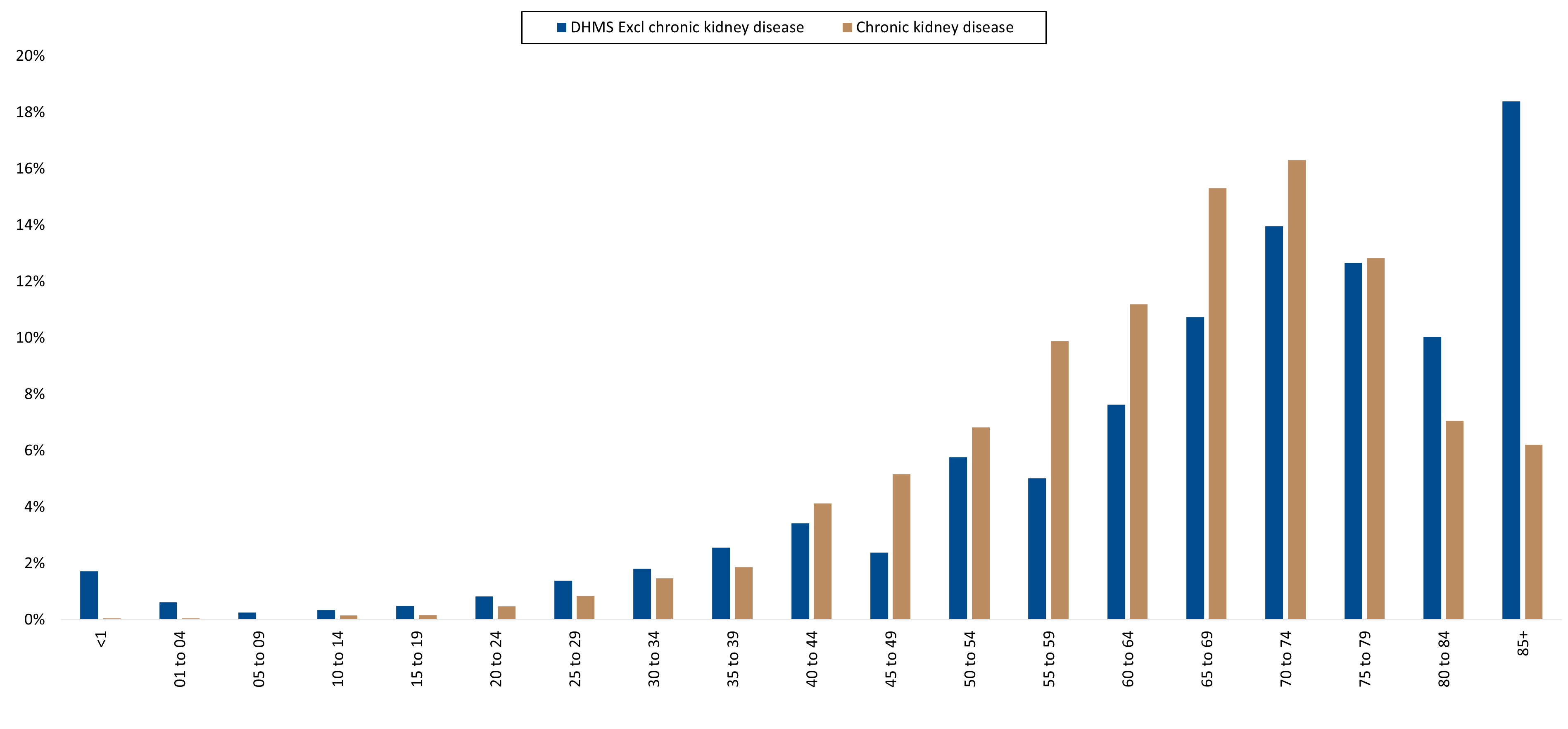
Figure 17: Distribution of deaths among DHMS members living with CKD compared to DHMS members who do not have CKD, by age, between the years 2010 and 2022.
Over time (standardised by age and sex distribution), Scheme members living with CKD have consistently higher mortality rates than average DHMS members (who do not have CKD). The CKD-related mortality rate was 5.3 times higher than the average DHMS mortality rate in 2022.
