Part 3 of 3: Thirteen year longitudinal analysis of mental health condition trends among Discovery Health Medical Scheme members, focusing on condition severity and support

"This is the concluding article of our three part series highlighting key mental health condition trends among Discovery Health Medical Scheme (DHMS)" members showing trends in the severity of symptoms in the depression population, as well as the support available to members who are at risk or who have been diagnosed with the condition. It is encouraging to observe that members taking part in these programmes have shown improvements in their PHQ 9 scores and reduced severity of their symptoms.
Authors
Discovery Health Intelligence Team members Katherine Tregoning (Actuary), Claudia Pastellides (Actuary), Cassi Rubin (Head: Mental Health Risk), Lara Wayburne (Chief Health Intelligence Actuary)
In part one of this series, we looked at the growth in prevalence of members registered or claiming for mental health conditions, the most common mental health conditions, and the correlation between living with a chronic health condition and a mental health condition. Part two examined the demographic trends among DHMS members with mental health conditions and the role played by age, sex and family circumstances.
These insights revealed that depression is the leading driver of the notable rise in mental health conditions over the last 13 years. In this article, we analyse the trends in the severity of symptoms in the depression population, as well as the support available to members who are at risk or who have been diagnosed with the condition.
Overview
Discovery Health Medical Scheme has been using the PHQ‑9 questionnaire, a standard tool for assessing the severity of depression symptoms, to monitor depression among its members. We've used the data to inform our mental health programmes. Since 2020, the number of members completing this assessment has increased significantly, along with the proportion of moderate to severe assessments. Younger members tend to report more severe symptoms, and women are more likely to complete the assessment. There has also been a rise in claims related to self‑harm, especially among young people and women, reinforcing the need for targeted support.