That said, the age and sex standardised mortality rate in the CKD population has decreased from 12,311 per 100,000 person years in 2010 to 8,922 per 100,000 person years in 2022 (a 28% decrease over 12 years).
Impact of COVID-19 on mortality rates over 2020 and 2021
In 2020 and 2021 mortality rates increased across the DHMS member base (Figure 18). To determine the extent to which this was due to COVID-19 disease, we removed deaths where the underlying cause (determined by healthcare workers and experts, in mortality coding) was related to COVID-19. Doing this showed there was no increase in deaths in either the members living with CKD or the general DHMS population, so the increase in deaths was linked to COVID-19 disease.
Among members who died of COVID-19, those living with CKD experienced a higher mortality rate in the first year of the pandemic (a 29% increase from 2019) than members not living with the disease (16% increase from 2019).
- Compared to 2019, in 2021 mortality rates were 54% higher for members living with CKD and 57% higher for those not living with CKD.
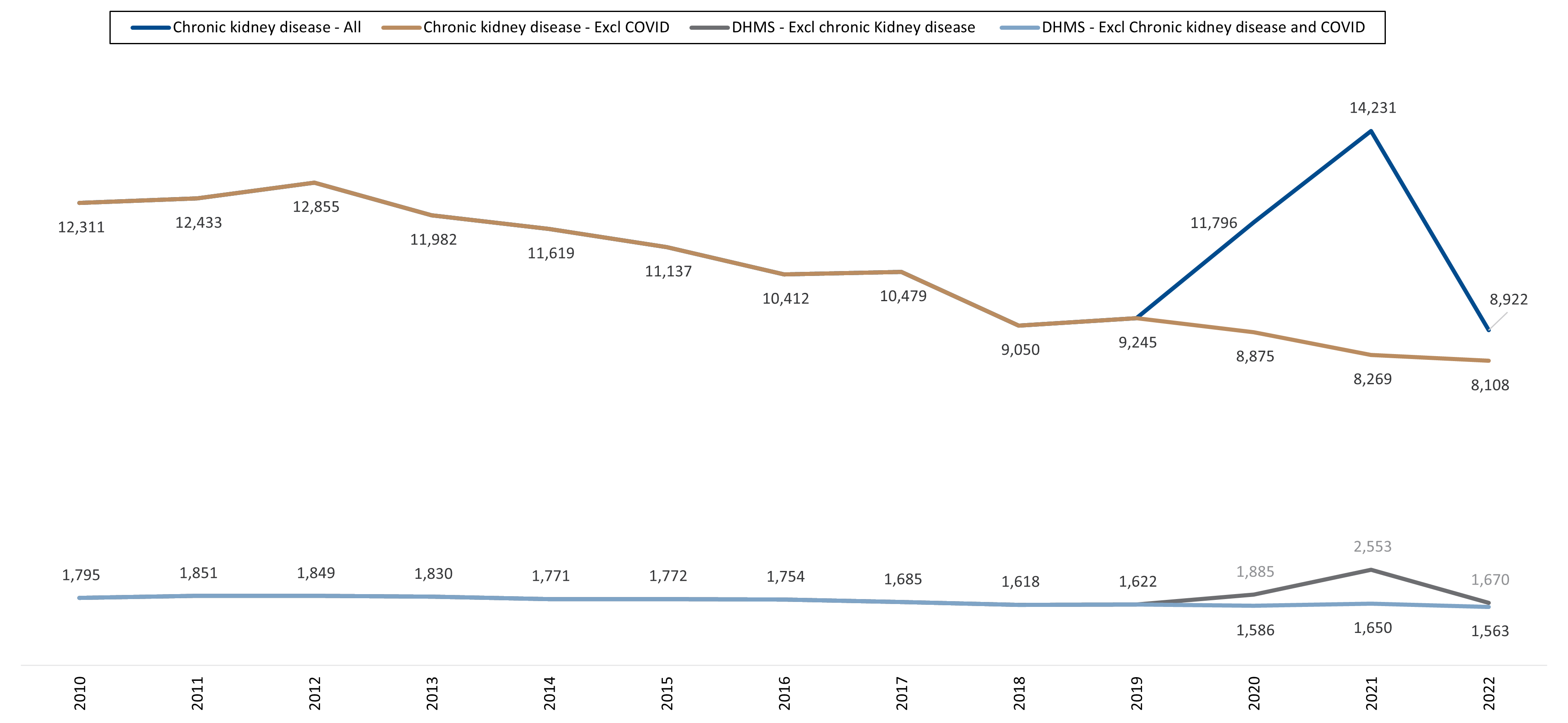
Figure 18: Age and sex standardised mortality rate per 100 000 person years over time, for DHMS members who have CKD compered to average DHMS members (who do not have CKD)
Looking within our cohorts:
In 2022, members of our chronic dialysis cohort experienced a higher mortality rate than the pre-dialysis cohort - 12,989 per 100,000 person years versus 6,537 per 100,000 person years. (Figure 19). So, the mortality rate amongst those on chronic dialysis was 2.0 times higher than those on pre-dialysis in 2022.
That said, these mortality rates were lower in 2022 for both groups than they were in 2010 - 23% lower for the chronic dialysis group, and 32% lower for the pre-dialysis group.
The transplant population was excluded from this part of our analysis due to high volatility in mortality rates in this group each year. (This is a small population, and, for example, there were a low number of deaths (31) deaths in this group in 2022, compared to the other two cohorts).
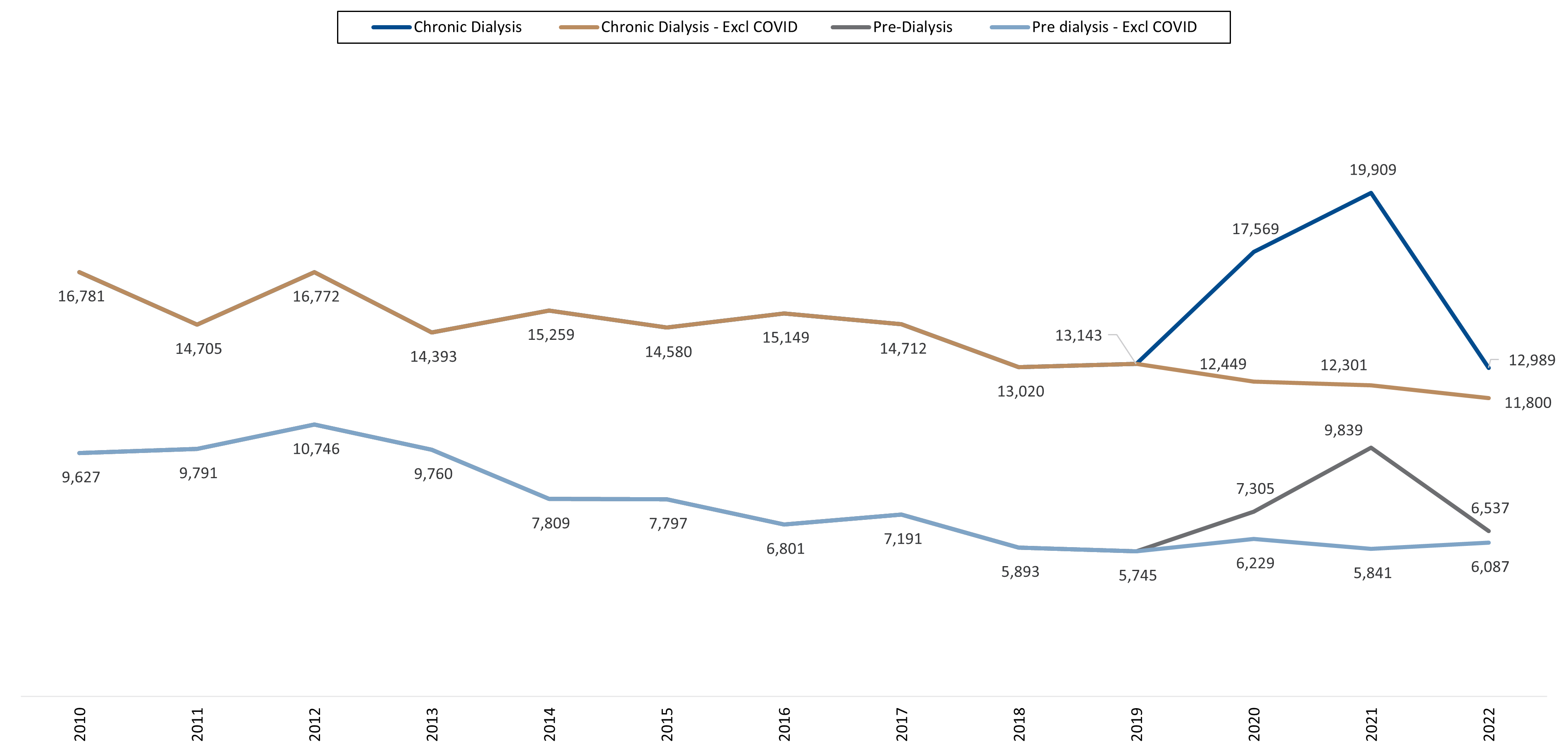
Figure 19: Age and sex standardised mortality rates for members living with CKD in the pre-dialysis versus the chronic dialysis population over time.
Possible contributors to decreased mortality rates
A major likely contributor to reduced mortality rates in the CKD population has been a reduction in cardiac related deaths.
Comparing underlying causes of death in Scheme members living with CKD in 2012 (starting reference point), 2019 (latest pre-COVID reference point) and 2022 (our most recent reference point), shows that the proportion of deaths due to cardiovascular conditions decreased from 55.7% in 2012 to 25.9% in 2022 (Table 1).