In response, we launched the Mental Health Care Programme in 2020 and the Depression Risk Management Programme in 2025. These initiatives offer coaching, lifestyle support and digital therapy, and have shown positive results. We've seen improvements in the PHQ‑9 scores of members who joined the programmes, compared to those who did not. Our findings support the value of proactive healthcare in improving mental wellbeing.
Analysing depression severity
The Patient Health Questionnaire 9 (PHQ‑9) is a validated scale used for screening, monitoring and measuring the severity of depression. All Discovery Health Medical Scheme (DHMS) members can complete a PHQ‑9 as part of a mental wellbeing assessment in the Discovery Health app , on the Discovery website or with their treating healthcare professional.
The questions in the PHQ‑9 assessment cover topics ranging from feelings of depression, lack of pleasure in doing things, appetite, self‑harm, concentration and sleep. Each question has a score ranging from 0 to 3, where 3 is the most severe response. Table 1 shows how the PHQ‑9 assessment scores are interpreted, with a score between 20 and 27 indicating severe symptoms of depression.
|
Total score |
Severity of depression symptom |
|
1-4 |
Minimal |
|
5-9 |
Mild |
|
10-14 |
Moderate |
|
15-19 |
Moderately severe |
|
20-27 |
Severe |
Table 1: Interpreting the PHQ‑9 assessment scores
Since data collection began in 2020, the number of Scheme members who complete a PHQ‑9 assessment has grown each year. In 2024, 351,000 members completed 463,000 PHQ‑9 assessments, compared to the 118,000 members who completed 133,000 PHQ‑9 assessments in 2020 (Figure 1).
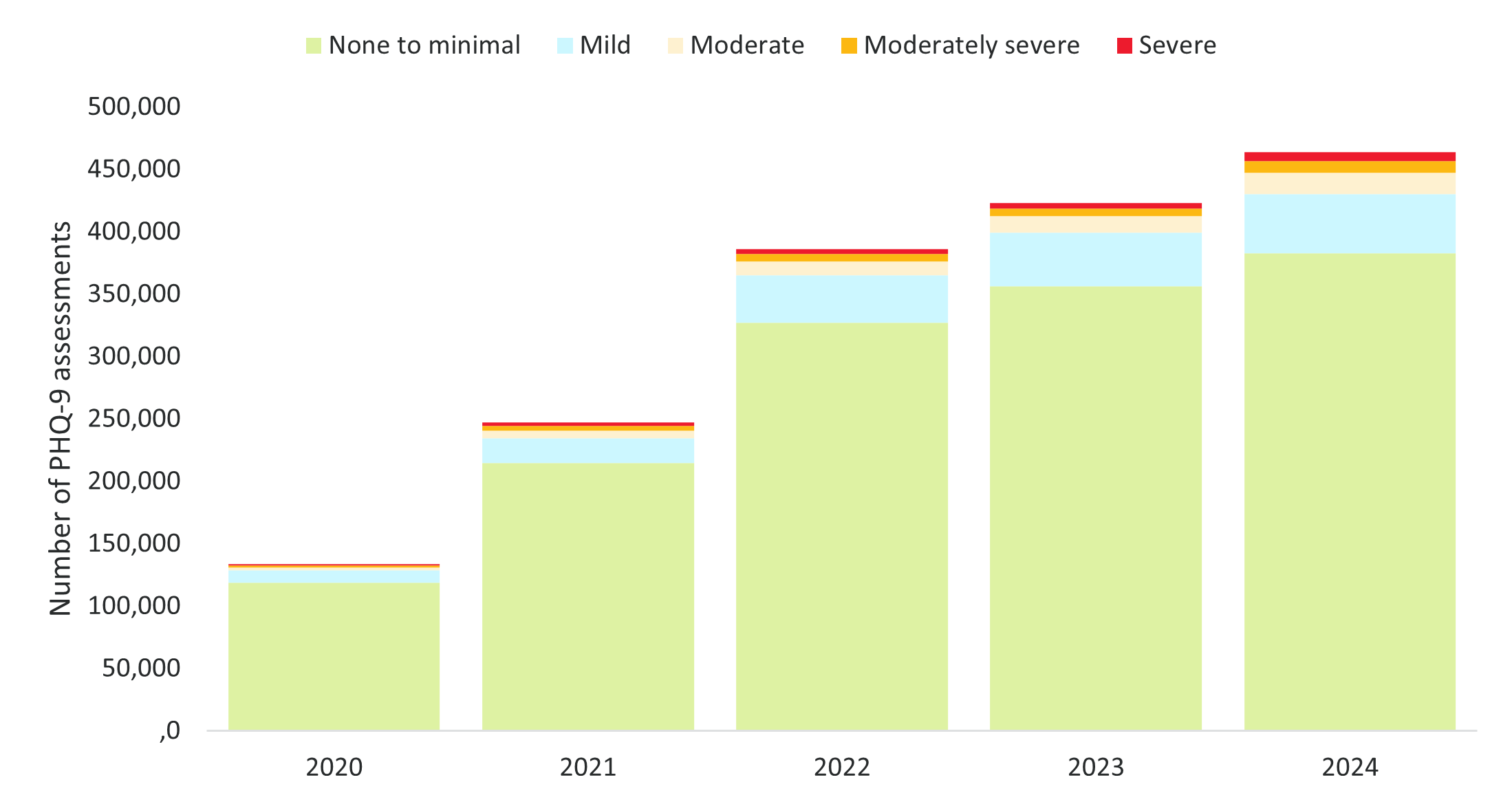
Figure 1: Number of PHQ‑9 assessments recorded for DHMS members
Figure 2 shows completed PHQ‑9 assessments with depression symptoms ranging from mild to severe between 2020 and 2024. The proportion of PHQ‑9 assessments showing moderate to severe symptoms (a PHQ‑9 score between 10 and 27) increased from 39% in 2020 to 41% in 2024. Conversely, the proportion of assessments showing mild symptoms (a PHQ‑9 score between 5 and 9) reduced from 61% in 2020 to 59% in 2024. This trend shows an increasing proportion of DHMS members with more severe depression symptoms.
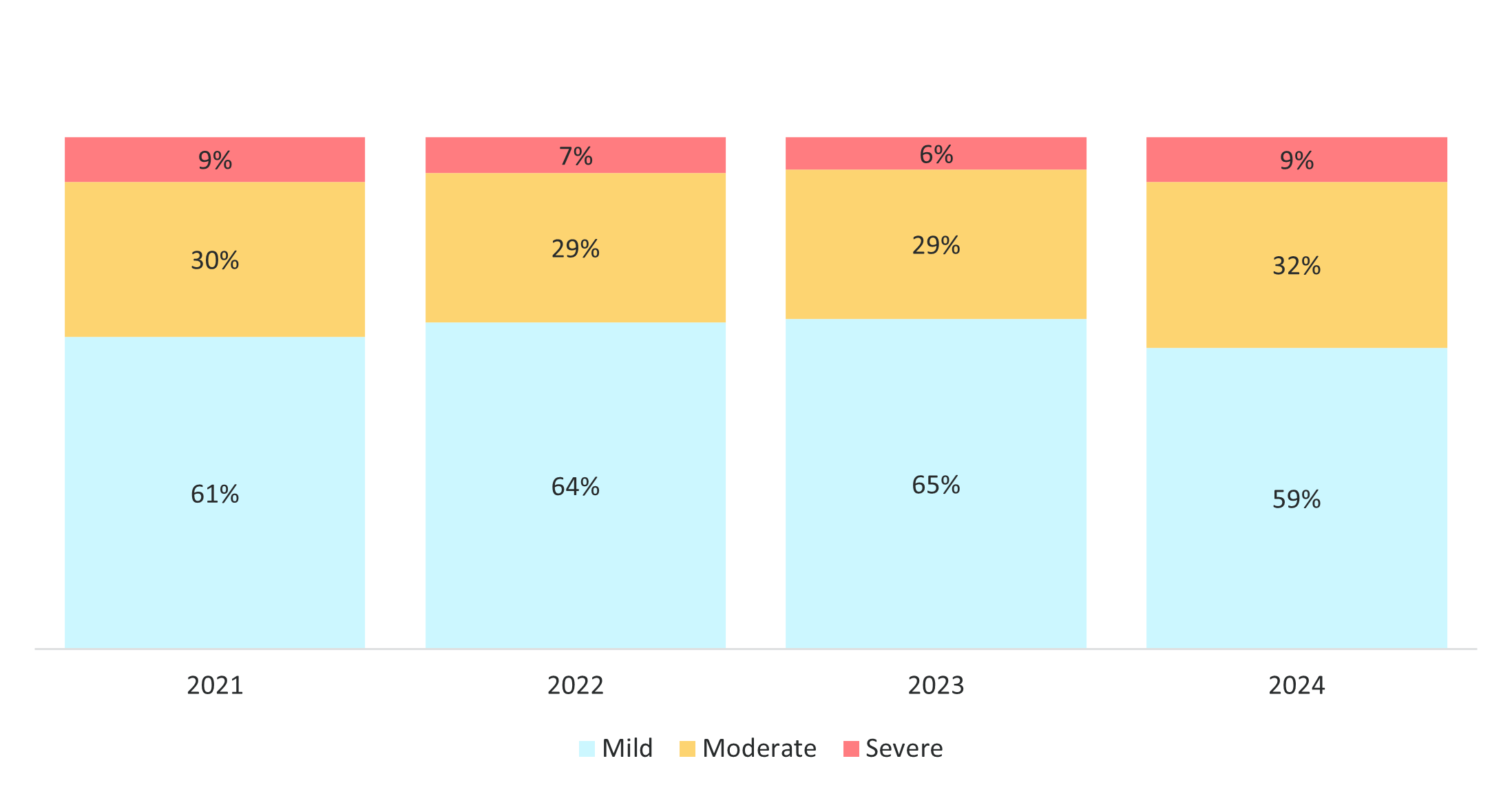
Figure 2: Proportion of PHQ‑9 assessments with mild, moderate or severe symptoms of depression
Of those members who completed a PHQ‑9 assessment, 6% were registered or claiming for depression at the time of their assessment. Of the members whose PHQ‑9 showed severe symptoms of depression, 42% were already registered for depression at the time of the assessment (Figure 3).