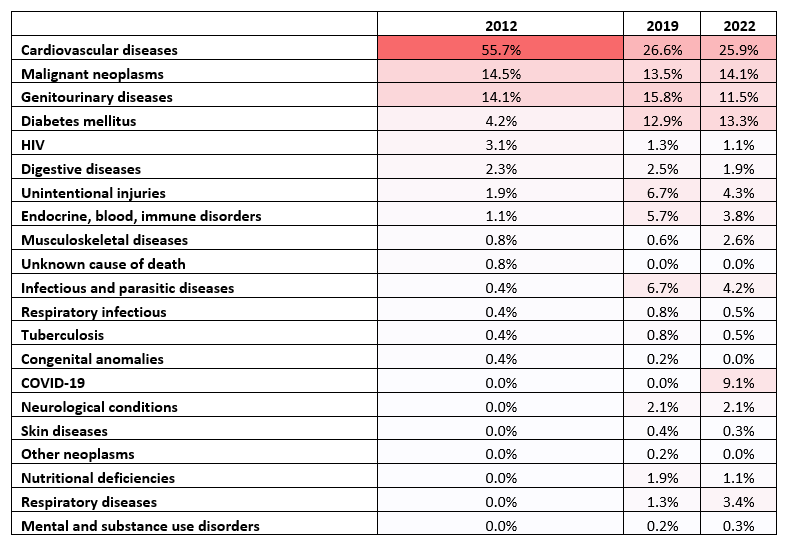
Table 1: Underlying causes of death among DHMS members living with CKD in 2012, 2019 and 2022, represented as a proportion of total deaths in the CKD population.
Statins are a group of medicines which lower levels of low-density lipoprotein cholesterol, in the blood (high levels of which raise one's risk of heart disease).
- Many studies 17, 18, 19 show that statin use reduces mortality rates in those who have cardiovascular disease as well as other chronic diseases.
- Furthermore, a meta-analysis20 of 11 randomized controlled trials revealed that statin use decreases mortality rates in people who have CKD.
There has been a steady increase in number and proportion of Scheme members who have CKD using statins over the years. Comparing claims in 2010 and 2022, there has been a 33% increase in the proportion of members claiming for statins (Figure 21). This increased statin use may be one contributor to decreased mortality rates seen in the CKD member population, and particularly due to the linked decline in deaths related to cardiovascular disease.