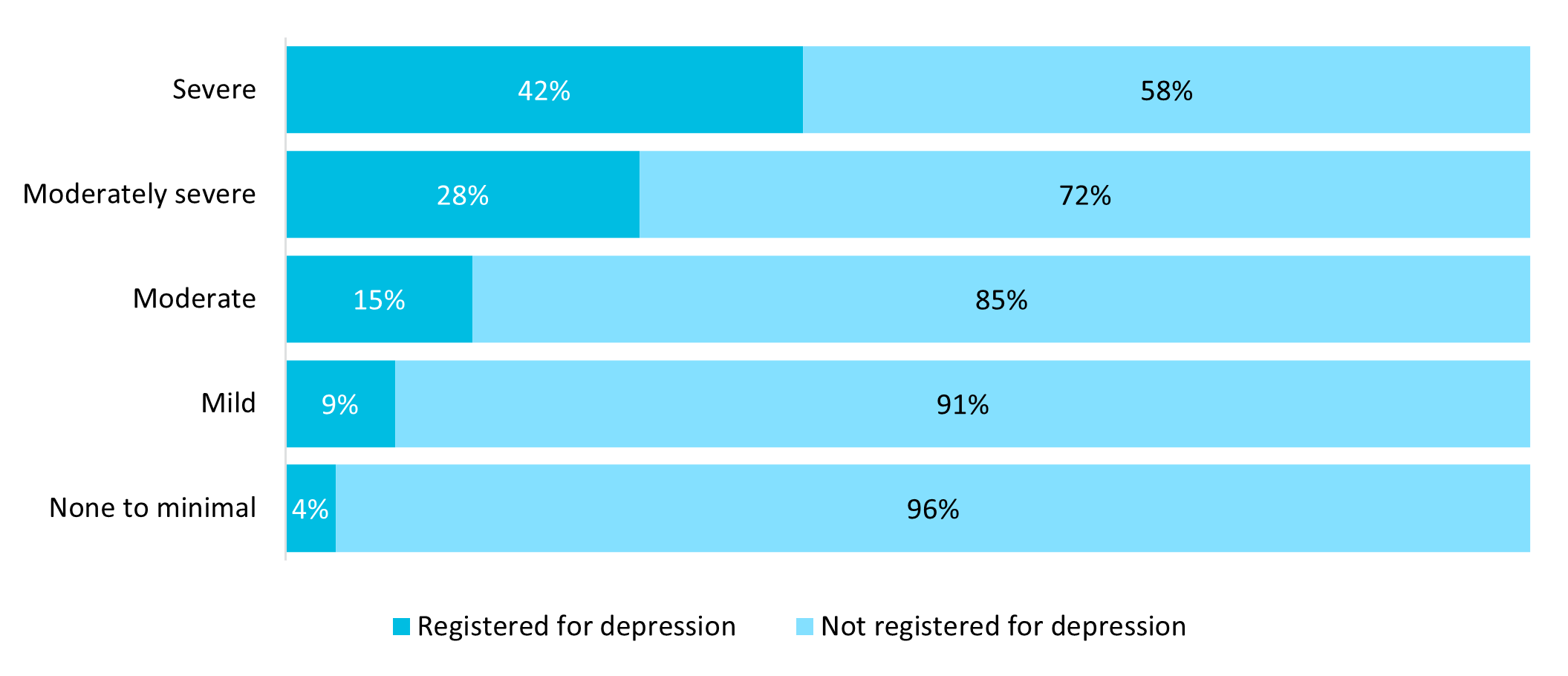
Figure 3: Proportion of members completing a PHQ‑9 questionnaire by depression registration status in 2024
Although most members who completed a PHQ‑9 assessment were female (56%), the number was lower than the 62% of females who had claimed or registered for a mental health condition in 2024. This may suggest a gap between continuous screening of symptom severity and registration for a mental health condition. Discovery Health Medical Scheme encourages members who are registered for or who are at risk of depression to regularly complete a PHQ‑9 assessment. We present the results of the assessments to the Scheme members and their treating mental healthcare professionals to help manage their conditions.
The average age of those who completed a PHQ‑9 was 42. Members who showed moderate to severe symptoms of depression on the PHQ‑9 were, on average, five years younger than those who showed none to minimal signs of depression. It's clear that when responding to mental healthcare needs, we must consider the differences in the age profile of members with depression symptoms.