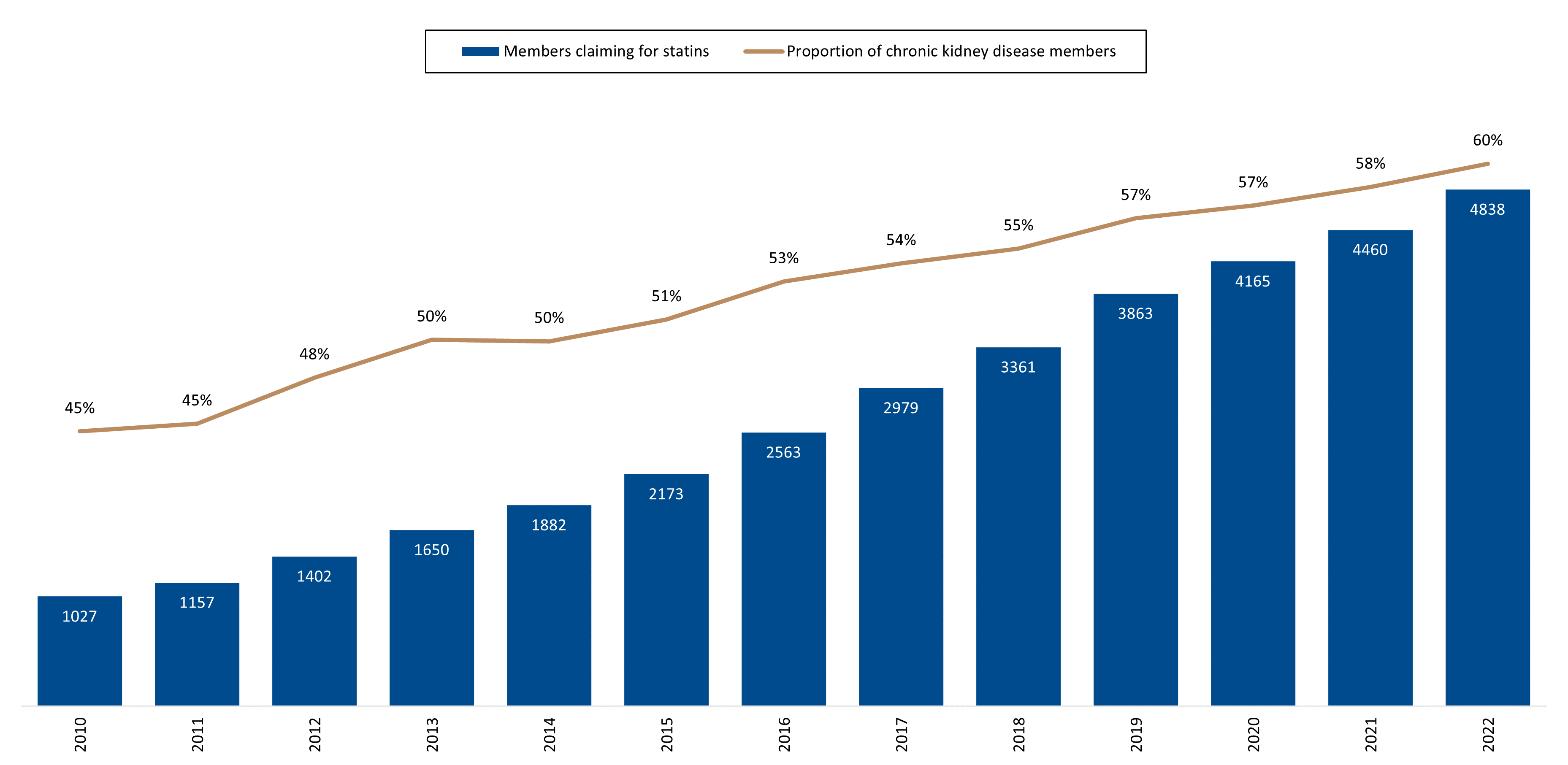
Figure 21: Number and proportion of members who have CKD, claiming for statins between 2010 and 2022.
Another possible contributor to the reduced mortality rates recorded amongst members with CKD may be the maturation of the linked healthcare provider market over the years.
The number of dialysis facilities used by Scheme members increased 4.7-fold between 2010 and 2022 from 28 providers in 2010 to 131 in 2022. (This figure doesn't reflect all of the dialysis centres operating in South Africa - 278 in 2020, of which 249 were in the private sector21). Furthermore, there has been a 1.5-fold growth in the number of nephrologists in private practice in South Africa between 2010 and 2022.
Conclusions
Highlights from our data set:
General:
The number of DHMS members who have CKD has more than quadrupled over time - from 1,747 members in 2008 to 8,113 members in 2022, with a 4.6-fold increase in incidence and a 3.25-fold increase in the prevalence of CKD. We have also seen a 7.6-fold increase in our pre-dialysis member population and 4-fold increase in our dialysis population over the time frame.
Scheme members living with CKD in 2022 were 59 years old on average, compared to 36 for the average (not living with CKD) DHMS member. Most members (58%) were male. Most members were treated in Gauteng followed by Kwa-Zulu Natal (20.2%) and the Western Cape (19.7%).
The number of people in the DHMS kidney transplant population has remained relatively stable over the years due to long waiting periods for organ transplants.
Disease stage:
In 2022, the majority of members were in a pre-dialysis population (48%), and chronic dialysis (40%) population. In 2022, the majority of pre-dialysis group members had moderate or severe kidney damage (stage 3 and 4). Only 16% of members in the pre-dialysis group had mild kidney disease. So, most members were very close to Stage 5 and progressing to kidney failure and needing dialysis, indicative of growing disease complexity and treatment costs.
Cost implications of CKD
As Scheme members who have CKD increase year-on-year, so too do related healthcare costs. This cohort makes up only 0.2% of total DHMS members yet contribute 4.1% of total Scheme costs in 2022 (R2.4 billion in 2022 compared to R316 million in 2008).
In 2022, the cost of treating a Scheme member who required renal dialysis was 29.0 times higher than costs claimed by an average DHMS member.
When it comes to hospital admissions, in 2022, the most admissions were in the chronic dialysis population where, 2,444 members (75%) were admitted at least once, and 1,732 members (53%) multiple times. Across all three cohorts the average number of admissions, for those who had multiple admissions, was between 3.2 and 3.9 in 2022, showing the degree to which these Scheme members require repeat hospital-level care. Frequent admissions are costly to the Scheme but also come at significant cost to Scheme members' quality of life, as they imply recurrent illness, and come with a heightened risk of exposure to hospital-acquired infections. Members also experience the stress of being away from home and loved ones, with disruption to their lives in general.
Furthermore, those members who require dialysis spend a significant portion of their time traveling to and from dialysis centres. Dialysis only ends when members have a successful kidney transplant, but (as discussed in our introduction) the waiting list for donor organs increases year-on-year22, 23 in South Africa.
Risk factors for CKD and comorbid conditions
CKD is often preceded by other chronic conditions. Only 205 (3%) of our total 8,113 members who have CKD in 2022 had no other chronic conditions. At the same time, 23% of DHMS members who were registered for CKD (1,832 people) were also registered for more than five additional chronic conditions. The most common associated comorbidities were essential hypertension with hypercholesterolaemia (in 12% of members) followed by hypertension alone (11%) and then a combination of essential hypertension with hypercholesterolaemia and type 2 diabetes (9%).
Vitality status
The proportion of members who live with CKD and who were Vitality members had, from 2008 to 2022, decreased from 53% to 32% of members. Among Vitality members in 2022, members of our pre-dialysis and transplant groups (18% and 17% respectively) were on higher Vitality statuses (Silver, Gold, or Diamond status) than people in the chronic dialysis group, suggesting that the latter populations are more able to live healthier and more active lifestyles than those on chronic dialysis.