Self-harm
It's also clear that mental health severity is worsening among DHMS members when we look at claims for self‑harm or self‑poisoning. Figure 4 shows that, after the COVID‑19 pandemic, there has been an increase in claims with an ICD‑10 code associated with intentional self‑harming or self‑poisoning actions.1
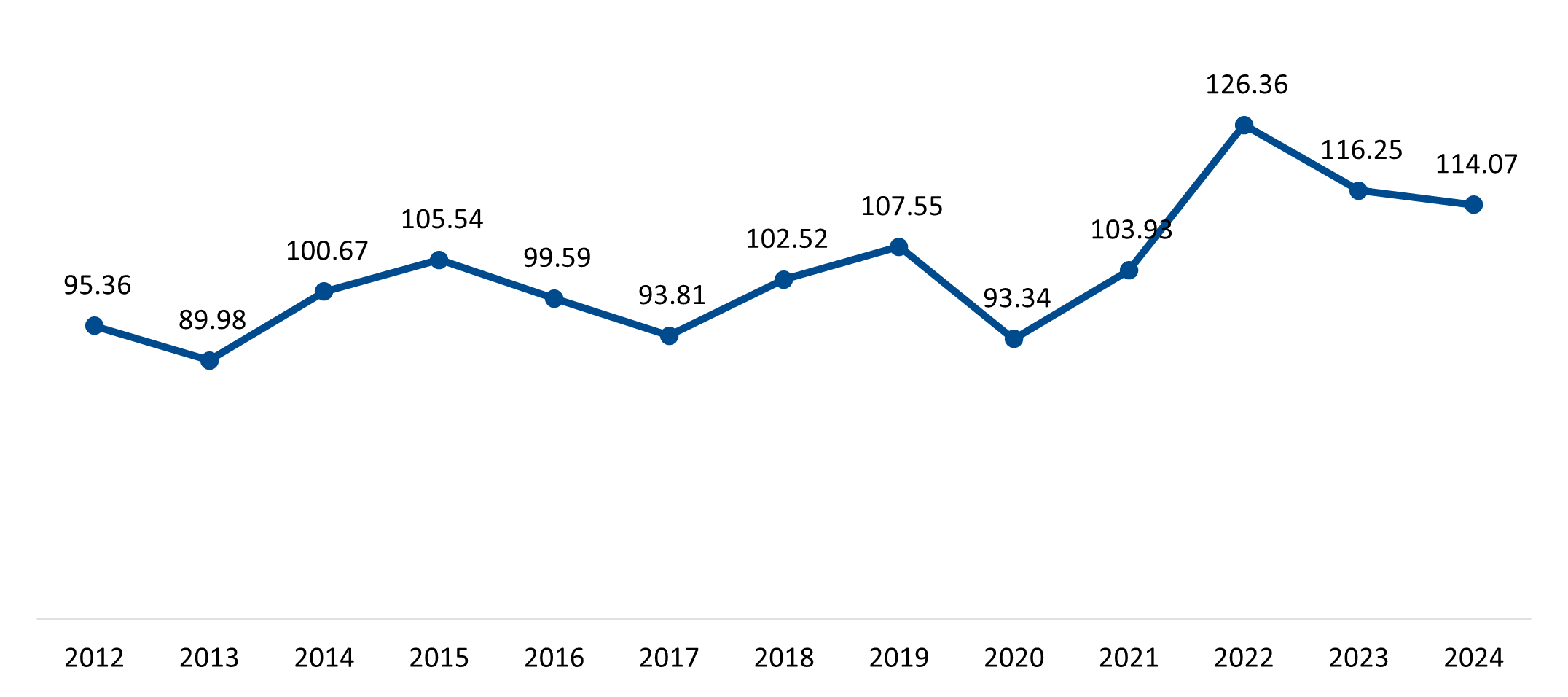
Figure 4: Rate of claims among DHMS members for an ICD‑10 code associated with self‑harm per 100,000 distinct lives
The data suggests that suicide or self‑harm claiming rates were 66% higher among female members than male members (140.6 for females vs 84.7 for males in 2024, as shown in Figure 5). This trend has been consistent over time and also aligns with international surveys which show that females have higher rates of suicidal behaviour or attempts.
1 WHO ICD-10 codes X60 to X84 billed as the primary or secondary diagnosis in a claim.
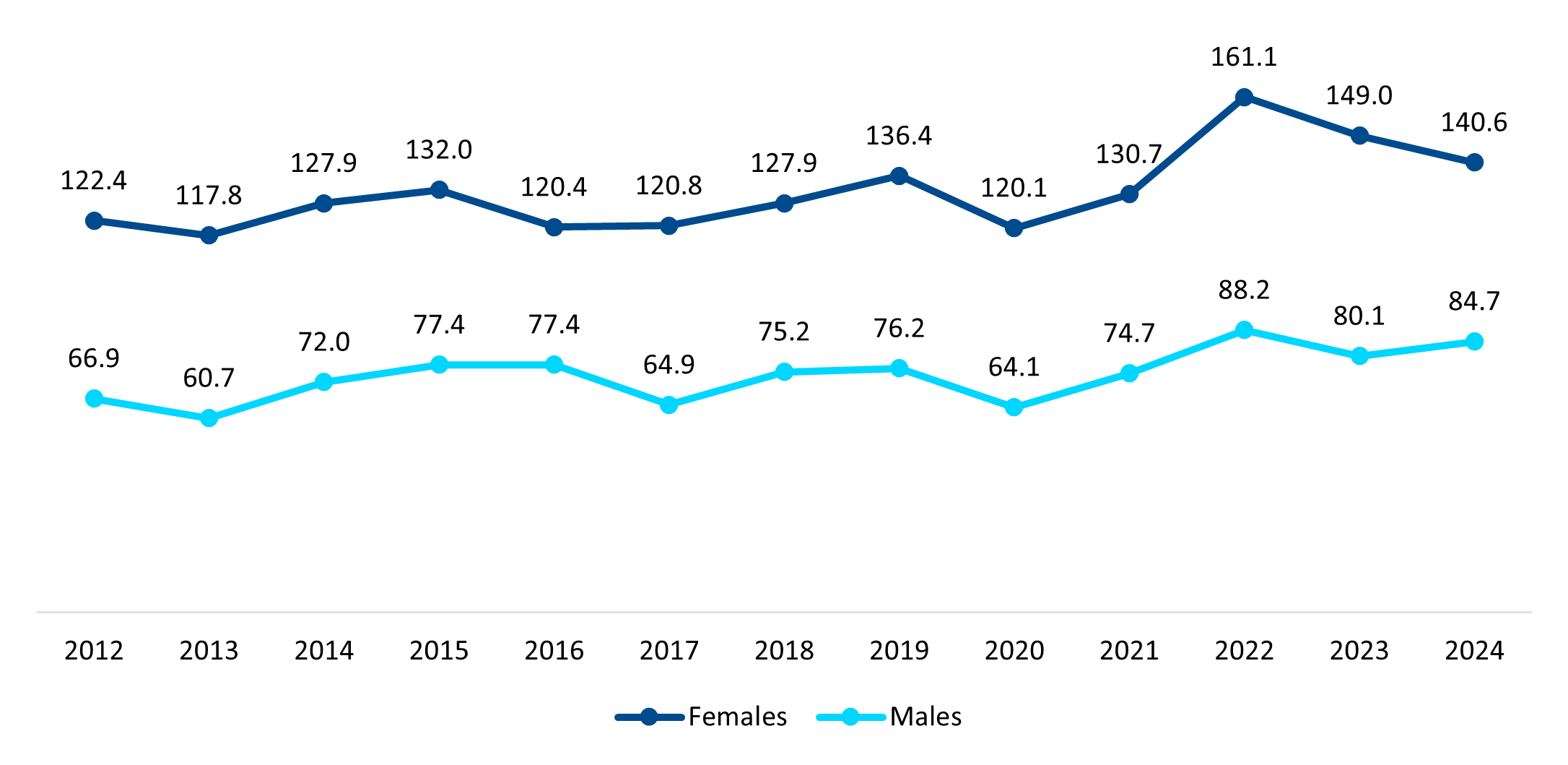
Figure 5: Rate of claims among DHMS members for an ICD‑10 code associated with self‑harm per 100,000 distinct lives by gender
DHMS members under the age of 24 showed the largest increase in claims linked to self‑harm between 2020 and 2024 at 32% (from 85.62 lives per 100,000 in 2020 to 112.62 lives per 100,000 in 2024), compared to an 18% increase in claimants over the age of 24 (from 97.08 lives per 100,000 in 2020 to 114.72 lives per 100,000 in 2024) (Figure 6). This reinforces the need to focus on interventions tailored for young members.
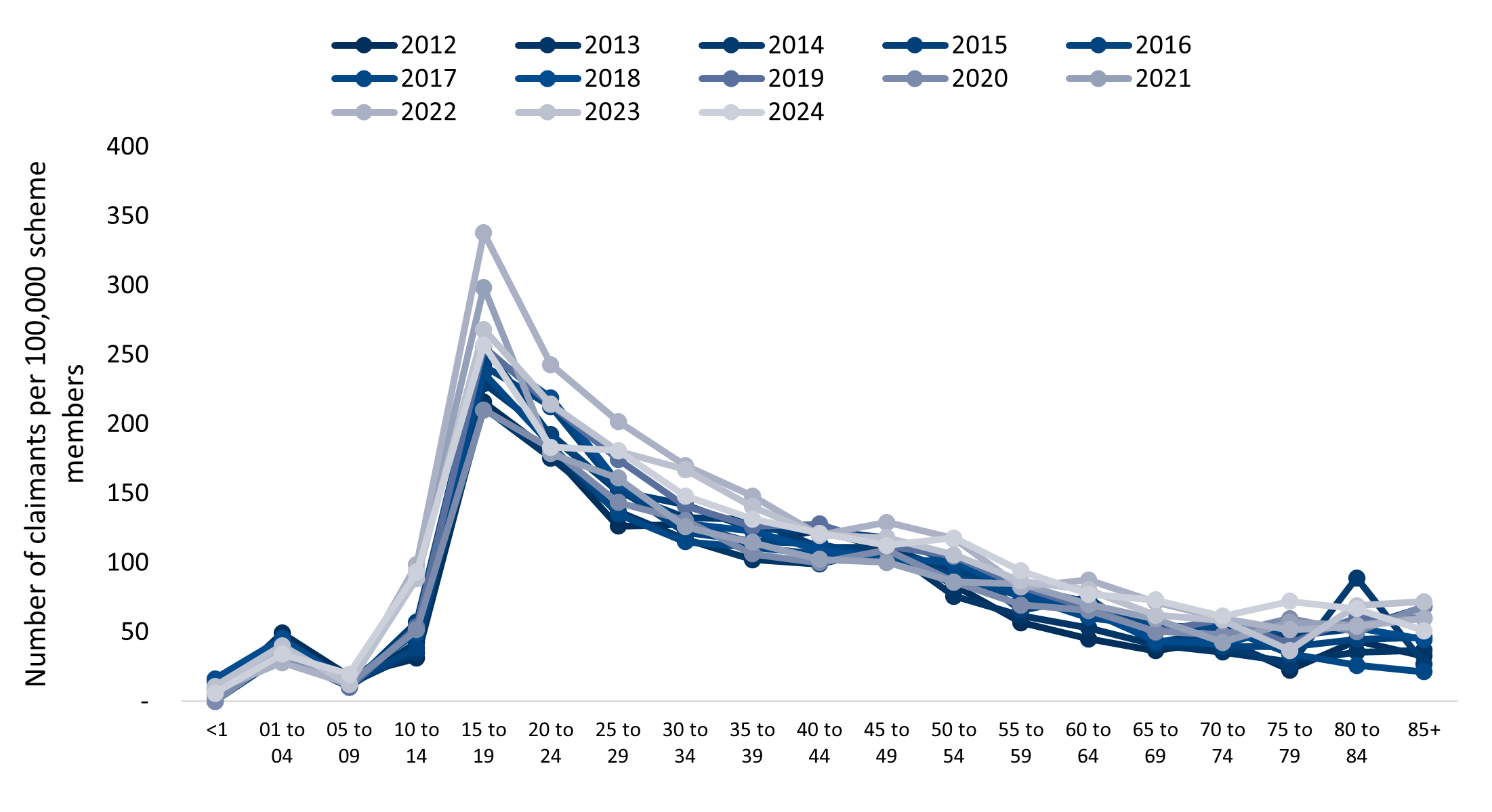
Figure 6: Number of DHMS members claiming for an ICD‑10 code associated with intentional suicide or self‑harm per 100,000 distinct lives by age
Discovery Health Medical Scheme's mental health response
Mental Health Care Programme
To respond to the increase in mental health condition prevalence and to focus on out‑of‑hospital patient care, DHMS launched the Mental Health Care Programme in 2020. This is a six‑month disease‑management programme that gives members who have been diagnosed with depression extra benefits so they can manage their condition. Members complete a PHQ‑9 assessment when they join, to make sure they meet the criteria. Once on the programme, they will have:
- All their Prescribed Minimum Benefits2
- Access to one internet‑based cognitive behavioural therapy course
- Up to three consultations with the enrolling Premier Plus GP
- Group or individual psychotherapy sessions
- Antidepressant medicine.