Life expectancy and mortality rates
It is important that the onset of kidney disease is identified as early as possible, to improve patient and cost outcomes24. Compared to those diagnosed at an advanced disease stage, people who catch the onset of risk factors for CKD as early as possible are in a better position to manage their disease and delay their progression to end stage renal failure.
Our age profiling data suggests life expectancy among members with CKD in general (across all three of our cohorts) has increased from 60 - 64 in 2008, to 70 - 74 in 2022.
So, mortality rates for members living with CKD have decreased over time. Yet, deaths among these members were still 5.3 -fold higher than for the average DHMS member in 2022 (7.8 times higher for those on chronic dialysis). Also, people living with CKD die younger than the average DHMS member - in 2022, 73.9% of members who died were under 75 years old versus 58.9% of average DHMS members who die before the age of 75.
In 2022, deaths among members living with CKD resulted in an average of 15 years of life lost per person. The average number of years of life lost to CKD is not much lower than average years of life lost due to some cancers.
- Another of our recent analyses showed that breast cancer resulted in 20.4 years of life lost per person, certain lymphatic and haematopoietic cancers in 19.7 years of life lost per person and cancer of the oropharynx in 18.8 years of life lost per person. Like cancer, CKD is of growing global concern in terms of years of life lost. Collectively, the results of this analysis emphasise the importance of regular preventive screening checks to detect the risk factors such a hypertension and diabetes of CKD, or the early onset of the disease (especially where members have the risk factor conditions described).
On the positive side, Scheme members living with CKD have experienced a reduction of 34% in age and sex standardised mortality from 2010 to 2022 (achieved steadily except for the COVID-19 pandemic period - 2020 and 2021).
The are many possible contributors to this decreased mortality rate. These include the increased use of statin medicine (reflected in member claims data) which is associated with a reduction in cardiovascular disease in particular and other chronic conditions related to CKD; the maturing and expansion of the renal provider market for better quality of and access to care; and also, the support offered through managed care programmes.
DHMS offers tailored care programmes for members with certain chronic conditions. The Scheme's Kidney Care and Cardio Care programmes are designed to make it easier for members who live with kidney and heart disease respectively, to manage their conditions. The programmes provide access to relevant benefits, value-based contracts with providers, as well as management of risk factors through the support of a multidisciplinary care team.
The Kidney Care programme promotes quality of care for members on chronic dialysis only. The programme's measurement and reporting systems also identify areas of concern that are shared with a member's care team for intervention. There has been significant improvement in the quality of care accessed by members on chronic dialysis since the inception of the Kidney Care programme in 2008:
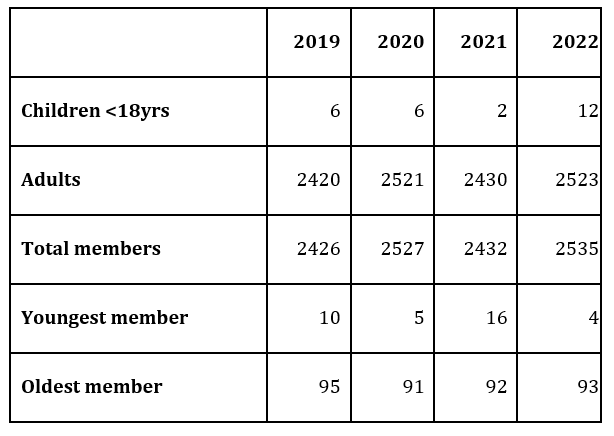
- Number of members (adults and children) on the Kidney Care programme in recent years.
In 2022, 32% of Scheme members who have CKD and who were enrolled on the Cardio Care programme subsequently also enrolled on the Kidney Care Programme (compared to only 1% in 2015), showing that in these members, renal failure (needing dialysis) was detected.
This also shows how for members who have cardiovascular disease, being on the Cardio Care programme may contribute to earlier identification of renal failure. These managed care programmes are key monitoring patient health, as CKD often has no obvious symptoms (often called a 'silent' disease) until the disease is already established or advanced to the point of serious health complications.
ACKNOWLEDGEMENTS
We would like to thank Discovery's Kidney Care team (in particular, paediatric nephrologist Prof. Errol Gottlich who heads up DHMS Kidney Care programme) for their contributions to and support of this analysis.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes. Please also look out for our related analysis of solid organ transplantation trends within the DHMS member base over time (2009-2019).