The members' PHQ‑9 scores have been analysed. Their scores were recorded either on the day they joined the programme or in the six months beforehand. These scores were then compared to their scores after they completed the programme. It was found that 62% improved their PHQ‑9 score, 26% remained in the same band and 13% moved to a band with more severe symptoms. Of those who completed two PHQ‑9 tests, before and after they joined, the proportion of members in the 'None to minimal' and 'Mild' bands increased, whereas the proportion of members with moderate to severe depression decreased (Figure 7). This shows that the severity of depression symptoms reduced after members completed the Mental Health Care Programme.
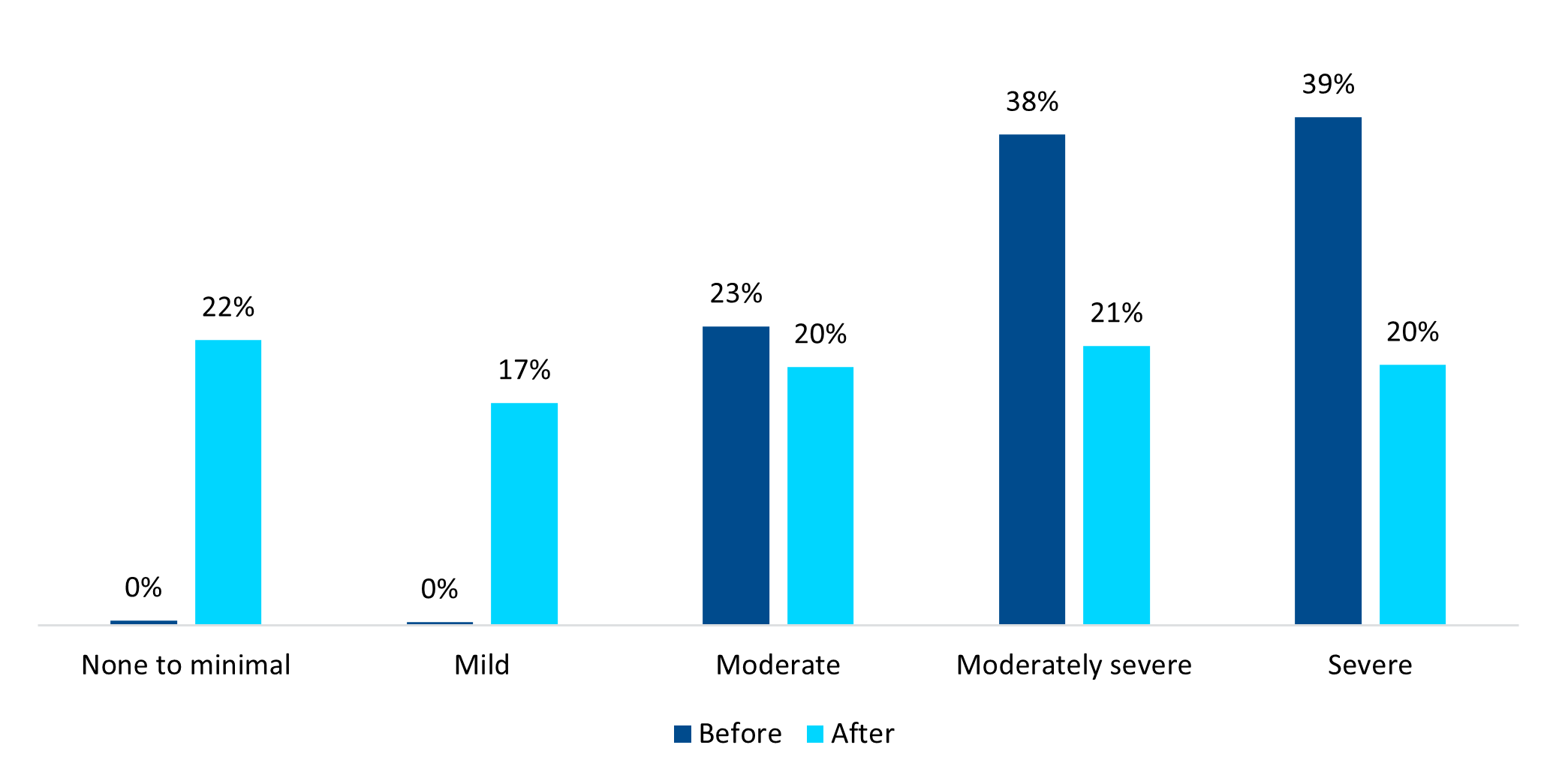
Figure 7: The PHQ‑9 score results for members who joined the Mental Health Care Programme, comparing results from the day they joined (or before) to results after they completed the programme (those who completed two or more tests, at least six months apart)
In comparison, Figure 8 shows that members who did not join the Mental Health Care Programme and who completed multiple PHQ‑9 assessments stayed in the same band after each assessment. This shows the clinical improvement in the outcomes of members who joined the Mental Health Care Programme, compared to those who did not.
2 DHMS members living with depression can apply for the out-of-hospital diagnosis and treatment set of the Prescribed Minimum Benefits basket of care for depression. This means they can have 15 out-of-hospital consultations or 21 days of in-hospital psychiatric treatment.
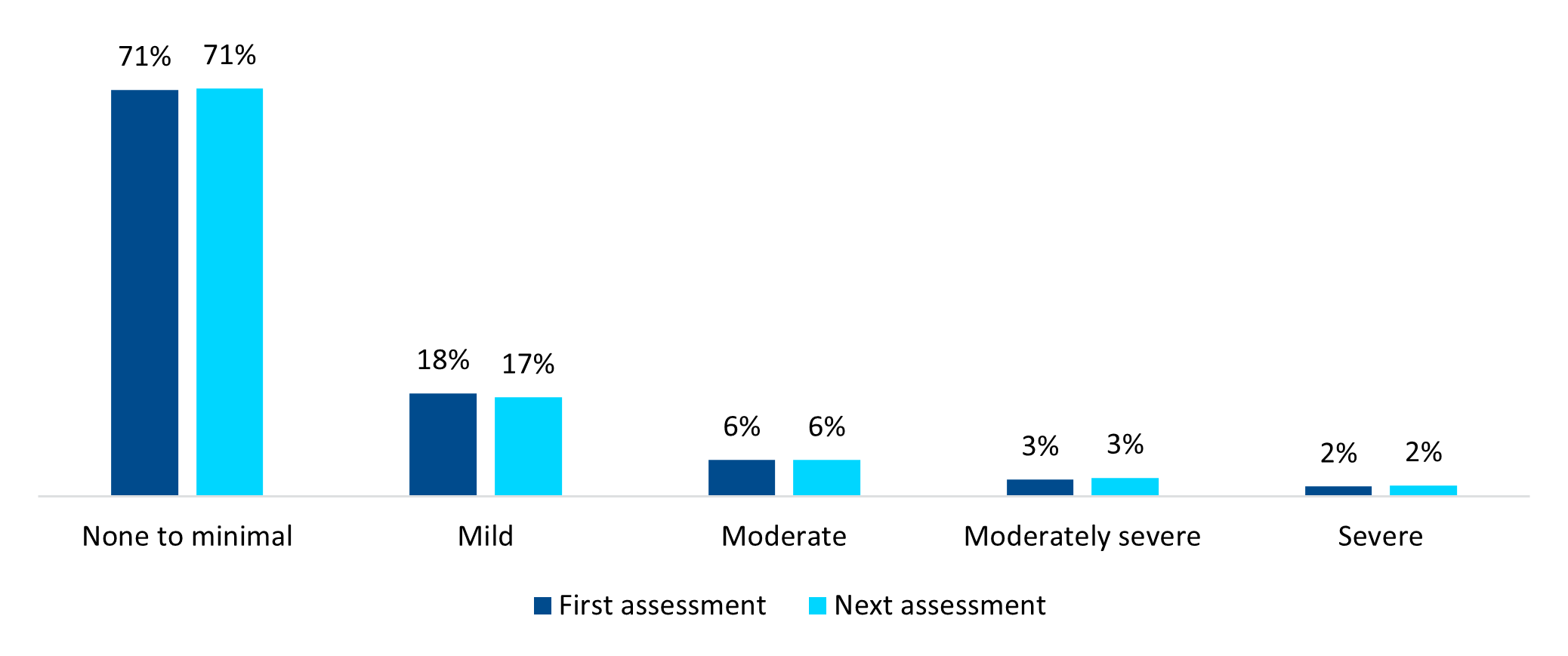
Figure 8: Distribution of PHQ‑9 score results of DHMS members who qualified for but did not join the Mental Health Care Programme (those who completed two or more tests, at least six months apart)
Digital Therapeutics
Digital Therapeutics (DTx) are a new class of evidence‑based therapeutic interventions delivered online and recommended by a healthcare professional. The Discovery Health digital mental healthcare solution (delivered in partnership with Silvercloud® by Amwell® and registered with the South African Health Products Regulatory Authority) gives DHMS members access to the first funded internet‑based cognitive behavioural therapy (ICBT) benefit in South Africa. This digital course is funded from any benefit where psychotherapy is covered, depending on benefit approval and availability.
In DHMS members who took up this benefit and completed a PHQ‑9 assessment before and after the course, we have seen an improvement in PHQ‑9 scores after finishing the ICBT. Before the programme started, 56% of members had moderately severe to severe self‑reported depression symptoms. This is compared to only 35% of members after finishing the course (Figure 9). This digital solution offers cost‑effective, clinically validated and accessible mental healthcare.