- "Epidemiology of chronic kidney disease: an update 2022" 18 Mar. 2022, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)60687-X/fulltext
- "Chronic kidney disease: global dimension and perspectives", 31 May 2018, thelancet.com/journals/lancet/article/PIIS0140-6736(13)60687-X/fulltext
- "Chronic Kidney Disease Diagnosis and Management. A Review" 1 Oct. 2019, https://jamanetwork.com/journals/jama/article-abstract/2752067
- "Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories", 16 Oct. 2018, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31694-5/fulltext
- "Kidney health for everyone everywhere - from prevention to detection and equitable access to care", 9 Mar. 2020, https://www.scielo.br/j/bjmbr/a/v3TMFdj83pz6Bz4hpSgwgNw/?lang=en#
- "Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis", 6 Jul. 2016, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0158765
- "Cost-effectiveness of hemodialysis and peritoneal dialysis: A national cohort study with 14 years follow-up and matched for comorbidities and propensity score", 27 Jul. 2016, https://www.nature.com/articles/srep30266
- "Widely-used kidney function tests underestimate scale of kidney disease in Africa", 13 Jul. 2022, https://www.wits.ac.za/news/latest-news/research-news/2022/2022-07/widely-used-kidney-function-tests-underestimate-scale-of-kidney-disease-in-africa-.html
- "Chronic Kidney Disease in the United States, 2023", 30 May 2023, https://www.cdc.gov/kidneydisease/publications-resources/CKD-national-facts.html
- "Overview - Dialysis", 29 Sept. 2021, https://www.nhs.uk/conditions/dialysis/
- "WAITING LIST STATISTICS", 2022, https://odf.org.za/statistics/
- "Organ transplantation during the COVID-19 pandemic - impact on deceased organ donor referrals and consent rates in the Western Cape, South Africa", Mar. 2022, chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/http://www.scielo.org.za/pdf/sajsurg/v60n1/10.pdf
- "The Waiting List - The Need", https://www.coursera.org/lecture/organ-donation/the-waiting-list-the-need-d1sLf
- "Stages of kidney disease", 26 Oct. 2022, https://www.kidneyfund.org/all-about-kidneys/stages-kidney-disease
- "Chronic kidney disease (CKD)", 8 Aug. 2023, https://www.kidneyfund.org/all-about-kidneys/chronic-kidney-disease-ckd
- "How Vitality Works", 2023, https://www.discovery.co.za/vitality/how-vitality-works
- "Effect of Statins on All-Cause Mortality in Adults: A Systematic Review and Meta-Analysis of Propensity Score-Matched Studies", 1 Aug. 2022, https://www.mdpi.com/2077-0383/11/19/5643
- "2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS)", 1 Jan. 2020, https://academic.oup.com/eurheartj/article/41/1/111/5556353?login=false
- "2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines", 10 Sep. 2019, https://www.sciencedirect.com/science/article/pii/S073510971933877X?via%3Dihub
- "Statins decrease all-cause mortality only in CKD patients not requiring dialysis therapy-A meta-analysis of 11 randomized controlled trials involving 21,295 participants", Jun. 2013, https://www.sciencedirect.com/science/article/abs/pii/S104366181300056X?via%3Dihub
- "Global Dialysis Perspective: South Africa", Dec. 2020, https://journals.lww.com/kidney360/Fulltext/2020/12000/Global_Dialysis_Perspective__South_Africa.14.aspx
- "Organ donation and transplantation in South Africa - an update", 2013, http://cmej.org.za/index.php/cmej/article/view/2764/3004
- "Long waiting list to receive organs in SA", 16 Aug. 2022, https://www.sanews.gov.za/south-africa/long-waiting-list-receive-organs-sa
- "Assessing the impact of screening, early identification and intervention programmes for chronic kidney disease: protocol for a scoping review", 16 Dec 2021, https://bmjopen.bmj.com/content/11/12/e053857
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only the data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.