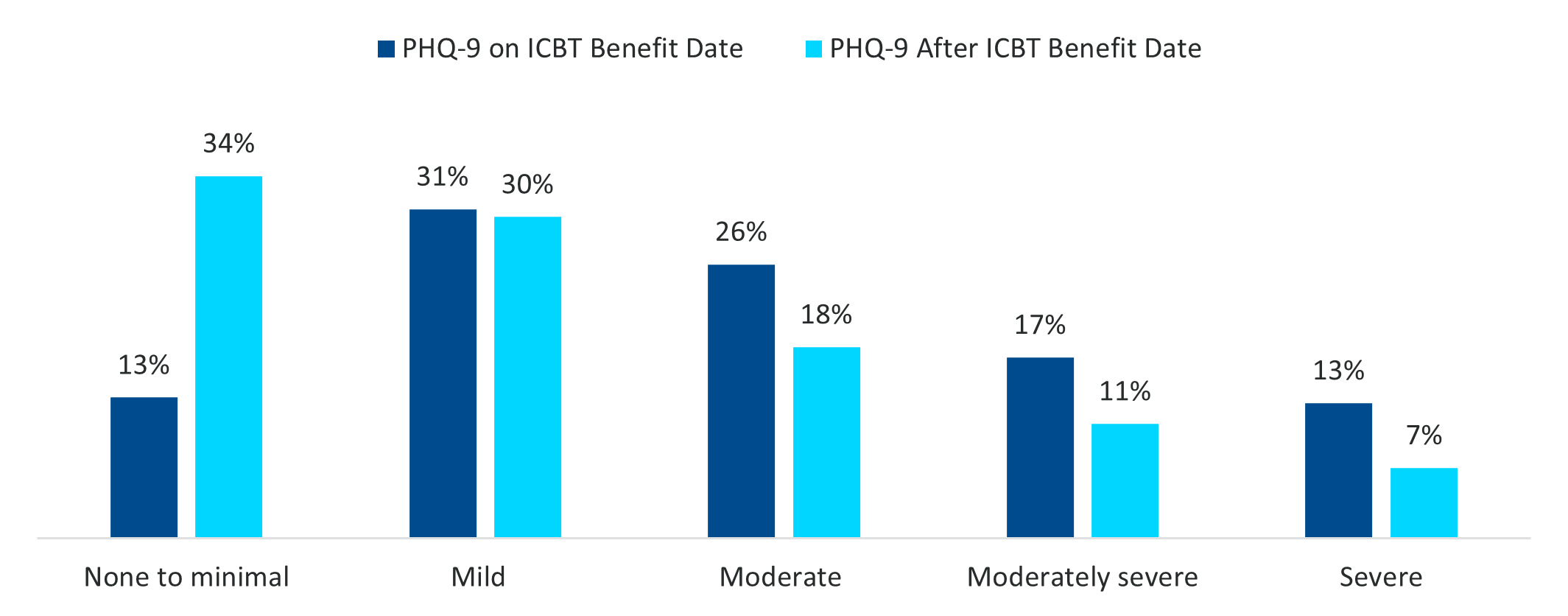
Figure 9: Distribution of PHQ‑9 score results of DHMS members in 2024 before and after completing an ICBT course, Digital Therapeutics (for those who completed both PHQ‑9 assessments)
Depression Risk Management Programme
In 2025, to enhance proactive care in the mental health space, with a focus on early identification and early intervention, DHMS launched the Depression Risk Management Programme. This is a six‑month programme, founded in neuroscience principles, to support mental wellbeing, help reduce symptom severity and lower the risk of depression.
As part of the programme, members have:
- Access to interventions which focus on sleep, physical activity and nutrition
- Consultations with mental healthcare professionals
- Regular engagement with a qualified mental health coach
- Access to digital mental health tools and ICBT where appropriate.
Qualifying members are proactively identified for this programme based on the results either of their mental wellbeing assessment or of a machine‑learning algorithm designed to dynamically identify depression risk.
Conclusion
We have seen an increase in members screening for depression symptoms by completing a PHQ‑9 as part of their mental wellbeing assessments. The data points to a concerning trend of rising severity in depression symptoms, based on ‑reported PHQ‑9 scores and an increase in self‑harm claims. Regular depression screening is still an important tool for monitoring health conditions. It should be encouraged for those who are at risk or already diagnosed.
Discovery Health Medical Scheme is committed to being proactive and responsive, given the growing prevalence and severity of mental health conditions. Identifying depression risk early is a key focus, and the Depression Risk Management Programme offers members a unique opportunity to get preventive care. The introduction of a comprehensive disease management programme for mental health, along with internet‑based cognitive behavioural therapy (ICBT), has shown promising results. Members taking part in these programmes have shown improvements in their PHQ‑9 scores and reduced severity of their symptoms.
These outcomes reinforce the value of targeted mental health support in improving member wellbeing and addressing the challenges of living with a mental health condition.
Interested in knowing more or reporting on these findings?
Please contact us on MEDIA_RELATIONS_TEAM@discovery.co.za to request any updated data available since publication and to obtain any further context required.
Did you find this post interesting?
Please visit our Discovery Health Insights Hub for a range of analyses and insights shared by our Discovery Health Intelligence Team over the past three and a half years and spanning a variety of health-related themes. All of our COVID-related analyses are posted under our "COVID-19 Insights" pillar.
All information shared on this page is based on perspectives gained from analysing data acquired by Discovery Ltd and its various affiliate entities (Discovery). The analysis, which is conducted by Discovery's actuarial and data science team, aims to encourage industry dialogue. Publications containing our analyses are shared for educational and informational purposes only. Each publication reflects only these data available for analysis at the time of publication. It does not, unless otherwise indicated, constitute peer-reviewed, published scientific research, and hence should not be interpreted as such or used as a basis for altering treatment decisions. While every effort has been made to ensure the accuracy of the content conveyed, we cannot be held liable or responsible for any actions or decisions taken based on the information shared in this article.